An ongoing dialogue on HIV/AIDS, infectious diseases,
July 4th, 2009
Progress on Consent for HIV Testing?
 As I’ve noted here several times (some might say ad nauseum), I am convinced that Massachusetts’ arcane law requiring written informed consent prior to HIV testing is a barrier to more widespread screening — an opinion that is shared by virtually every clinician I’ve asked about this issue.
As I’ve noted here several times (some might say ad nauseum), I am convinced that Massachusetts’ arcane law requiring written informed consent prior to HIV testing is a barrier to more widespread screening — an opinion that is shared by virtually every clinician I’ve asked about this issue.
Last week, there was an announcement about progress (of sorts):
Clearing the way for HIV testing to become almost as routine as checking for cholesterol, state public health officials issued an advisory yesterday saying that the written consent required by law can be included in general permission forms patients sign for medical care.
Until now, Massachusetts doctors have typically given patients separate consent forms to authorize HIV testing, but yesterday’s directive makes clear that one form is sufficient, as long as the general consent form explicitly mentions HIV testing. Separate permission forms pose a barrier to testing for patients and healthcare providers alike, health officials said.
I’m of two minds about this. On the one hand, we could simply do away with the law — something that most other states have already done, with Connecticut’s pending legislation providing a wonderfully common-sense approach on how to do this.
In addition, putting HIV in with the general consent for medical care seems both 1) kind of sneaky (does anyone actually read all that paperwork?) and 2) perpetuating HIV exceptionalism, since no other specific diseases are mentioned.
These concerns notwithstanding, I’m all for anything that makes it easier for people to find out their HIV status. As noted in this article, 31% of people in MA find out they have HIV within 2 months of an AIDS diagnosis.
And that’s 31% too high.
June 20th, 2009
More HIV in the Adult Film Industry (Maybe)
From the New York Times last week:
Health officials in Los Angeles said Friday that 22 actors in adult sex movies had contracted HIV since 2004, when a previous outbreak led to efforts to protect pornography industry employees.
(snip)
Occupational health officials have long argued that failing to require that performers wear condoms during intercourse and other acts is a violation of safe-workplace regulations.
But Deborah Gold, a senior safety engineer with the California occupational health department, said violations in the pornography industry were so widespread that the state had a difficult time cracking down.
My first response on reading this was amazement that the number was so small — and, remarkably, that number turned out to be even smaller (1 case) when further details emerged in the LA Times:
Los Angeles County public health officials backtracked Tuesday on their statements last week that at least 16 unpublicized cases of HIV in adult film performers had been reported to them since 2004.
Despite their release of data to The Times describing the cases as “adult film performers,” the county’s top health official acknowledged that the agency does not know whether any of those people were actively working as porn performers at the time of their positive test.
(snip)
The county lacks sufficient information to delve deeply into the cases and still has received no formal report on the most recent case.
“The system we have and the laws we have do not facilitate the kind of contact tracing and verification that we’d like to see,” [LA County Health Officer] Fielding said. “AIDS has been treated separately from other STDs.”
Bottom line here: Aside from this well-researched cluster of cases reported in 2004 in the MMWR, we likely only have a vague idea how many cases of HIV are in, or linked, to this “industry” — which in addition to these semi-regulated companies undoubtedly has a huge underground as well.
And until we get rid of this bit of HIV exceptionalism cited above by Dr Fielding, appropriate contact tracing and partner notification are going to be very difficult indeed.
June 8th, 2009
H1N1: A Tale of Two Practices
 As an adult ID/HIV doctor, I must say the clinical impact of H1N1 thus far has been underwhelming, notable more for the calls about prophylaxis or suspected cases than the real thing.
As an adult ID/HIV doctor, I must say the clinical impact of H1N1 thus far has been underwhelming, notable more for the calls about prophylaxis or suspected cases than the real thing.
(Last week, one patient with fever and “suspected swine” — hard for people to shake that name — turned out to have … Lyme disease. Ah, New England in June.)
But for my wife, the pediatrician? There’s a full-blown epidemic out there, with outpatient visit volumes way up, and nearly continuous oseltamivir prophylaxis among her staff. As in mid-winter, she and her practice partners are routinely making the influenza diagnosis based on symptoms alone.
And while this report suggests the age cut-off for partial immunity to H1N1 is 60, I suspect strongly — based on our highly-anecdotal, two-doctor-family, completely non-scientific observation — that it’s going to turn out to be quite a bit younger.
June 1st, 2009
“Long-term Nonprogressors” and “HIV Controllers”: Rare Indeed
 When giving an overview of HIV pathogenesis to a group of clinicians, Bruce Walker usually asks the assembled if they have any patients in their practice who have undetectable viral loads without antiretroviral therapy.
When giving an overview of HIV pathogenesis to a group of clinicians, Bruce Walker usually asks the assembled if they have any patients in their practice who have undetectable viral loads without antiretroviral therapy.
Generally about three-quarters of the audience has at least one such patient. They are then asked to refer them to his research cohort, which has a goal of trying to figure out why some patients can control HIV replication without needing antivirals.
But how common is this “controller” phenomenon really? And how about its immunologic correlate — people with long-term HIV infection but no significant decline in the CD4 cell count?
Nifty paper in AIDS this month trying to answer this question: Using the French Hospital Database, and starting with over 45,000 potentially eligible patients, the group found that only 69 were “elite controllers” — that is, had >10 years HIV infection, 90% of viral loads <500 cop/mL, and most recent viral load <50 cop/mL.
Stable CD4s were even less common. Only 25 patients were “elite long-term nonprogressors” — that is, had HIV for more than 8 years, CD4 cells > 600, and no CD4 cell decline. That’s an prevalence of 0.05%, or 5 for every 10,000 patients.
Medical students and residents sometimes ask me if a particular patient of mine, asymptomatic and not on antiretroviral therapy, is a “long-term nonprogressor.”
I always respond by asking them what specifically they mean by the term — because as this paper shows, when you look for a truly benign course of HIV infection, you need to look pretty darn hard.
May 28th, 2009
The Paul Farmer Watch
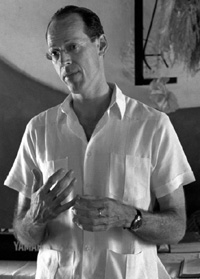 Our pal Paul Farmer keeps racking up the titles:
Our pal Paul Farmer keeps racking up the titles:
Dr. Paul Farmer, a pioneer in improving health services in the Third World, has been named chairman of Harvard Medical School’s Department of Global Health and Social Medicine …
(snip)
Peter Brown, spokesman for Brigham and Women’s Hospital, said Farmer also had been named to succeed Kim as head of the Division of Global Equity at the hospital, a Harvard teaching facility.
Of course what we we’re all wondering is whether he’ll stop with these, or go on also to accept a senior role in the Obama administration:
After weeks of feeling neglected and anxious that no new administrator has been named, USAID and international development community sources tell The Cable they are excited at reports that Paul Farmer, the legendary cofounder of an innovative group that has delivered healthcare to the poor in central Haiti and beyond, is under consideration to head the U.S. aid agency or serve in a top administration international assistance post that would encompass it.
Regardless of his decision, there is a huge irony here — which is that if ever there were a person in our field who couldn’t seem to care less about titles, it’s this guy.
Which is how it should be, of course.