An ongoing dialogue on HIV/AIDS, infectious diseases,
March 29th, 2014
Opening Day ID Link-o-Rama
 Several ID/HIV tidbits to keep you entertained until Sunday night’s opening “day” — for baseball that is.
Several ID/HIV tidbits to keep you entertained until Sunday night’s opening “day” — for baseball that is.
(I hear there’s some sort of basketball tournament going on as well.)
Away we go!
- Female-to-female sexual transmission of HIV is extremely uncommon — though one such case was diagnosed at our hospital over 20 years ago — but this most recent report from Texas is probably the strongest case report to date, with both convincing behavioral and phylogenetic evidence of the transmission. Note that the infected partner had stopped HIV treatment in 2010, and had an HIV RNA of 82,000.
- Thoughtful and interesting piece in the New York Times by noted health-care economist Uwe E. Reinhardt about the controversy over the price of sofosbuvir. Good primer on cost-effectiveness as well. The challenge here is that sofosbuvir is both an incredibly expensive drug and an incredible advance on what we had previously. Quandary indeed.
- We ID doctors do love ceftriaxone — almost as much as we love doxycycline — and at least anecdotally, have been pushing this envelope of this third generation cephalosporin by using it more and more for Staph aureus infections. This report of high rates of ceftriaxone resistance among MSSA isolates might give us pause, however. Important caveat: no link to clinical outcomes in ceftriaxone-treated patients.
- Taking acetaminophen with phenylephrine — a common combination “cold remedy” — can significantly raise phenylephrine levels, potentially to dangerous levels. One of the great ironies in your drug store is the vast array of cold medicines for sale — when basically none of them works at all. Because if one did work, don’t you think that would be the one we’d all use?
- Speaking of colds, I’d bet one of the most common questions primary care providers (and ID doctors) get is, “Is it safe to exercise when I have a cold?” Thoughtful response here on the Mayo Clinic site, which I will instantly adopt.
- Some of my friends were surprised when I didn’t comment on this latest flurry of news about the dangers of cat bites. Hey, stuff like this is ho-hum to us ID docs, we know already that cat bites are bad — but cat-to-human transmission of tuberculosis? Now that’s news! Importantly, this was M. bovis, which responds nicely to standard TB treatment. So add Mycobacterium bovis to toxoplasmosis, Bartonella spp (cat scratch disease), Pasteurella multocida … here, kitty kitty!
- So the “Five Second Rule” for food dropped on the floor is real: “Time is a significant factor in the transfer of bacteria from a floor surface to a piece of food.” Extraordinary! Either that, or these British researchers have way too much time on their hands. Note that carpet is safer from a microbe perspective if fluffier. For a paranoid’s view of the whole issue, plus a scientist in an oh-so natty outfit, watch this.
- Want to make your head spin? Read the methods section in this study on the use of xenodiagnosis for Lyme disease. It can be tough going at times (“Ticks were crushed and tested by PCR and injection of the lysate subcutaneously into an SCID mouse and/or by isothermal amplification followed by PCR and electrospray ionization mass spectroscopy, IA/PCR/ESI-MS,” egad), so this commentary is a big help — especially with this statement: “…detection of borrelial DNA by xenodiagnosis is not tantamount to detection of viable spirochetes.” Agree.
Back to baseball. Here’s the best story from Spring Training, the stray dog (Hank) who wandered into the Brewers’ training facility. Sure beats some guy with a mustache sliding into a mug of beer:
March 12th, 2014
Really Rapid Review — CROI 2014, Boston
 Despite the winter that would never end, intrepid HIV/ID researchers and clinicians arrived in Boston for this year’s Conference on Retroviruses and Opportunistic Infections –or more accurately, Conference on Retroviruses and Flaviviridae (little ID joke there) — which just finished last week. Not that it was easy — a winter storm roared eastward as the conference got started, leading to cancellation of dozens of flights headed this way from the Mid-Atlantic states. This was followed by many numb fingers and toes from our unseasonably frosty weather — it was 9 degrees F one morning, a balmy 12 degrees the next.
Despite the winter that would never end, intrepid HIV/ID researchers and clinicians arrived in Boston for this year’s Conference on Retroviruses and Opportunistic Infections –or more accurately, Conference on Retroviruses and Flaviviridae (little ID joke there) — which just finished last week. Not that it was easy — a winter storm roared eastward as the conference got started, leading to cancellation of dozens of flights headed this way from the Mid-Atlantic states. This was followed by many numb fingers and toes from our unseasonably frosty weather — it was 9 degrees F one morning, a balmy 12 degrees the next.
As usual, CROI was densely packed with scientific presentations and posters; some could argue that the content of one CROI includes as much information as the remainder of the HIV conferences put together. Certainly it feels that way sometimes, especially when there are synchronous “can’t miss” presentations — just try to be in two places simultaneously, especially when one of the slide session rooms is full. Check out the conference site for web casts and, eventually, many of the posters.
(Can’t directly link the abstracts yet — I put the abstract numbers in brackets after each citation — but you can get the full program here.)
Organized roughly (very roughly) by clinical trials, cure research, complications, epidemiology, and miscellaneous interesting studies, here is a Really Rapid Review™ of CROI 2014, brought to you in Technicolor by …oh, let’s get on with it already, and be sure to read to the very end for the top HIV study of the year, as well as a terrific video clip:
- Success with an NRTI-sparing regimen? Could it be? In the NEAT study, a fully powered randomized clinical trial, darunavir/r plus raltegravir was noninferior to darunavir/r plus TDF/FTC. But — and there are several buts — there was again quite poor performance of the DRV/r plus RAL in those with high viral load/low CD4 (around one-third failed), and more resistance on failure. Plus, aside from some renal markers, was it better in any way? Not really. Can’t seeing using this regimen much based solely on this trial [84LB].
- When combined with TDF/FTC, raltegravir was significantly better than both darunavir/r and (especially) atazanavir/r, with the relatively poor result of the atazanavir/r arm driving by lots of discontinuations for jaundice [85]. Why so high in this study? A theory: Give people the option to switch and stay in the study, and they’ll take it. Note that virologic outcomes were the same. Lipids, bone outcomes also better with raltegravir [779LB, 746].
- In a phase II dose-finding study, the investigational NNRTI MK-1439 — hereafter to be known as doravirine — was potent and well tolerated [92LB]. Guess the big question for its development is how much we need a new NNRTI — none of our current options is perfect, true, but they are pretty good. And what will be the three-letter abbreviation of doravirine? “DRV” is already taken!
- In the LATTE study — how can you not love that name? — a two-drug maintenance treatment of the v-e-r-y long half-life integrase inhibitor 744 and rilpivirine, both given orally, worked quite well [91LB]. There was only one case of treatment failure with resistance, occurring in a study subject who was on a heavily calorie-restricted diet — not good for rilpivirine! These results set up the potential for a future combination strategy using injectable long-acting preparations of each drug — once-monthly injections, anyone? And will that be a niche intervention or transformative antiretroviral strategy? You decide.
- For patients starting TDF/FTC/EFV, giving vitamin D and calcium significantly reduced the degree of bone mineral loss with ART initiation [133]. But is it enough to warrant doing it for everyone? And would it work if EFV were not the drug, which induces vitamin D metabolism? Somehow I’m just so biased against supplements, my gut feeling is to hold off for now in making this standard practice.
March 10th, 2014
CROI Is Over — and a Baby Once Again Takes Center Stage
One of our fellows asked me this AM when I was posting a RRR (Really Rapid Review™) of CROI 2014, and my response was to clear my throat, make some vague excuses, and curse the respiratory viruses that seem as perpetual as the cold weather this year.
It’s in the works, promise — but in the meantime, did you see the New York Times Editorial Page yesterday? Under the title, “Great Hope for Babies With H.I.V.”, the editorial cites the case reported at CROI last week of a second baby possibly “cured” of HIV after starting ART soon after birth.
Why do I use the word possibly and put the word “cured” in quotes? From the Times:
The baby, now 9 months old, has no signs of virus in her blood that can be detected by the most highly sophisticated tests. She cannot be considered “cured” or even “in remission” because she is still taking the drugs.
Yes, that bolding is mine.
Isn’t it incredible how much attention this case has received, despite that oh-so-important fact?
Prediction: One day we will be treating all babies born to HIV-infected mothers who are not receiving ART with combination therapy, at least initially.
But until we have more than a few of these anecdotes — especially those that have stopped treatment and not experienced viral rebound — let’s calm down already.
February 27th, 2014
CROI 2015 Dates Announced — And Warning, It’s Still Winter in Boston
From the CROI website:
We are pleased to announce that CROI 2015 has been scheduled!
Location: Seattle, WA, USA
Dates: Monday, February 23 to Thursday, February 26, 2015
Details and schedules: Will be posted in early summer 2014
Love their exclamation point. Yahoo indeed! Kudos to the conference organizers for getting the dates out early this year.
Meanwhile, for those of you planning to attend next week’s conference in Boston, I bring you this bit of chilling news. On the plus side, the whole convention center is interconnected with most of the conference hotels, or just a short walk away.
 But for some travel anxiety, especially for those planning on arriving Monday, here’s a good place to start.
But for some travel anxiety, especially for those planning on arriving Monday, here’s a good place to start.
Hey, since we can’t change the weather, might as well complain about it.
February 23rd, 2014
A Lower Dose of Efavirenz Works Just Fine — and Why This Matters
As we heard last year in Malaysia, and now published in The Lancet, 400 mg of efavirenz is just as effective as the standard 600 mg dose.
The proportion of participants with a viral load below 200 copies per mL at week 48 was 94·1% for efavirenz 400 mg and 92·2% for 600 mg (difference 1·85%, 95% CI −2·1 to 5·79). CD4 T-cell counts at week 48 were significantly higher for the 400 mg group than for the 600 mg group (mean difference 25 cells per μL, 95% CI 6—44; p=0·01).
The 400 mg dose was better tolerated, too. For the record, these data are far more convincing than prior dose-reducing strategies with other antiretrovirals (stavudine, zidovudine, ritonavir come to mind). The results of the study were no doubt outstanding.
So these results have huge implications internationally, where efavirenz-based regimens are the default first-line choice for essentially all treatment naive patients. A lower dose will make treatment cheaper, coformulations easier, the pills smaller, and the sun will shine brighter, too.
Here in the USA? As of today, these data are of limited value, and here’s why:
- As first-line therapy, efavirenz is overwhelmingly given as part of coformulated TDF/FTC/EFV (Atripla), which as you know includes 600 mg. Decreasing to 400 mg means increasing the number of pills, both because this splits up the coformulation and because EFV comes in 200 mg capsules.
- If we’re after similar efficacy and better tolerability, there are several other non-efavirenz first-line options that do the same thing, and are easy to take, too — notably TDF/FTC/rilpivirine, TDF/FTC/elvitegravir/cobicistat, and TDF/FTC or ABC/3TC + dolutegravir.
- Until a generic version of efavirenz is approved, there’s not all that much benefit from a cost perspective — though I do hear that TDF/FTC/EFV pricing has been going up.
- The 400 mg dose is not FDA approved for treatment.
So for now, I stick with my opinion about the waning of the efavirenz era — a drug which has been on an extraordinary run dating back its approval in 1998.
However, if the 400 mg dose does get FDA approved, and if there are future coformulations with EFV using this dose, and if these data are confirmed to lower toxicity while maintaining virologic efficacy, then efavirenz might make a comeback.
But it’s a long shot.
February 13th, 2014
Jeter is Retiring, and Certain ID Doctors Are Getting Old(er)
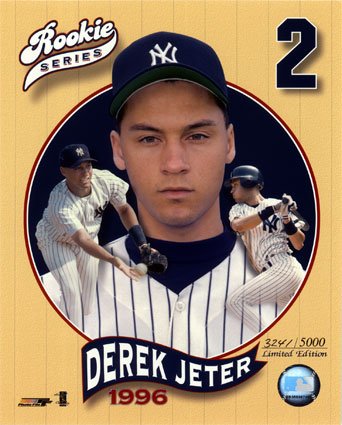 It’s safe to say that most of the perspectives on Derek Jeter’s retiring from baseball will not be written by ID doctors, so let me seize the opportunity.
It’s safe to say that most of the perspectives on Derek Jeter’s retiring from baseball will not be written by ID doctors, so let me seize the opportunity.
And since it’s always risky to dwell on players from a certain team while living in Boston — I have friends for whom a central component of their identity is Hatred for the Yankees — this will be less about Jeter’s retirement and more about how the news made me feel.
In a word — old.
You see, I was at the game when Jeter hit his first major league home run — opening day in Cleveland, April 2 1996, weather a balmy 38 degrees. That was a remarkable year on many fronts, both personal and professional, as my daughter was born, Boston experienced its snowiest winter ever, HIV became suddenly treatable (How About That!), and well, the Yankees won the World Series, in part thanks to their rookie shortstop.
So what was it like to be an ID doctor 18 years ago? Let’s take a look at the Wayback Machine, and I caution those of a certain age that this is guaranteed to make you feel downright ancient:
- You were still doing gram stains in a hospital lab that was on the patient floors.
- Aminoglycosides were a regular part of “triples” — you know, amp, gent, clinda.
- Amphotericin B had no liposomal formulation, and was co-administered with all kinds of magic potions (diphenhydramine, meperidine, hydrocortisone, pixie dust) to make it better tolerated.
- Erythromycin was used as an actual antibiotic — sometimes even intravenously.
- Ritonavir was used as an actual antiretroviral, and the dose was 600 mg twice daily (yes kids, you read that right).
- Severe C diff was extremely uncommon, and almost never happened in an outpatient.
- Community-acquired MRSA might be presented at an ID case conference given its rarity.
- There was hardly any vancomycin-resistant enterococcus — good thing, too, since there was no linezolid.
- If you wanted a quinolone to treat community-acquired pneumonia, you were out of luck — levofloxacin wasn’t approved until December 1996.
- If your patient needed indinavir, he/she needed to get it from a single mail-order pharmacy called “Statscript.”
- No echinocandins, oseltamivir, tigecycline, cefepime, daptomycin.
- Some days you spent half of your time on rounds looking for X-rays. These were actual films, viewed on a light box — or, if you were in the radiology department, on those noisy contraptions that rotated light boxes. (What did they do with those things?)
- These numbers/letters meant nothing: HLA-B*5701, HPTN 052, K65R, E138K, CCR5, CXCR4, Q80K, PrEP, TDF.
- Target vancomycin trough level: 5-10.
- Some people were actually taking ddC — which, despite the medical “information” from Dallas Buyers Club, was a pretty horrible medication.
- Best place for drug information was often the “PDR”. If you’ve never heard of it, don’t ask.
I could go on like this all day, but why not finish on a high note?
February 5th, 2014
Electronic Medical Records, Eye Contact — and Dogs
 A few thoughts on the importance of eye contact during patient care, no doubt inspired by my puppy’s first birthday, and his insistent and adoring (at least that’s how I see it) gaze:
A few thoughts on the importance of eye contact during patient care, no doubt inspired by my puppy’s first birthday, and his insistent and adoring (at least that’s how I see it) gaze:
- Long piece in the New York Review of Books — all doctors subscribe, of course — by Arnold (Bud) Relman, describing his experience as a 90-year-old who survives a fall. Riveting, moving, and typically curmudgeonly stuff from the ex-Editor-in-Chief of the New England Journal of Medicine. But this line deserves emphasis: “During the day I was visited on rounds by teams of physicians. They spent most of their time outside my room, studying and discussing the data on their mobile computers.“
- How do interns spend their time in the era of electronic medical records? Let’s look at the data — “Interns spent 12% of their time in direct patient care, 64% in indirect patient care, 15% in educational activities, and 9 % in miscellaneous activities. Computer use occupied 40% of interns’ time.“
- Or, for a more poetic description, read Abraham Verghese’s brilliant description of the “iPatient”: “On my first day as an attending physician in a new hospital, I found my house staff and students in the team room, a snug bunker filled with glowing monitors … the demands of charting in the electronic medical record (EMR), moving patients through the system, and respecting work-hour limits led residents to spend an astonishing amount of time in front of the monitor.”
- One of my colleagues in General Medicine, Jeff Linder (who parenthetically does some nice ID-related work too), found that the number one barrier to use of electronic medical records during an outpatient visit was loss of eye contact with patients — which does not surprise me a bit.
- The solution? Get a medical scribe to join you in the exam room so you can actually look at the patient while taking the history. This is the money quote from this wonderful New York Times piece: “For decades, physicians pinned their hopes on computers to help them manage the overwhelming demands of office visits. Instead, electronic health records have become a disease in need of a cure, as physicians do their best to diagnose and treat patients while continuously feeding the data-hungry computer.” FYI, after reading this piece, every single colleague of mine wants a scribe now.
- The hospital periodically receives patient surveys from these guys. The leading complaint, of course, is parking — this is Boston, after all. But in the Top Five Complaints is also something along the lines of, “That doctor seemed more interested in the computer than in me.”
- Department of Oversharing: I recently saw a doctor for an eye issue, and he was very competent and nice. He spent 90% of the visit (aside from the exam part) entering what I was telling him into his electronic medical record. The computer was situated far to his left, so he was facing away from me the entire time; I could have put on this hat, he never would have noticed.
OK, so I’m nearly done. Except to comment that we used to be able to take notes while facing our patients, and that this allowed a kind of organic eye contact that seems all but impossible in the electronic medical record era. Note that I won my 8th Grade Typing Competition (72 words/minute, thank you), so don’t blame inadequate keyboarding skills.
And since this started with a dog (dare you to click on the image above) and eye contact, I might as well say that they run rings around both cats and us electronic medical records-obsessed doctors when it comes to this skill.
Enjoy more dog magic in this nifty documentary:
January 30th, 2014
Unanswerable Questions in Infectious Diseases: Persistent MRSA Bacteremia
 Ok, here’s a favorite of adult ID specialists everywhere — a real tough one. The case goes something like this:
Ok, here’s a favorite of adult ID specialists everywhere — a real tough one. The case goes something like this:
Older person, many medical problems. Probably is on hemodialysis, with the vascular surgeons having some difficulty with access. There’s diabetes, of course, and cardiovascular disease, and oh yeah, a mechanical aortic valve that’s around 10 years old. Some toes are missing from prior surgical treatment of osteomyelitis.
Now? Fever and mental status changes have brought him/her to the hospital, and 100% of the umpteen blood cultures done since admission are positive for MRSA. They remain positive even though the MIC to vancomycin is 1.0 and the trough concentration of the drug is 18.
Since starting on vancomycin, the patient has improved somewhat, but continues to have fevers and, yes, positive blood cultures. Lots of them — it’s been days. Vancomycin MIC is checked again, and it remains unchanged. Maybe even it’s 0.5 this time. An exhaustive search for a removable focus of infection has yielded nothing — no abscess, no valvular vegetations/root abscess, no spinal osteomyelitis, clots. A cardiac surgeon has been consulted, and passes on the opportunity to replace the valve, thank you very much. The dialysis AV fistula is functioning, for now, but is not red or draining.
So the question is this:
With persistent MRSA bacteremia despite “appropriate” vancomycin therapy, should the antibiotics be changed?
Lots of options out there. Linezolid. Daptomycin. Ceftaroline (off label, of course). Combination therapy, with the idea that more should be better, naturally. You could add gentamicin (really?), or rifampin (biofilms!), or do a vancomycin/beta-lactam combination.
Let’s hear from you — vote on these options (as I said, there are lots of them this time), then comment away.
January 21st, 2014
Unanswerable Questions in Infectious Diseases: The Positive Cultures for Candida in an ICU Patient
 OK, gang. You did such a bang-up job on Question #1 that I can’t resist getting another consult.
OK, gang. You did such a bang-up job on Question #1 that I can’t resist getting another consult.
Here’s the case: Patient in intensive care, has been there for some time — at least a week, probably weeks. Perhaps he/she had surgery (especially abdominal surgery) that didn’t go well, or has severe cardiovascular disease, or multiple trauma from an MVA, or suffered a large intracerebral hemorrhage or stroke. There have been several antibiotic “courses” directed at fevers of too many origins.
Each day you see the patient, and each day there’s a fever — generally 100.5 or a bit higher. Normotensive. Nothing obvious on exam. Labs show a WBC of 11-15 — in other words, not normal but not horribly abnormal either. LFTs are fine.
All bacterial cultures are unrevealing. Several sputum cultures, however, are positive for Candida; a urine culture (from a foley catheter) is positive also. If the patient has an abdominal drain, it has a few yeast in there too. Imaging is non-specifically abnormal — some pleural effusions, but no obvious pneumonia; CT shows no abscess.
So here’s the question:
Should patients in the ICU be given systemic treatment for Candida spp. if they have positive cultures from multiple sites other than blood?
If you want to research the question, here are a couple of randomized trials here and here, concluding yay and nay, respectively.
Or just go ahead and vote, and have at it in the comments section.
January 15th, 2014
Unanswerable Questions in Infectious Diseases: The Abdominal Collection and Duration of Antibiotic Therapy
 Each time I attend on the inpatient service, the number of questions for which we just don’t have a definitive answer continues to amaze me. And here’s the most remarkable part — many of them come up all the time!
Each time I attend on the inpatient service, the number of questions for which we just don’t have a definitive answer continues to amaze me. And here’s the most remarkable part — many of them come up all the time!
In that spirit, I will post a series of these quandaries, and you, the brilliant readers, will offer your answers or, barring a definitive answer, your individual approach.
Let’s start with this one:
How long should we continue antibiotics in someone with infected abdominal collection and a percutaneous drain?
You know the situation — peritonitis from perforation, or diverticular abscess, or a surgical mishap, and now the interventional radiologists have kindly placed a drain into the infected collection. (Or, more commonly, multiple drains into the multiple collections.) The patient, once critically ill, is improving — albeit slowly — and the resident, surgical PA, and surgeon all want to know the answer to the above question.
Low grade fevers — 99.5 F or so — continue. There might be an ongoing anastomotic leak, there might not. There is no plan for more surgery. White blood cell count is down from 25K to 15K. Platelets are slowly rising.
Yes, this is a specific variant on the age-old “How long should we treat?” question. I’ve opined on this before, but now we’re getting specific. These IDSA guidelines say “4-7 days,” but that implies rapid source control, no ongoing leak, everything going smoothly.
(And these smooth-sailing cases rarely trigger an ID consult.)
So what do you do in this particular situation? Please vote and comment — especially if you don’t like any of these answers!

