An ongoing dialogue on HIV/AIDS, infectious diseases,
May 18th, 2011
HIV Exceptionalism and the Department of Unintended Consequences
Quick question: If there were one piece of information — clinical or lab — that you would use to determine the quality of care in an HIV  program, what would it be? (Choose one.)
program, what would it be? (Choose one.)
- Rates of influenza vaccine administration
- Receiving PCP prophylaxis with CD4 < 200
- Adherence counseling before starting antiretroviral therapy
- Baseline toxoplasmosis serology
- Proportion of patients on treatment with suppressed viral load
Maybe I’m being presumptuous here, but one of these — virologic suppression — completely blows the rest of them away. Sure, the others are worthwhile, but data linking them to improved outcomes for people with HIV are either pretty weak (adherence counseling, flu vaccine) or nonexistent (toxoplasmosis serology).
Even the use of PCP prophylaxis for CD4 < 200, which was highly effective and prolonged survival in the pre-ART era, doesn’t come close to the benefits of effective ART. One paper even questions whether we need it, provided that the person is on fully suppressive HIV therapy.
So why bring this up under the title of “HIV Exceptionalism”? Because a certain unnamed institution in an unnamed city (hint: begin with “B”) cannot obtain the aggregate viral load data on their own patients as part of a quality improvement initiative.
The reason? Anything with “HIV” attached to it, you see, is privacy-protected information under Massachusetts Chapter 111, Section 70F, unless the patient provides written informed consent. No exceptions listed.
Which means that people with HIV can’t participate in this quality improvement program — in effect, are discriminated against — due to a law that in the post HIPAA era should not even be necessary, since all medical information is now considered confidential.
The state law on HIV testing and privacy, by the way, dates back to when HIV was called “HTLV-III”, and it’s showing its age. Fortunately, revisions to it are in the works that allow for appropriate testing, clinical care, research, and quality improvement.
Stay tuned.
May 17th, 2011
Physician Bloggers Categorized
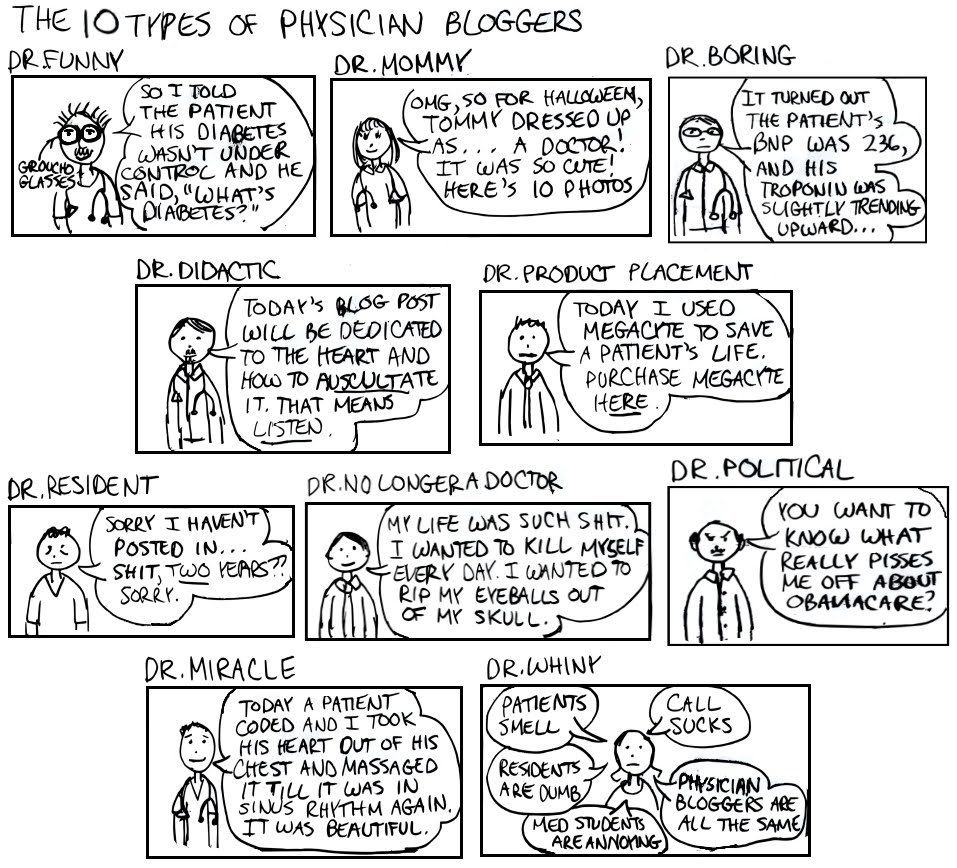 About a year ago I linked this cartoon from “Dr. Fizzy”, and I’ve been a regular visitor to her site ever since.
About a year ago I linked this cartoon from “Dr. Fizzy”, and I’ve been a regular visitor to her site ever since.
Anyway, more kudos to her for this dead-on categorization of MD bloggers.
(I guess the British “spot-on” is a better choice for us docs.)
Not exactly sure where I fit in this list — yikes — but boy does she get it right here.
In fact, one could replace “The 10 Types of Physician Bloggers” with “The 10 Types of Physician Dinner Companions”, and you’d have a good description of how we MDs interface with the world in pretty much every setting.
May 9th, 2011
Routine Screening for Anal Cancer: Are We There Yet?
A paper recently published in AIDS evaluated the cost effectiveness of various strategies for anal cancer screening in HIV positive men-who-have-sex-with-men (MSM).
The “bottom line” (ahem):
In HIV-infected MSM, the direct use of high resolution anoscopy is the most cost-effective strategy for detecting anal intraepithelial neoplasia
High-resolution anoscopy without any prior testing was the most cost-effective of 18 strategies assessed for initial anal cancer screening… This study suggests that direct use of HRA is a reasonable strategy for initial anal cancer screening in a population with a high prevalence of disease. Several other strategies were also effective at a moderate cost, including the one used in my own practice: initial anal cytology, with referral to HRA for individuals found to have atypical squamous cells (ASCUS) or greater.
We covered this area of controversy around a year ago on this site, at which time Joel Gallant admitted to an even less aggressive strategy — namely, not referring patients with ASCUS for HRA at all, but simply monitoring them with yearly pap smears.
His rationale?
My patients don’t enjoy going through HRA, biopsy, and ablation, the parallels between anal and cervical dysplasia aren’t perfect, and the protocols around anal Pap smear are written without much evidence backing them up.
As you might have guessed, I have tremendous ambivalence about what to do about anal cancer screening as of May 9, 2011 (today). On one side: this is a highly morbid (and potentially fatal) complication of HIV, a screening protocol, however vague, is out there, and there are advocates who strongly support screening.
On the other side are the issues cited by Joel, the lack of recommendations for anal cancer screening in published guidelines, and the fact that at one of my two practice sites, there has been no single provider who readily offers HRA.
Just speculation here, but on a national level, this last factor might be the most important driver in how often HRA is done at all.
And just like any situation where test availability drives volume, there’s something not quite right about that.
May 4th, 2011
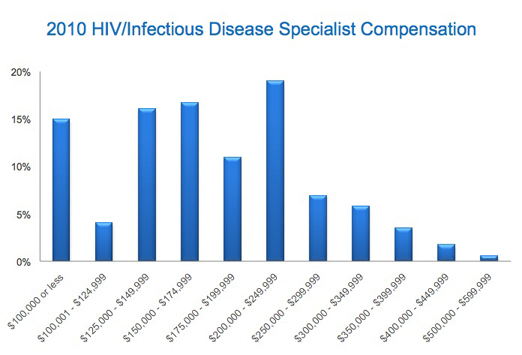
How Much Do ID/HIV Doctors Get Paid?
 A long time ago, I was very close to becoming a Cardiologist. Really.
A long time ago, I was very close to becoming a Cardiologist. Really.
Even though my fascination with ID and microbiology started in medical school — and believe me, not much fascinated me in medical school — the fact that all the top residents in my program were going into Cardiology made me feel that somehow I should be doing this too. Plus, the guy who was Chief of Medicine was very influential.
When I came to my senses, and realized that I wanted to go into ID, there was a small problem — I had already matched in a Cardiology program. Hence I faced the tricky task of telling the program director, “Thank you very much for your kind offer, but I’ve decided I want to be an Infectious Diseases specialist.”
I remember his look of annoyance (understandable). It was soon replaced by one of disbelief. And then came a line I will never forget:
At least your motivation isn’t financial — ID doctors get paid s–t.
All of this came back to me when I read this fascinating survey over on Medscape on what we doctors get paid.
Some of the interesting results:
- Yes, ID specialists (median of $174,750/year) are at the lower end of the specialist scale. Other bottom feeders? Pediatricians (it’s a family thing), Rheumatology, Endocrinology, Primary Care …
- And the program director at my cardiology-fellowship-that-never-happened was right: Cardiologists are the third-highest-paid physicians (after orthopedic surgeons and radiologists), with a median income of $325,000. 20% of Cardiologists report making more than $500,000, while almost this many ID/HIV docs get < 100,000.
- However, despite this disparity, a higher proportion of ID docs (55%) than Cardiologists (45%) report they were fairly compensated. Is that because ID is the most fascinating field in medicine? And that an endocarditis case is surely more interesting than the simple plumbing they generally care for? (That was a joke. Some of my best friends are cardiologists.)
- Weird disconnect between geographic cost of living and salaries, with the lowest pay coming in the most expensive places to live. This is of course the complete opposite of salaries in business, banking, and law. So if you want your doctor’s pay to go further, don’t live in California or Washington/NYC/Boston!
Of course, as we tell our kids, when choosing a career, it’s not about being rich — it’s about being happy.
But if you want to be both rich and happy, the specialty-of-choice is clearly Dermatology — median annual income is nearly $300,000, and a whopping 93% said they’d choose the same specialty again, the highest of all the fields surveyed.
Acne treatment never looked so good.
April 28th, 2011
Hepatitis C Week is Upon Us
 After many — and I mean many — years of telling patients that new hepatitis C drugs were “coming soon,” that time has finally come.
After many — and I mean many — years of telling patients that new hepatitis C drugs were “coming soon,” that time has finally come.
An FDA Advisory Panel yesterday favorably reviewed the HCV protease inhibitor boceprevir; today telaprevir got the same unanimous report. The FDA will certainly follow with approval for both drugs, and hence they will be available for actual use soon.
While these are undoubtedly huge advances for patients with HCV genotype 1 — who faced a 30-40% chance of cure with IF/ribavirin now, compared with up to 80% by adding one of the new drugs — many questions remain about how they will be used, and in whom.
In no particular order, and without even trying to be comprehensive, here are some of the “known unknowns“:
- How will clinicians choose between them?
- Is a 4-week lead in with IF/RBV (as was done with the boceprevir studies) necessary? Additionally, is it useful, by identifying “null” responders who will have a higher rate of developing treatment failure and PI resistance? Could starting all three drugs simultaneously improve outcome?
- How long should treatment be? Will this vary depending on HCV RNA kinetics from person-to-person? Seems like this is a situation ripe for sophisticated modeling, and that more frequent HCV RNA monitoring (especially early) will inform this decision.
- How will patients in the chaotic real world tolerate these drugs? Interferon/ribavirin is already no picnic, and adding these additional meds will mean additional side effects.
- Related: Besides the signature toxicities (telaprevir — rash and anemia, boceprevir — anemia and dysgeusia), what other side effects will appear with more widespread use? Note that it’s not a question of if these side effects will occur, it’s when will occur, and what they will be.
- How will resistance be assayed? Will genotype testing become commercially available? If so, what new combination of letters and numbers (i.e. mutations) will need to be memorized?
- How do these advances influence treatment decisions about the patients who don’t have HCV genotype 1, especially those with genotype 4? I suspect not at all, at least for now.
- How will compliance be with these three-times a day regimens? Will it improve over the course of therapy, or will patients get “pill fatigue.” We know they will get regular fatigue — I have yet to see a patient receiving interferon who didn’t mention this as a side effect.
- View from 20,000 feet: If someone is currently very stable — with low risk of HCV disease progression — should they “act now” or wait for even better, less toxic options? Given the huge effort in HCV drug development, how long before we have treatments for HCV that are comparably simple to HIV therapy? Is a single-pill combination tablet too much to ask? Remember, for HIV, such a treatment would have been unimaginable in 1996; less than 10 years later it was the mostly widely-used HIV combination in the country, and remains so today.
- Who will be the HCV Providers? Will the legacy of gastroenterologists’ leading the way in hepatitis therapy continue, or will this Infectious Disease finally be embraced by Infectious Disease Doctors? (Italics represent my view.)
- How much will the new drugs cost? Will they be covered for all patients? How about for those who have a favorable IL-28B genotype — and would be likely responders to IF/RBV alone?
- How will our HIV co-infected patients respond? Data are extremely limited — and the drug-drug interactions promise to be unbelievably complex. As of April 28 2011, we only have data on use of telaprevir with either EFV or ATV/r.
- How do you design an HCV clinical trial once these drugs are approved? Will all “control” arms now need to be IF/RBV + something-previr?
Answers to some of these questions will come with formal FDA approval, which will necessarily include some “package insert” indications for therapy.
But stay on your toes, because it seems highly likely that this is one therapeutic area in ID that truly lends itself to the cliche, “moving target.”
April 25th, 2011
FEM-PrEP: A Set Back in HIV Prevention Research
HIV prevention has been on such a roll recently that the recent negative news from the FEM-PrEP study came as something of a surprise. Bottom line:
Following a scheduled interim review of the FEM-PrEP study data, the Independent Data Monitoring Committee (IDMC) advised that the FEM-PrEP study will be highly unlikely to be able to demonstrate the effectiveness of Truvada [emtricitabine (FTC) and tenofovir disoproxil fumarate (TDF)] in preventing HIV infection in the study population, even if it continued to its originally planned conclusion. FHI subsequently concurred and has therefore decided to initiate an orderly closure of the study over the next few months.
When studies are stopped early by a data and safety monitoring board, the investigators are of course as taken by surprise as the rest of us, and hence lots of details from this study are still not available.
As a result, we can only speculate why TDF/FTC (Truvada) worked for prevention of HIV among gay men, but not among heterosexual women. Some (unofficial) thoughts thoughts from my friend/colleague Raphy Landovitz, who does research in HIV prevention:
I’m willing to bet it all comes down to adherence, with the proof to come in the drug-level analyses. As iPrEx showed, self report of 95% in both arms is meaningless. One also wonders if there was more condom non-adherence as part of fertility goals.
Regardless of the cause, these negative results underscore one of the most important specific items in the CDC “Guidance” on use of PrEP: that for now, if it’s prescribed, the only appropriate recipients are high-risk MSM.
[Edit: Nice summary of the FEM-PrEP study findings and implications over here in Journal Watch HIV/AIDS Clinical Care.]
April 18th, 2011
When to Start Antiretroviral Therapy, Take 3
 A third observational study on “When to Start ART” has just appeared in the Annals of Internal Medicine, “The HIV-CAUSAL Collaboration.”
A third observational study on “When to Start ART” has just appeared in the Annals of Internal Medicine, “The HIV-CAUSAL Collaboration.”
As with ART-CC and NA-ACCORD, it’s a large study, starting with over 20,000 people with HIV with baseline CD4s >500 receiving care in Europe and the United States. Out of this group, 8392 experienced CD4 declines into the 200-500 range and are included in this analysis. Outcomes of interest are mortality and new AIDS-related events, depending on when combination ART (“cART”) was started.
The results?
Initiation of cART at a threshold CD4 count of 500 increases AIDS-free survival. However, mortality did not vary substantially with the use of CD4 thresholds between 300 and 500.
The authors also cite a “number needed to treat” of 48 for starting at 500 rather than 350 for prevention of AIDS or death, a fairly low number when compared to some interventions widely adopted in cardiovascular disease.
While not the blockbuster results of the NA-ACCORD study — whose nearly two-fold reduction in mortality for starting at >500 remains both unreproduced and, let’s face it, unexplained — these results still point to a substantial clinical benefit of starting ART before CD4s fall too low.
In addition, none of these large observational studies even hints at a negative effect of starting early on clinical outcomes, and other potential benefits of treating HIV (reduced risk of HIV transmission, reduced long-term incidence of non-AIDS events) can’t be included.
As nicely summarized in the accompanying editorial, the quantitative benefits of early ART can’t come close to the benefits of late ART, which are nothing short of miraculous.
It’s up to us — patients, providers, society — to determine whether early ART is worth it.
April 15th, 2011
A “New” Antiretroviral Option Quietly Enters the Market
There’s a new antiretroviral option out there, a 400-mg extended-release tablet formulation of nevirapine that can be dosed once daily.
However, you might not have noticed, since it’s not really that new, and it’s not clear that this formulation offers any significant advantages over the nevirapine we already have. Writes Keith Henry over in Journal Watch:
Issues that will temper enthusiasm for the new formulation include continued concern about serious adverse effects with nevirapine (namely, Stevens-Johnson syndrome in the general patient population, and liver toxicity in women with CD4 counts >250 cells/mm3 and men with CD4 counts >400 cells/mm3), the availability of safe and effective non–nevirapine-containing regimens, the likely approval of additional one-pill once-daily regimens (e.g., tenofovir/FTC/rilpivirine, abacavir/3TC/dolutegravir, and tenofovir/FTC/elvitegravir/cobicistat), and the possibility of nevirapine coming off patent in 2012 (which creates potential for a lower-priced generic).
Add to these issues the need to still take* the 200 mg once-daily lead in for 14 days, and one wonders how much use this “new and improved” nevirapine is going to get.
(*I know, split infinitive — it just sounds better that way!)
April 11th, 2011
Organ Transplants from HIV-Infected Donors
On the heels of last month’s report of HIV transmission from an organ donor — covered here in Journal Watch — comes this remarkable article in the New York Times about lifting the ban on organ donation from donors known to be HIV positive.
Naturally, the first group of patients slated to receive these HIV positive organs would have HIV themselves.
But the article goes further:
But some experts, including Dr. Segev and Dr. Kuehnert, say they can foresee such transplants even for H.I.V.-negative patients because contracting H.I.V. would be preferable to kidney or liver failure.
“I don’t want to minimize living with H.I.V, but it is a medically treatable disease now,” said Charlie Alexander, president of the United Network for Organ Sharing, which manages the country’s organ transplant system. “In certain cases, I think it would be medically appropriate.”
If ever there were proof that HIV is now a highly-treatable condition, I’d say this could be Exhibit One.

