An ongoing dialogue on HIV/AIDS, infectious diseases,
February 18th, 2022
A Return of Antiretroviral Rounds — What Regimen Would You Choose?
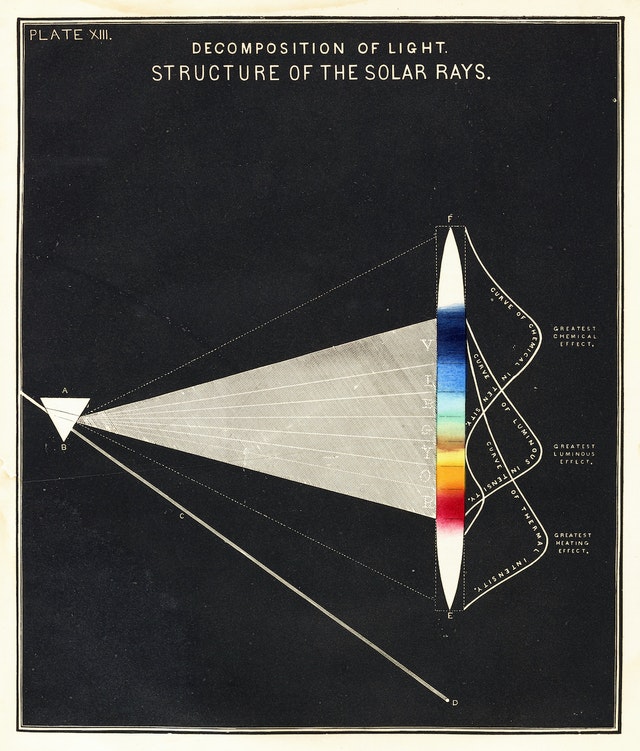
Structure of the Solar Rays, Edward Livingston Youmans, 1856.
Years ago, back in the pre- and early internet days, one of the most popular features in the newsletter Journal Watch AIDS Clinical Care was something called Antiretroviral Rounds.
We’d present a case, then have two expert discussants weigh in on what they would do. The link above is a case from ancient history — 1998! — to show how far we’ve come.
Today, in honor of Antiretroviral Rounds, and inspired by a particularly annoying interaction — ok, an infuriating interaction — with a pharmacy over an insurance issue, I bring you a reprise of this feature and ask you to select what HIV treatment you’d recommend. This week, the case; next week, what happened.
(Details shared with the patient’s permission, and slightly modified.)
This man in his 60s has had HIV likely since the early 1980s from treatment of an inherited coagulopathy. He was diagnosed shortly after testing became available in the mid-1980s.
He started treatment with zidovudine, then later added didanosine. Several years of low-level viremia but clinical and immunologic stability followed.
I met him in the mid-1990s, shortly after he moved to Boston. He works in a very demanding job, where he has a leadership position and travels a ton. He’s a workaholic even by American standards, and that’s saying something.
His one and only resistance test showed he had resistance to both zidovudine and didanosine, but preserved predicted activity of tenofovir, lamivudine, and all the drug classes he had never taken. In the early 2000s, he started tenofovir, lamivudine, and lopinavir/ritonavir. He has had virologic suppression since then.
Brief trials of switching treatment to a different drug class led to significant side effects. Efavirenz caused severe somnolence, mood alteration, and sleep disturbance; raltegravir made him feel “like I’ve aged a decade overnight.”
So fast-forward to today, and he’s on the one-pill daily treatment of darunavir-cobicistat-emtricitabine-tenofovir alafenamide. No side effects. Feeling fine.
So what’s the problem? Not surprisingly given his treatment history and age, he has some “diseases of aging.”
- Didanosine caused non-cirrhotic portal hypertension and gastropathy, a condition I’ve learned may lead to unreliable stomach acidity (that will be important for later).
- Years of HIV and tenofovir DF have resulted in osteoporosis.
- He has arthritis in multiple joints, leading an orthopedist to strongly recommended a trial of steroid injections.
Experienced HIV clinicians will hear this recommendation for injectable steroids, and get very worried. The medical literature is replete with reports of marked hypercortisolism and sometimes subsequent adrenal insufficiency from the interaction between “boosters” (this is the cobicistat in his regimen) and injectable steroids. This is the same drug interactions issue getting attention now with the ritonavir in Paxlovid, though that’s relatively easy since it’s only 5 days of treatment, with a couple of more days for the ritonavir effect to wear off.
I have seen numerous cases of this interaction over the years, sometimes with serious consequences (compression fractures, steroid myopathy, sleep disturbance, depression, hyperglycemia, intractable hypertension, fluid retention). This intra-articular treatment is erroneously thought by some not to be a “systemic” treatment, and many clinicians are unaware that cobicistat and ritonavir markedly impair the clearance of many corticosteroids. A second injection is particularly problematic, but it can happen after one shot, too.
Let’s assume the steroid injection is going to go forward. (As an ID doctor, I will not debate the merits of this widely used treatment, controversial as it may be in some settings.)
So it’s time to change the HIV regimen, right? Given his history and only one-class resistance, this shouldn’t be too difficult — but there’s a history of intolerance to efavirenz, and to raltegravir, and he may have unreliable stomach acidity. Note that intramuscular injections would be dicey given the underlying coagulopathy.
What would you recommend, and why?
Categories: Antiretroviral Rounds, Health Care, HIV, Patient Care
Tags: Antiretroviral Rounds
You can follow any responses to this entry through the RSS 2.0 feed. Both comments and pings are currently closed.
10 Responses to “A Return of Antiretroviral Rounds — What Regimen Would You Choose?”

Paul E. Sax, MD
Contributing Editor
NEJM Journal Watch
Infectious Diseases
Biography | Disclosures | Summaries
Learn more about HIV and ID Observations.
Follow HIV and ID Observations Posts via Email
- Two Pandemics, Compared: Reflections on HIV and COVID-19
- The Mystery of the Isolated Hepatitis B Core Antibody, Solved
- Federal HIV Guidelines Face a Shutdown — A Critical Loss for Clinicians and Patients
- Why the Sudden Firing of ACIP Members Should Put Every Clinician on High Alert
- How ID Doctors Get Paid, Part 3: The Grab Bag Edition
- ID Cartoon Caption Contest (125)
- ID Cartoon Caption Contest #2 Winner — and a New Contest for the Holidays (92)
- Dear Nation — A Series of Apologies on COVID-19 (80)
- How to Induce Rage in a Doctor (77)
- IDSA’s COVID-19 Treatment Guidelines Highlight Difficulty of “Don’t Just Do Something, Stand There” (74)
-
 NEJM Journal Watch — Recent Infectious Disease Articles
NEJM Journal Watch — Recent Infectious Disease Articles- RSV Infection Substantially Raises Risk for Cardiovascular Events
- Pediatric Hospitalizations for Mycoplasma pneumoniae Rose Sharply in 2024
- Sulopenem, a New Antibiotic for Uncomplicated Urinary Tract Infection
- Is Cardiovascular Risk Sustained After SARS-CoV-2 Infection?
- Which Hepatitis B Vaccine Provides the Longest-Lasting Protection in People with HIV?
-
Tag Cloud
- Abacavir AIDS antibiotics antiretroviral therapy ART atazanavir baseball Brush with Greatness CDC C diff COVID-19 CROI darunavir dolutegravir elvitegravir etravirine FDA HCV hepatitis C HIV HIV cure HIV testing ID fellowship ID Learning Unit Infectious Diseases influenza Link-o-Rama lyme disease MRSA PEP Policy PrEP prevention primary care raltegravir Really Rapid Review resistance Retrovirus Conference rilpivirine sofosbuvir TDF/FTC tenofovir Thanksgiving vaccines zoster

The NNRTI should be active. I’d avoid the InSTIs (esp long acting) given his reaction but could trial B/F/TAF if had to. But only would have to if a big bad insurance company denied doravirine.
This is an extremely insightful comment!
-Paul
I believe all options will work in terms of the viral load. DTG and DOR are more likely to produce intolerance due neurological side effects than BIC. I’m guessing monitoring kidney function and the liver given the history of the patient, although hepatotoxicity has been associated to other drugs rather than BIC in the regimen. Further, this should be more safe since the patient is already tolerating FTC/TAF.
This was my reasoning to. I wanted to select (and would have suggested biktarvy) but what insurance would deny that? Doravirine had to be denied is my guess ..
I love these cases because despite a somewhat complicated history, you can still do pretty much anything.
I like the doravirine option. We have switched so many patients off of PI based therapy and onto INSTIs so why do something different? Possibly to avoid any excess weight gain from INSTIs in a patient we feel would maintain suppression with doravirine. Not sure what the bmi is but patient is probably more sedentary given the arthritis. Intolerance to RAL is probably not a major reason to avoid other INSTIs and the patient would also likely do great with either dtg/3tc or b/f/taf
This is prime time for shared decision making. You have someone who is very experienced in this world who you can talk about all the options with and likely trust to get back to you. Personally? I’d try him on an INSTI regimen for a month. If he feels like trash go to DOR.
All three options (TAF/FTC/BIC, 3TC/BIC or TAF/FTC+DOR) are expected to be active, so no problem selecting if looking for antiviral efficacy.
Intolerance to EFV and RAL does not implies intolerance to DOR, DTG or BIC but intolerance to any of them is possible. If the patient agrees, I would try one of them and reassess tolerance. I would start with doravirine (although in a switch trial it did not show an advantage when changing EFV, it is not the same case because the patient has been without EFV for many years). And if it is not tolerated, I would try other option.
Note: In Spain all three options are cheaper than TAF/FTC/DRV/c.
Considering that he had not failled to lamivudine and the change of raltegravir wasnt because of any mutation, o would recommend 3tc + dtg.
We already know that he has good adherence to pills and nowadays we already have the one pill option. Despite of the steroid treatment i would recommend this pair combination
Your hint about the patient’s wonky gastric pH makes me less confident bictegravir will work, although I could be paranoid. DOR should work even against EFV resistant viruses, which seem unlikely given what sounds like a short run stopped for intolerance. Whatever you chose, looking forward to learning from you again…
I chose the doravirine option. We know that it has fewer CNS side effects than efavirenz, and there is far less information about side effect differences between the various INSTIs. Fortunately, all three of the choices are likely to maintain virologic suppression.