An ongoing dialogue on HIV/AIDS, infectious diseases,
March 7th, 2022
How to Induce Rage in a Doctor
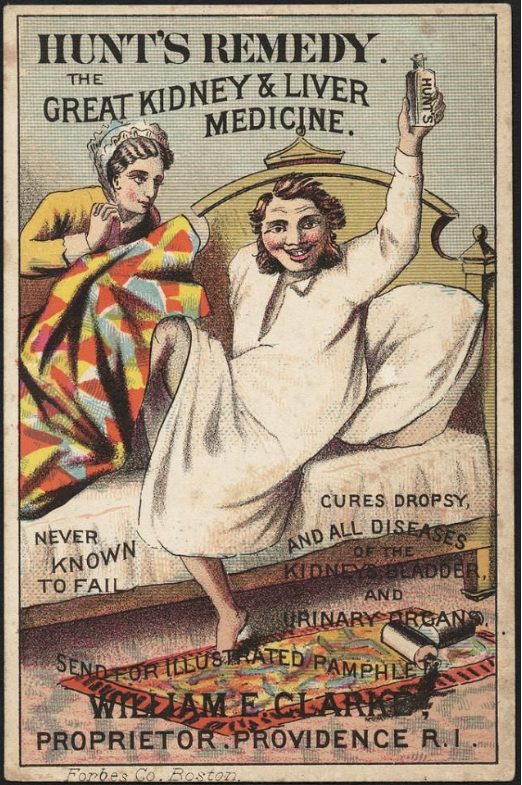
Advertisement for Hunt’s Remedy, which cured all diseases but did not require a prior authorization.
If you’re wondering how to make a doctor angry — really, really angry — read on. Because asking us to justify treatment decisions to insurance companies and their pharmacy benefit managers must rank right up there with the greatest tortures of practicing medicine in this country.
Mind you, this isn’t just about my patient, or about me — such infuriating events take place innumerable times in countless offices, hospitals, and clinics around the country every day, wasting everyone’s valuable time with no evidence whatsoever that they improve the quality of care.
Such struggles are an inevitable part of a healthcare system that values profits over people. The debates require a veritable army of staff on both sides to navigate what should often be very straightforward treatment issues.
Here’s a timeline of what happened. It’s Part 2 of the case presented a couple of weeks ago, which appeared with the patient’s permission (certain details changed).
February 6: Patient notifies me he needs a corticosteroid injection for back pain, which is contraindicated with his current HIV therapy due to a potentially serious drug interaction. We set up a video visit to discuss alternative HIV treatment options.
February 7: Televisit. I explain some treatment options, which I outline as bictegravir/TAF/FTC, dolutegravir/3TC, or doravirine plus TAF/FTC. He opts for the doravirine option based on side effects from previous treatments. Prescription sent to pharmacy.
I mention to him that doravirine sometimes requires a prior authorization. I also tell him that with his employer-provided insurance, it most likely will be fine. After all, the guy has a high-powered job in a very well known organization. He must have good coverage.
Furthermore, while HIV treatment remains quite expensive, none of the alternatives I’ve offered costs significantly more than what he’s currently receiving, and some cost less — at least based on the prices available to us.
Ha. Not so fast.
February 10: Message from patient that his pharmacy told him doravirine wasn’t covered. Needs a prior authorization.
I ask our pharmacy team, which consists of pharmacists and pharmacy techs hired for this express purpose, to help with it. They send it in, along with my office note from the televisit which justifies the reason for the treatment change.
February 14: I hear from the pharmacy team — prior authorization has been denied. Oh, and there’s this message:
Alternative Requested: PIFELTRO [doravirine] is NON-FORMULARY. MUST USE EFAVIRENZ, NEVIRAPINE, EDURANT. Call xxx-xxx-xxxx.
Well, this is a joyful Valentine’s Day present. They obviously don’t know his medical history, or much about HIV treatment. Why can I make this assumption?
- Efavirenz caused severe side effects years ago — he can’t take that.
- Nevirapine is not recommended in any treatment guidelines anymore, especially in people (like my patient) with high CD4 cell counts, as this increases the risk of severe hypersensitivity — he can’t take that.
- Edurant (rilpivirine) should not be given to people with low stomach acidity since it won’t be fully absorbed — he can’t take that.
I’ve always wondered — what if we followed these directives, and something truly terrible happened? After all, there are people who have died from nevirapine hypersensitivity, either from toxic epidermal necrolysis or fulminant liver failure or both.
Would the insurance company bear any of the blame, or legal risk? Would they care? I know the answer, sadly.
February 15: I call the phone number, which takes me to the pharmacy benefit manager. It’s the Giant-est of the Giants. How do annual revenues of more than 30 billion dollars sound? Pay for plenty of doravirine with that.
Phone tree. Then hold music. A warning about high call volume and long wait times. Then a person. Below a sampling of the dialogue.
Pharmacy Benefit Manager person #1: Hello, you’ve reached Brett. May I have the client’s member number?
Me: I don’t have it. I have his name and date of birth.
PBM person #1: OK, I’ll take that.
[pause while they look up the record]
PBM person #1: It says here the prior approval was denied. Pifeltro is non-formulary. You must use [pauses] EFAVIRENZ, NEVIRAPINE, EDURANT. [Difficulty reading the HIV drugs implies no knowledge of HIV medicine.]
Me: I know that — this is why I’m calling. But he can’t take any of those.
PBM Person #1: Do you want a clinician-to-clinician consultation?
Me: Yes. That’s why I called — this is the number we were given.
PBM Person #1: OK, let me transfer you.
[Hold music. Another warning about high call volumes and long wait times.]
PBM Person #2: Hello, you’ve reached Blake. May I have the client member #?
Me: I just gave that information to the previous person. Didn’t they pass that along to you?
PBM Person #2: Sorry, no.
Me: I have the name and date of birth, not the client #.
[Information given again.]
PBM Person #2: It says here that your prior approval was denied. You must use [pauses] EFAVIRENZ, NEVIRAPINE, EDURANT [more difficulty pronouncing the HIV drugs].
Me: That’s what the last person said to me, and I already know that. My patient can’t take any of these drugs. This is supposed to be a peer-to-peer consultation.
PBM Person #2: They sent you to the wrong number. I can forward.
[Hold music. Long hold.]
PBM Person #3: Hello, this is Bobby. May I have the patient’s name and client #?
Me: I only have the name and date of birth.
[Information given again. Third time, but who’s counting.]
PBM Person #3: I found the record. The Pifeltro was denied.
Me: Yes, Bobby, I know that, this is why I’m calling. Hoping you can help me. I’m an ID/HIV specialist in practice since 1992, and I’ve known this patient since 1996, including his full treatment history. The recommended alternatives are contraindicated — he can’t take any of them.
[Long pause.]
Me: Hello, do you need any further information?
PBM Person #3: I’m sorry, doctor, but I am not authorized to approve this drug.
Me [more than a little annoyed at this point — in fact here’s a good description of how I looked]: Why then am I speaking with you? This is the phone number I was advised to call. Are you a clinician? Do you have any knowledge of HIV treatment? Do you have access to the notes that were submitted for this claim?
PBM Person #3 [sounds like Bobby is now driving a car while speaking with me]: I’m sorry, Doctor. I am not authorized to approve this drug. If you want to appeal, or the patient wants to appeal, they will need to directly contact his insurance company with an appeal letter.
So why did all this happen? Why did Brett, Blake, and Bobby each fail to help my patient get his prescription covered?
It all starts with the relatively high cost of HIV treatment to begin with — a cost that has increased over 30% since 2012, a rate 3.5 times faster than inflation. Unlike most other industrialized countries, where government payers gather disease experts to review treatment options, then work with the pharmaceutical companies to arrive at a cost, such deliberations here are explicitly blocked and remain controversial.
With antiretroviral therapy so costly, insurance companies enlist the PBMs to negotiate what treatments get covered, what don’t, and how much they’re going to cost. It’s all done behind closed doors, in exchanges that one insider told me are “brutal.” As concisely (and accurately) stated in the opening to this recent perspective, “Prescription drug prices in the United States are opaque.”
The PBMs also sometimes direct where patients can most easily get their prescriptions filled (which may be the same companies, imagine that), and discourage dispensing of less expensive (but not negotiated) products.
If you think this clandestine process is ripe for distortion, obfuscation, and misuse of power, you’d be absolutely right. The lack of transparency means my patient and I have no way of finding out why doravirine isn’t covered — just that it isn’t.
But one thing I can state with 100% confidence — the refusal to cover my patient’s doravirine prescription has nothing whatsoever to do with improving the quality of his care, or following treatment guidelines, or really anything related to his health at all.
It was all about money. And that is sad indeed.
Hey, two more entries for the timeline:
February 25: Received information about the appeal process, and wrote the letter.
March 7: Still waiting …
(Thanks to brilliant colleagues Drs. Aaron Kesselheim and Ben Rome for reviewing this post. And to Dr. Glaukomflecken for making us laugh and cry at the same time.)


You are right, the bottom line is money (although sometimes even this logic does not hold up–adding our bewilderment). The solution is to enact laws that allow Medicare to set drug prices to a level that are comparable to those in other countries. Bernie Sanders may be wrong in many other ways, but on this one, he is spot on!
Wow! How true, how true! So many of us are exhausted by this frequent series of events! Hmmm, provider burn out from this, then add mandatory EMR documentation, and now all the COVID garbage. All this really means less and less patient care or less quality care. I 100% agree with your article. Thank you!
All this sounds exhausting.
However, a simpler solution to avoid all the HIV medication hassle is for the interventional pain physician to reduce the dose of steroid for pain injection. Steroid injections potentiate the dose of anti-retroviral medications, which can lead to anti-retroviral toxicity. The patient will likely get significant pain relief from a low dose steroid injection for his back pain, while greatly reducing risk of anti-retroviral toxicity. My patients do. Steroid injection doses are routinely higher than needed, and I reduced my injection dose years ago. Consider talking with the pain doctor.
Unfortunately, power and money are the coin of the realm. If one could hold the Insurance Company and specifically those who make such decisions liable, that might over-rule such medically inappropriate decisions. Alas, only the physician is held responsible. One would think that our legal brethren would be interested in this, after all, the target is usually the one with the deep pockets.
This is one of the major reasons why I retired from my solo PLLC practice. I was at the end of the rope.
~25 years ago I went through an analogous experience seeking approval for a newer, but FDA-approved anti-cancer drug. During what became a heated exchange, I demanded who SHE was, as I was a nationally/internationally recognized medical oncologist holding a professorship at a medical school. Just as I recognized her voice it was revealed that she was a nurse returning to the workforce, having not worked for 15+ years. She lived in our neighborhood and was the mother of my older son’s high-school classmate & best friend. She had no experience in oncology. I got nowhere in spite of a professional position and a personal friendship
Ironically ~15 years later her son died of male breast cancer after being on every appropriate FDA-approved drug, every EUA drug. etc. for which she and her husband vociferously argued.
This is not patient care. This is an investment dictatorship.
Money talks! Bulls$$$ walks! Thanks America for making Health Care profitable to Commercial Insurance!!! Your life depends on Capitalism?
Why not name the insurance company in this piece? Shaming works sometimes!
The company representative states, “I hear you but it is not approved”. My reply is, “If it is not approved, then you don’t hear me”.
I am just a gp …since 1968.
My treatment for back pain is based on the observations of mind-body approach of Dr John Sarno,MD (Professor at Rusk Rehabilitation,New York Un until late age.
Book “Healing Back Pain : the Mind Body Connection ‘(1984) and a 26 min interview on You Tube (2017) shortly before his death at 93. and ‘Healing the Mind,Healng the Pain.”
Success rate is excellent …in those who try it ,(Including myself in 1995 after 20 years of suffering
Treatment is free ,but needs a change in perception.
A recent meta analysis on 35 studies on back pain(2 on neck pain) concluded that none of the treatments proposed for back pain (AINS,Physio,Surgery etc) worked.,(In Journal Watch Gen Med 2018?)also nov 2021 on Sciatica)
Dr Allen Brett ,MD ,senior editor concluded “:That pretty well summarises our experience”)
Back pain is no 2 reason for consulting a doctor in N America.
But I agree with Dr Sax ,practicing medicine in USA is a horrible experience.
That is why I came back to Canada in 2004.Getting the medicine is so much easier.
Precisely the reason I retired a couple years earlier than planned. Diabetes supplies (including continuous glucose monitors not to mention insulin pumps) and meds (which manage glucose and decrease CV and kidney disease risk) required prior authorization either every 6 or 12 months. I controlled the urge “I am unaware of diabetes being cured.”) Same story for osteoporosis meds.
Thank you for allowing this conversation
Amen! I tried to prescribe pioglitazone for a patient on a SGLT2i/metformin combo pill, prior to considering expensive injectables sure to need a PA. Pio is a cheap generic, despite which it is a step therapy and ultimately declined because the insurance wouldn’t understand the patient is already on the required metformin. It took an hour on the phone to straighten. Turns out that GLP-1 analogs are same step and equal cost to patient, so something probably better for the patient despite usual short term cost benefit thinking.
I suggest that all physicians and patients learn about PBMs. These entities were designed to lower costs but have become a scam. There are just a few PBMs and they work off of kickbacks that they call rebates. The end result is higher drug prices and big pharmacy firm being owned to a large extent by the PBMs. The whole system is a remarkably disgusting scam.
You have just described a day in the life of a rheumatologist. The system is ludicrous. Step therapy is required based solely on deals made with drug companies behind doors. In the last year I have had multiple instances of insurance companies requiring patients who are doing well on therapies to switch their treatment since the insurance company decided not to keep the prior preferred drug on the next years formulary. Can you imagine how many more patients a week I could help if I did not spend hours daily in the fight to get patients the medications they need? This madness needs to STOP!
I feel your pain. I treat patients with sarcoidosis which has no FDA approved drugs. I have spent so many hours trying to get steroid sparing agents approved because I know in the long run it’s better for my patient. PET scans also are impossible. I think they hope you will give up with all the transfers. I think it is on purpose. I never give up. I don’t know how many years I can keep doing this though.
Denying or delaying patient care is malpractice committed by the insurance company and/or their authorized representatives. Some of these individuals are also practicing medicine outside the bounds of medical licensure. Give them some love courtesy of appropriate Counsel, and where appropriate, the medical and nursing boards of licensure. That will take the zeal from the immoral greed.
Now , that is a bizarre career. Denying care without being responsible. 30 billion $$$ profits must allow companies great legislative steerage.
I once had a patient with pulmonary blastomycosis. After a week of getting runaround about approval for itraconazole, and several hours on the phone, I learned that the health insurance contract with the patient’s employer (a hospital!!) did not cover ANY antifungal drugs for ANY reason!
After threatening to call the press and attorneys general of the states involved (where I practice, where the patient lives, and where the insurance company is based) so the insurance company can explain how they wrote a policy that does not cover life threatening infections, I received a call back that the insurance company had decided to grant an “exception” and pay for treatment of this particular fungus.
The overarching theme of the article and all of the responses to it is money is the root of all evil. I beg to differ. What is the root of money? Creative production in a free society, in this context life-saving medications, gives value to peoples lives and to the means of exchange which is money.
Capitalism is the free exchange of values in a free society. What has caused this to go awry in our country as it clearly has? The commingling of the power of money with the coercive power of government has caused what we are experiencing to happen. Massive corporate lobbying and political campaigns financed by massive corporate money has led to this outrageous corporate truculence and non-caring attitude doctors and patients are experiencing.
What is the solution? A constitutional convention to overturn the Supreme Court ruling, Citizens United vs FEC circa 2012, which labeled money as free speech which couldn’t be limited. Term limits should be included as well as a start for the ultimate answer: Complete separation of private economics and state for the same reason as the separation of church and state.
Please take some of these egregious cases to court and blow this system up. I am convinced you could convince a jury paying out of pocket is not feasible for high cost meds. Great editorial (there is a counter point in support of prior auths which is laughable in comparison). https://pubmed.ncbi.nlm.nih.gov/32584673/ or https://www.jmcp.org/doi/pdf/10.18553/jmcp.2020.26.7.822
Man, you are so right. Loved the video by the way. We need to laugh now and then between the high stress, anger and sadness affecting doctors these days!