An ongoing dialogue on HIV/AIDS, infectious diseases,
May 6th, 2015
An Apology to Subscribers, and Five Random ID/HIV Questions to Ponder
Some of you have been kind enough to enter your email address in the little box on the right side of this page, which gives you a “subscription” to this site. It looks like this:
We thank you for signing up! Delivery is usually prompt and reliable (even during this past winter’s historic snowstorms), and the price can’t be beat (free).
But this week, due to a fascinating technical glitch — text copied from the FDA web site included a prohibited character, a little empty box — no e-mail notification was sent out with the latest post. Our apologies! For the record, the post included various thoughts on the nettlesome problem of fat accumulation syndromes in HIV, and a terrific video from that famous ID specialist John Stewart.
In exchange for this inconvenience, we’re offering a full refund — plus a bonus Five Random ID/HIV Questions to Ponder
- Could this investigational zoster vaccine really be 97% effective? Total game-changer for shingles prevention if it turns out to be this effective and safe.
- Are we going to call the newest azole antifungal “isavuconazole,” or by it’s weird real name, “isavuconazonium?” Strongly hoping the former.
- What percentage of ID doctors know exactly what “MALDI-TOF” stands for? My guess: 54%.
- Has anyone prescribed elvitegravir or cobicistat as individual agents? Probably — it’s a big country. But why did they do this?
- Why did several people in Colorado catch plague from a sick dog? Yikes, a few chewed shoes you expect. But plague?
Speaking of plague …
May 4th, 2015
A Drug for Neck Fat, and Some Thoughts on Fat Accumulation Syndromes in HIV
 It’s not often that a FDA drug approval for cosmetic dermatologists and plastic surgeons will get the attention of HIV/ID specialists, but this past week was an exception. From the FDA report:
It’s not often that a FDA drug approval for cosmetic dermatologists and plastic surgeons will get the attention of HIV/ID specialists, but this past week was an exception. From the FDA report:
The U.S. Food and Drug Administration today approved Kybella (deoxycholic acid), a treatment for adults with moderate-to-severe fat below the chin, known as submental fat … Kybella is a cytolytic drug, which when injected into tissue physically destroys the cell membrane. When properly injected into submental fat, the drug destroys fat cells; however, it can also destroy other types of cells, such as skin cells, if it is inadvertently injected into the skin.
Those of you who don’t practice HIV medicine might not know this, but various fat accumulation syndromes remain a bedeviling problem for our patients. And while I have absolutely zero experience with this new fat-melting injection stuff, I doubt I’m the only HIV specialist who didn’t immediately think of a few patients who could be candidates. Here’s a representative image, courtesy Medscape.
For these patients, the office visit will generally go something like this, almost invariably with someone who has been doing great on treatment for years:
HIV MD: Hi —-, your numbers look terrific — viral load undetectable, CD4 normal, liver and kidney tests fine.
PATIENT: Good to hear! Anything I can do about this weight gain? And this big belly? And look at my neck! I was looking at my drivers license recently, and I look totally different!
HIV MD (Uh-oh, this is a tough one.): Well, there’s diet and exercise.
PATIENT (Does he think I don’t know that? Jeesh.): Yes, of course. What I mean is, are these meds causing me to get fat? If so, should I switch treatment to make it better?
HIV MD (Doing his/her best.): It’s not really the medications themselves, not directly. And switching the meds isn’t going to help. The reason for weight gain on HIV treatment is complicated, and caused by several things … (Various hypotheses outlined, none of them straightforward or easily remediable.)
PATIENT (Oh well. I still think it’s the meds.): OK, thanks.
Now about those “various hypotheses” — below is a short synthesis of what might be going on, by no means meant to be authoritative or comprehensive, but just to get the conversation started:
- Untreated HIV induces a catabolic state. This is particularly the case for patients with advanced disease, where energy expenditure exceeds intake, leading to weight loss. This is the main reason why HIV alone caused wasting, even without a diagnosis of an opportunistic infection. Classic review article here from 23 years ago!
- The main driver of this catabolic state is decreased appetite. In research done in the pre-ART era, a careful analysis of energy intake and expenditure among untreated HIV patients showed that their actual metabolism was often lower than normal — or at most, a little increased — but their food intake was dramatically reduced. The cause of this anorexia is most likely high levels of circulating inflammatory cytokines, such as tumor necrosis factor. This decrease in food intake is often not noted by patients — who may remark, when newly-diagnosed with HIV and very low CD4 cell counts, that they have recently had “successful” weight loss for the first time in their adult lives.
- Effective HIV therapy reverses this catabolic process. Once a person starts on ART, inflammatory cytokines drop, appetite improves, and, as I tell my patients, “the virus is no longer eating any of your food.” The result is not surprisingly weight gain, which is gratifying, even thrilling, especially if there had been serious weight loss.
- The weight gain from effective HIV treatment can be both rapid and too much of a good thing. News flash — there’s an obesity epidemic in most of the world. Not surprisingly, once HIV is treated, our patients become just like the non-HIV population — prone to excessive consumption of processed, packaged, and high caloric junk. In fact, they might be more likely to eat these foods since they are hungry all the time. If they had previously been quite sick from AIDS, then they might also be deconditioned and hence less likely to exercise. And if they’re older, they already have a naturally slower metabolism. Both advanced HIV disease and older age are risk factors for increased weight gain on treatment.
- Rapid and excessive weight gain leads to fat accumulation. In a different form of pathologic “refeeding syndrome” than described in the medical textbooks, the rapid weight gain from HIV treatment can cause fat deposition, most commonly in certain anatomic sites. Probably the best described is excessive abdominal visceral fat, which is associated with increased cardiovascular risk and that big belly the above “patient” described. But abnormal fat accumulation isn’t just limited to abdomen, and every HIV clinician has patients with significant fat deposition in the neck (both anterior and posterior) and upper trunk.
You’ll note that the above list does not cite any specific HIV drugs responsible for this process. That was intentional.
Remember when we used to say that the NRTIs caused lipoatrophy, and the PIs fat accumulation? Turns out we were half right (the first part): the best data we have from randomized clinical trials emphatically does not conclusively implicate one class of drug any more than others. Here’s the most recent of these studies, comparing fat gains with raltegravir, atazanavir, and darunavir-based regimens. I’m sure if you polled a hundred HIV specialists before this study was done, 99 would have bet that raltegravir would be associated with the least fat gain. And 99 would have lost that bet, as all were essentially the same.
So for now, what can we do? A few options:
- Education. We need to do a better job educating our patients about this potential effect of HIV treatment. (Note I don’t say “side effect.”) It’s a return-to-health phenomenon, so the weight gain is a good thing. But a bit of advice about high-quality foods (I’m a big fan of this Michael Pollan book), watching calories, and exercising might do something to prevent excessive weight gain. And we have to be clear it’s not the HIV meds. Switch strategies expressly for this purpose are likely to fail.
- Tesamorelin. The growth hormone releasing hormone analogue with the sonorous name, tesamorelin is FDA-approved for visceral fat accumulation in HIV. On the plus side it clearly does reduce central fat in some patients. On the minus side it’s a
twiceonce-daily injection, it’s expensive, the effects quickly reverse when it’s stopped, and it doesn’t work in all patients. But for a select few, it does the trick. - Make friends with a good plastic surgeon and cosmetic dermatologist. Though several years ago the makers of a facial filler tried to engage HIV specialists in doing these procedures, let’s be frank — it’s best left to the people who do this kind of thing for a living. Some patients will have great results.
- Lobby and advocate. Lots of these treatments aren’t covered by insurance, making them unavailable to those who really need them. That’s a shame, because in severe cases these are highly stigmatizing and dramatically reduce quality of life — they should be covered!
- Research. If there’s a specific cause to this weight gain and fat accumulation problem, let’s see if we can figure it out. Fortunately, there are lots of smart people who continue to study the mechanisms of this process.
Meanwhile, if anyone has experience with this new drug for neck fat, let me know!
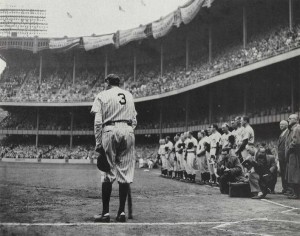
And enjoy this video, just because we’ll miss him…
April 22nd, 2015
Seriously — How Much Would You Pay for a Curbside Consult?
Let me start with an email exchange I had with a PCP recently:
Hi, Paul, quick question 😉 This lady, 49 YO woman from Haiti, asymptomatic, totally healthy. Got TSpot done for immigration purposes, it’s positive with negative chest Xray. Treated with INH 6 months in 2001. She travels to Haiti annually so could had been reexposed, though doesn’t report being with anyone with TB. Do I need to treat her again? THANKS!
Carla
To which I responded:
Hi Carla, unless there’s been a significant re-exposure and immunosuppression, no need to re-treat.
Paul
p.s. You know we could start getting paid for these “eConsults.” How much do you think they are worth?
So it’s now Carla’s turn to answer my question:
Priceless!!!! Seriously, not sure, since some questions are more complicated than others. Sometimes it’s straightforward like this, and sometimes you have to review more data so that should be compensated more no?
Carla helped me out here, especially with her first response — priceless indeed. But the second part — where she suggested that this “straightforward” question is worth less a more complex one — hints at why estimating the value of these consults is so difficult.
And it’s important that we figure it out, and soon. With the inevitable move to “value-based” insurance contracts, many ID doctors are getting the push to formalize these clinical relationships. That’s a good thing, as clearly getting advice from a colleague can be a more efficient way to provide quality care than referring everyone for a formal consultation, and it puts a value on what previously was almost always done gratis.
Back to the question in the email — is it so straightforward? Clearly not to Carla, who as a generalist has to manage all medical problems not just ID ones, but to us brilliant ID doctors, sure. An IGRA (the T-Spot) and tuberculin skin test are basically two different ways of looking at the same thing (evidence of immune response to TB), and I’ve already been asked this question (or one like it) several times. Plus, I can touch-type (as I’ve bragged elsewhere, I could crank out over 70 words/minute in my 8th grade typing class), and happened to be sitting at my desk daydreaming about puppies playing baseball when the email popped into my in box.
Even if you account for the distraction factor — it was hard to get that puppy image back — it still took only a few minutes.
And as I’ve calculated before, if paid on an hourly basis, this comes out at a whopping $6/consult, or almost enough for a couple of fancy coffees at Starbucks. If we believe the good news from this latest Medscape salary survey that ID doctors are no longer in the basement when it comes to annual salaries — sorry, pediatricians — we’re only up to $8/consult (add a bagel to your coffee order).
So when it comes to curbsides, if you pay by time/consult, we ID doctors could be in deep trouble — the faster we do it, the less time-value it has, and the less we make. It’s quite different with surgeons — they get paid more with greater experience and efficiency.
Furthermore, though the fee-for-service model is horribly broken for ID as a specialty — no way to win on either volume or procedures — our clinical productivity is still mostly measured by how many patients we actually see. Every curbside we do is potentially a patient visit that didn’t happen. Note again how we differ from surgeons and other procedural specialists — from a revenue perspective, they have an incentive to keep simple non-operative cases out of their clinics.
Finally, the consultant is taking on some non-zero medicolegal risk. Should that be somehow factored into the compensation? In this excellent review — which is very pro-curbside — the author states that courts have consistently concluded that there is no actual medicolegal risk to the person being curbsided provided there is no relationship between him/her and the patient. However, he also accurately states: “Of course, even in the absence of actual liability, there is always a possibility that the consulted physician will be sued for medical malpractice. Although such a physician should ultimately prevail as a matter of law, the entire process is best avoided [emphasis mine].” Hard to disagree!
Other payment models are out there for informal consults, such as getting a flat rate per consult regardless of complexity (how much?), or getting a percentage of your salary covered for being “on call” for this service (what percentage?). And of course many will still have to live with the status quo of getting nothing — gratitude counts for something.
Provided, of course, it doesn’t end with (pet-peeve alert) “Thanks in advance!” A simple “Thanks” is perfectly fine.
Now, how much would you pay?
April 15th, 2015
Does Scientific Language Come Across as Wishy-Washy?
 I had the opportunity to interview author Seth Mnookin recently for a podcast on Open Forum Infectious Diseases, and it was a real treat. He’s Associate Director of the graduate program in Scientific Writing at MIT, and the author of the The Panic Virus: The True Story Behind the Vaccine-Autism Controversy.
I had the opportunity to interview author Seth Mnookin recently for a podcast on Open Forum Infectious Diseases, and it was a real treat. He’s Associate Director of the graduate program in Scientific Writing at MIT, and the author of the The Panic Virus: The True Story Behind the Vaccine-Autism Controversy.
Not surprisingly given his title, Seth thinks a lot about how language conveys information about health and science. While researching the topic of vaccine safety for his book, he discovered the striking difference in how the various sides communicated their message to the public:
When you had an NIH official or a CDC official making a statement and then you had a parent, it almost seemed to me like they were talking in two different languages … So when a doctor or Harvey Fineberg would be on TV and say, “Well based on all of the evidence that we have, we’re reasonably confident that there’s no concern that vaccines cause autism that we know of at this point, etc.” In science that means, “Yeah, we’re really sure about this.” But in English that means, “Yeah we have no idea what we’re talking about and we’re about to find out that actually we’ve been doing something horribly wrong…”
And the parents challenging vaccine safety? They couldn’t be more sure of themselves:
A great example of this is when Jenny McCarthy was on Larry King’s show and she was talking about her child, and she said, “The story that I have about my child is science.” [She also said something almost exactly like this on Oprah.] A point that I try to stress is that actually the plural of anecdote is not data, and that the fact that there is a story to be told about something does not make it true.
In research, we’re taught to be curious, questioning, and skeptical — but this doesn’t play well on the big stage. If the message is as clear as the overwhelming case for vaccine safety and efficacy, we have to just say it.
There’s more interesting stuff in the full interview, including how he chose to tackle this tricky subject, how big of a problem the hard-core anti-vaccine activists actually are right now, and when the police start to take seriously various threats on your life (not kidding about that, unfortunately).
April 8th, 2015
New HIV Treatment Guidelines, and the End of an Era
 The new Department of Health and Human Services (DHHS) HIV treatment guidelines are out, and thanks to skillful direction by Alice Pau, it’s as usual a must-read document — all 288 pages, of course!
The new Department of Health and Human Services (DHHS) HIV treatment guidelines are out, and thanks to skillful direction by Alice Pau, it’s as usual a must-read document — all 288 pages, of course!
There are several major changes, so a good place to start is the all-important “What’s New in the Guidelines” summary page. Some of the biggest modifications come in the “What to Start” section:
- There’s now a more focused list of “Recommended regimens” — it’s down to just 5. Specifically, TDF/FTC plus DTG or EVG/c or RAL (that’s 3), ABC/3TC/DTG (4), and TDF/FTC plus DRV/r (5).
- The regimens that are limited to patients with low HIV RNA are now classified either as “Alternative” — TDF/FTC/RPV — or “Other” (ABC/3TC plus EFV, ABC/3TC plus ATV/r).
- TDF/FTC plus ATV/r is now an “Alternative” regimen, largely due to the results of ACTG 5257.
- TDF/FTC/EFV is now an “Alternative” regimen, largely due to issues of tolerability.
With the caveat that as a member of the Guidelines panel, I can only give you my personal perspective (not that of the committee), here are a few comments on this last one — the demotion of efavirenz from “Recommended” to “Alternative” — which seems to me a pretty big deal.
First the good stuff about EFV, which was approved by the FDA way back in 1998:
- In clinical trials, efavirenz has been better or as good virologically than all its comparators for years and years. I still remember the shock when we learned that EFV creamed indinavir — a potent protease inhibitor, who would have predicted that? — and subsequently it won or tied in numerous head-to-head studies. That success continued until the drug was compared to integrase inhibitors (in particular dolutegravir), but note that rates of virologic failure were still just as low with EFV even in this comparison. And is there any agent that so consistently does well in patients with high baseline HIV RNA and/or low CD4?
- Efavirenz has such a long half life that regimens with the drug are remarkably forgiving, even if people forget to take it every day. It’s so forgiving, in fact, that studies suggest you can do fine taking it only 5 days a week, or at a reduced daily dose. Not that we recommend these strategies, but still — we all have patients on EFV-based regimens who admit that they skip it periodically (usually because of side effects, but that’s a different story), yet they maintain virologic control.
- Although no HIV treatment is cheap, TDF/FTC/EFV is less expensive than most of the other initial regimens we use today.
- Efavirenz (with TDF/FTC or TDF/3TC) is the default initial treatment globally, where it is widely available as a single pill taken once a day. That counts for a lot — obviously the vast majority of people with HIV in the world don’t live here.
So what’s the issue? Why then is it now an “Alternative” rather than a “Recommended” option? In my opinion, it comes down to progress we’ve made in improving side effects. Many choices are available now that are simply easier for patients — and clinicians, who can skip the time on pre-treatment education and management of tricky side effects. Specifically:
- All the clinical trials comparing EFV with integrase-based options demonstrate significantly lower rates of central nervous system (CNS) side effects with the latter. As already noted, in the head-to-head study against dolutegravir, drug discontinuations due to adverse events led to a superior result for DTG. The same thing happened when EFV was compared to RPV — in the low viral load stratum, RPV was superior because it was better tolerated.
- Virtually everyone who starts EFV gets some sort of CNS side effect of varying severity in the first week or two. Not a good idea to start the day (or even a week) before a big presentation, or travel, or some other major life event. In most patients, these CNS side effects diminish rapidly over the first few weeks of therapy. However, a minority still have some residual weirdness going on long term — dizziness, abnormal dreams, morning grogginess. Some learn to live with it and are fine, but others don’t realize how off they’ve been feeling until they stop the drug. (Brief aside — what’s up with the small fraction of patients who choose to take EFV during the day? That always perplexed me.)
- More serious CNS side effects can rarely occur, in particular depression. In this retrospective analysis of four randomized clinical trials, patients randomized to EFV-based regimens had a more than two-fold increased risk of suicide or suicidal ideation compared with those not receiving EFV. And while the absolute risk was overall low, this is a severe enough adverse effect that one should be very cautious about using the drug in anyone with a history of depression. Although observational cohort and claims data have not shown this association, remember that this is a tricky thing to find in such data, and that in clinical practice we avoid prescribing EFV to patients with psychiatric disease.
- Every ID/HIV doctor has had patients who just can’t take this drug, and it’s not from depression. OK, anecdote time — here are a few of mine: The guy who drives for a living who knew immediately he wasn’t as alert on the road taking EFV. The person whose dreams were so vivid that they were essentially indistinguishable from hallucinations (and not pleasant ones). The high-functioning scientist who simply couldn’t concentrate at work. The person (actually a few) with severe rash and fevers. Of course some of the vivid dream stories were pretty funny — my favorite was someone who dreamt that her kitchen had been extensively renovated, including specific selections of cabinets and appliances. Imagine her disappointment when she came downstairs to find the scruffy old kitchen unchanged!
Yes, I still have patients on EFV-based treatment who are doing great, and they don’t want to switch — that’s fine, no reason to do so. But the bottom line is that I haven’t prescribed TDF/FTC/EFV to a patient starting HIV therapy in nearly three years. Too many other good options out there now.
Hey, progress is a good thing!
I did this poll before — now let’s try it again, a year and a half later:
April 3rd, 2015
Melting Snow ID Link-o-Rama
 A few ID/HIV tidbits to contemplate as we go from slipping on ice and snow to dodging the mud:
A few ID/HIV tidbits to contemplate as we go from slipping on ice and snow to dodging the mud:
- Beta-lactam therapy alone is non-inferior to regimens that also cover “atypicals” for hospitalized patients with pneumonia. These results challenge a dogma that has been present for a couple of decades — namely, that all patients admitted with community-acquired pneumonia should get either a quinolone or a beta-lactam plus a macrolide. But is one study done in the Netherlands enough to change clinical practice?
- Flurry of recent papers on the cost effectiveness of HCV therapy: One, two, three, and four, to be exact. Bottom line? A huge oversimplification goes like this — from a societal perspective, the new treatments are for the most part cost-effective and expensive. And, of course, from an individual perspective — meaning you are the individual being treated, or the prescriber — they are a no-brainer.
- Related: Entertaining and informative discussion of HCV pricing, and what’s going on behind the scenes from longtime ID/HIV clinician, researcher, and educator Mike Saag. When it comes to this market, what’s the opposite of transparent? Highly recommended, especially for fans of Get Smart. And if you want some additional info on the world of “Pharmacy Benefit Managers”, read this. (Thanks to Mike for the link)
- “Fourth Generation” HIV screening tests that detect both antigen and antibody can still miss acute HIV. Remember, the duration of p24 antigen detectability during acute HIV is relatively short. Important to think about this limitation, especially when evaluating patients for PrEP — we should have a low threshold to order HIV RNA.
- The outbreak of injection drug use (IDU)-related HIV in Indiana is a stark reminder of how quickly HIV can spread with the right mix of bad ingredients — rising rates of opiate addiction, poverty, and lack of access to clean needles. Notably, in the rest of the US this mode of HIV transmission has become quite rare — here in Boston, I haven’t seen a newly acquired case of HIV from IDU in years. Bad time for complacency on this issue.
- Watch out for ciprofloxacin-resistant shigella in returning travelers. As noted in the report, “shigella is transmitted easily from person-to-person”, which is something of an understatement since some people can get sick after ingesting fewer than 100 bacteria.
- The air near beef cattle feed yards carries antibiotics, antibiotic resistance genes, and resistant bacteria. Yuck, good idea to stay up-wind. Remember, 80% of our national use of antibiotics goes to livestock. Will the programs announced this week by Obama actually reduce this use?
- I recently learned that two of the HACEK organisms have new names: Haemophilus aphrophilus is now Aggregatibacter aphrophilus, and Actinobacillus actinomycetemcomitans is now Aggregatibacter actinomycetemcomitans. Wow. The mnemonic “HACEK” still works, however, standing for Haemophilus species, Aggregatibacter species, Cardiobacterium hominis, Eikenella corrodens, and Kingella species. I’m convinced some of us chose ID as a specialty just so we could know information like this.
Hey, it’s Holy Week. Colored (sometimes green) eggs and ham! Peeps! Matzo balls and brisket! Jelly fruit slices! For those of a less traditional spiritual bent, enjoy this:
H/T to Joel Gallant for the vid.
March 28th, 2015
Quick Question: Should HIV-Negative People in Serodiscordant Relationships All Get PrEP?
 From a very thoughtful and experienced primary care provider came this query:
From a very thoughtful and experienced primary care provider came this query:
Hey Paul, quick question —
One of my patients, an HIV-negative gay man, is in a long-term relationship with one of your HIV-positive patients — my patient says his partner has been on successful HIV treatment for years. Obviously I can’t check his partner’s record to confirm this, but my patient is quite reliable and why should he be lying about this? He says they always use condoms.
He asked me today if he should go on PrEP — should he? He seems awfully low risk, denies other sexual exposures, etc.
Feel free to suggest that I send him to see you for a formal consult.
Thanks,
Roy
Unless you’ve been hiding under a rock (cold and damp down there, isn’t it?), you know by now that pre-exposure prophylaxis (PrEP) works incredibly well to prevent HIV in high risk, seronegative men who have sex with men (MSM) — even better than we thought, according to the recent PROUD and IPERGAY studies presented at CROI.
Related to my colleague’s query, note that the USA guidelines clearly state the following is an indication for PrEP in MSM:
Is in an ongoing sexual relationship with an HIV-positive male partner
So end of story — PrEP should be started, right?
But there are several reasons why it’s not quite so obvious what to do in this exact situation — which is actually quite common:
- Treatment of HIV is all but 100% effective in preventing transmission of the virus. Remember the “Swiss Statement” that condoms weren’t even required if the positive member of serodiscordant couple was virologically suppressed? The results of HPTN 052 and observational studies (most recently this one) support this prescient claim.
- Eligible participants in the MSM PrEP studies were at “high risk” for getting HIV. In IPERGAY, for example, to be eligible a person needed to report “condomless anal sex with > 2 partners within the past 6 months.” A man in a monogamous relationship with an HIV positive partner on suppressive therapy — who also uses condoms — would never have been enrolled.
- The incremental risk reduction — if any — of a man taking PrEP whose sole partner is already on suppressive ART could never be justified on a “number needed to treat” or cost-effectiveness basis. This is pretty obvious, but is worth explicitly stating, if only so that when such treatment is prescribed, we all acknowledge that it’s done for other reasons.
So what might those reasons be? First, as my friend and colleague Raphy Landovitz puts it, “people aren’t completely honest with their providers about the who’s and whats of their sexual relationships – including as it relates to condom use.” Remember HPTN 052, and those “unlinked” HIV transmissions from outside the couple? That alone should give us pause.
Second, some patients I’ve seen understandably remain very nervous about catching HIV from their partners, even if on suppressive treatment — PrEP provides them an additional layer of security. The TDF/FTC is acting here more as a benzodiazepine than an antiviral. Again, per Raphy: “It restores peace-of-mind to something that the HIV/AIDS epidemic has stolen from gay men.”
- See him (the HIV negative guy) alone. Or if he’s uncomfortable seeing his partner’s doctor, offer to have him see one of my colleagues.
- Reassure him that the discussion is 100% confidential.
- Tell him the pros and cons of PrEP. Efficacy, safety, and cost, of course, but also the characteristics of the patients in the studies — that they were high-risk HIV negative gay men.
- Inform him that PrEP has never been explicitly tested in the HIV negative partners of people on suppressive ART in a monogamous relationship — and likely never will be since the risk of transmission is already so low.
- Let him decide.
In my anecdotal experience thus far, some have chosen to go on PrEP, and some haven’t.
And whether those who opted in did so because they’re actually at higher risk than they’re disclosing, or for peace of mind, or some combination — does it really matter?
March 21st, 2015
ID Learning Unit: Coagulase-Negative Staph, and the “Anti-Zebra” Residents’ Report
 At the risk of betraying a deep streak of nerdiness, I confess to being a huge fan of Residents’ Report. This infatuation goes back to my medical student days, when the occasional chance to watch the Chief Medical Resident — who seemed the smartest doctor on the planet — lead a discussion of an interesting case inspired all kinds of aspirations.
At the risk of betraying a deep streak of nerdiness, I confess to being a huge fan of Residents’ Report. This infatuation goes back to my medical student days, when the occasional chance to watch the Chief Medical Resident — who seemed the smartest doctor on the planet — lead a discussion of an interesting case inspired all kinds of aspirations.
Alas, I was never chosen to be Chief Resident, but have been lucky enough to sit in on my fair share of Residents’ Reports over the years, including one this past week. And so glad I did, as current Chief Resident Mary Montgomery tried a new twist on the genre: Instead of presenting a fascinating rare case — a “zebra” — or a challenging ongoing diagnostic dilemma, she chose a couple of extremely non-zebroid (that’s a word) cases that involved coagulase-negative staph (CoNS), a bug that frankly most of us think is pretty ho-hum.
But you know what? It was a great report, educational and entertaining, and here’s what we learned about this commonly encountered (but frequently challenging) entity:
- In the microbiology lab, a coagulase test is done on suspected staph isolates, looking for tell-tale clumping of plasma. Clumps = coagulase-positive (Staph aureus); no clumps = coagulase-negative. Watch!
- There are over 30 species of CoNS, with Staph epidermidis the most common — but you rarely see micro reports listing Staph epidermidis, since identifying the particular CoNS species is rarely helpful.
- Staph saprophyticus is a CoNS species that is the second most common cause of uncomplicated UTIs in young women. Fortunately, it’s sensitive to most antibiotics used to treat UTIs.
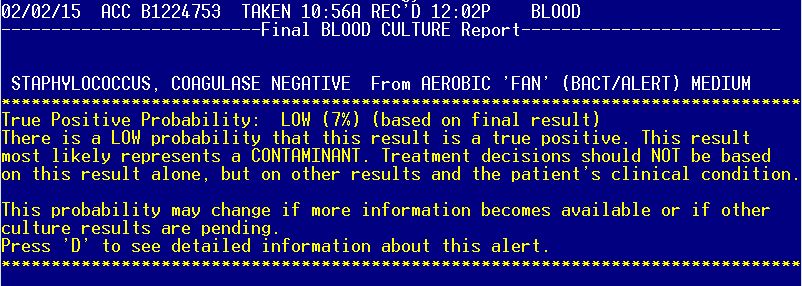
- CoNS are the most common isolates from blood cultures, and also the most common contaminants. Distinguishing true- from false-positive blood cultures can be tricky, in particular with CoNS, and this home-grown study provides some guidance — indeed, it’s incorporated into our ancient electronic medical record. (See above image — soon to be retired, alas, in a move of EPIC proportions.) Question: Has this study been updated by anyone?
- Clinically important infections with CoNS frequently involve prosthetic joints, mechanical heart valves, indwelling vascular catheters, ventricular shunts, vascular grafts, pacemaker or defibrillator leads, orthopedic hardware — in short, artificial ingredients!
- Treatment of choice for CoNS infection acquired in the hospital is vancomycin, since more than 80% are resistant to beta lactam antibiotics.
- CoNS are good at sticking to things, and have a virulence factor called arginine catabolic mobile element (ACME), which they unfortunately sometimes decide to transfer to MRSA. I hate when they do that.
- Production of biofilms — slime, think of the stuff that makes rocks slippery in a stream — makes CoNS difficult to clear from prosthetic material. Here’s a whole book about biofilms, great for leisure reading.
- Among antibiotics, rifampin seems to be the best at penetrating biofilms, hence its use as adjunctive therapy for many infections involving prosthetic material.
- Around 8% of native valve endocarditis is due to CoNS, and these patients have a high likelihood of requiring surgery. In my anecdotal experience they have an extremely indolent course, but not when the CoNS is Staph lugdunensis.
- Speaking of, Staph lugdunensis is a particularly aggressive form of CoNS, a wolf in sheep’s clothing that acts much more like Staph aureus than its wimpy coagulase negative brethren. It’s usually sensitive to beta lactams, too.
Of course I could go on and on about this last bug — we ID doctors adore Staph lugdunensis, which is both fun to say and is one of those factoids that separates us from the mere mortals out there who can’t be bothered to remember this arcane stuff.
Here’s a tip for you non-ID doctors: You can really impress your ID specialist friends by bringing up Staph lugdunensis when discussing a case, or even just in casual conversation:
Non-ID doctor: Hey, have you watched the new House of Cards season yet?
ID doctor: No, am waiting until I have time to binge-watch it.
Non-ID doctor: Makes sense. By the way, Staph lugdunensis.
ID doctor: Impressive!
Yes, I know. Time to get a life.
March 8th, 2015
Measles Vaccine Videos and the Challenge of Changing Someone’s Mind
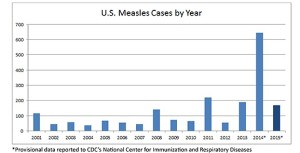 I suspect most of you have already been treated to this highly amusing video about the measles outbreak from Jimmy Kimmel — a comedy segment featuring real-life doctors, imagine that. Not your typical late-night comedy show performers, but they forcefully (and obscenely) get their message across.
I suspect most of you have already been treated to this highly amusing video about the measles outbreak from Jimmy Kimmel — a comedy segment featuring real-life doctors, imagine that. Not your typical late-night comedy show performers, but they forcefully (and obscenely) get their message across.
If you have just returned from a tropical island where the internet connection was iffy, however, here it is for your entertainment:
Probably fewer of you saw this next one, which is quite well done and pretty accurate scientifically. It also differs dramatically in tone:
My question for you: Which one is more likely to change the views of a person with an anti-vaccine stance, and why?
March 1st, 2015
Really Rapid Review — CROI 2015, Seattle
 For the 3rd time in its illustrious history, the Conference on Retroviruses and Opportunistic Infections (CROI) returned to Seattle this past week for it’s 22nd meeting. For those of us living in the North Pole, 50 degrees and drizzle never felt so wonderful!
For the 3rd time in its illustrious history, the Conference on Retroviruses and Opportunistic Infections (CROI) returned to Seattle this past week for it’s 22nd meeting. For those of us living in the North Pole, 50 degrees and drizzle never felt so wonderful!
(See image below for graphic representation — that’s my dog Louie wondering what happened to his world. Click on image for full impact.)
With 4000 attendees (capped at that number to keep it relatively “intimate”) and almost half of them from non-U.S. countries, CROI remains a dynamic, incredibly interesting meeting — in my opinion our very best HIV research gathering, guaranteed to make you sleepless while trying to cover it all. (Good thing we were in Seattle.) Where else can we get clinical, basic, translational, and behavioral researchers all together?
So on we go to a summary, a Really Rapid Review™ of some of the most interesting studies at the conference (at least from one perspective). Links are to the conference website (excellent this year), abstract #’s in brackets, and many of the oral presentations are available for webcast here. List is organized roughly by prevention, treatment, complications, cure, and miscellaneous cool stuff; please list in the comments any important studies I’ve missed!
- In a “real world” clinical trial called PROUD [22LB], pre-exposure prophylaxis (PrEP) with TDF/FTC in high risk gay men in London reduced HIV transmissions 86%. Real world” since the participants knew if they were receiving active drug or not (randomized to start right away or delay 12 months); the delayed PrEP arm extensively used PEP, making the results even more impressive. Study stopped early due to efficacy.
- As we heard in October, the IPERGAY (ha) study compared intermittent PrEP — two TDF/FTC’s before sex, one pill the next 2 days — to placebo, and was also stopped early. Efficacy of this “on demand” PreP? Again 86% [23LB]. Note that in both of these studies, incidence of HIV and protective efficacy of PrEP were higher than expected.
- More on PrEP: With evidence that risk of HIV transmission persists 6 months into ART [989], a program for discordant couples to provide PrEP for 6 months and ART to the person with HIV simultaneously makes a lot of sense — which is what they’re now doing for heterosexual couples in this program in Uganda [24].
- Here’s another study with zero transmissions in serodiscord
 ant couples not using condoms when the infected partner is on suppressive ART [1019LB]. Perhaps eventually someone will report another case of HIV transmission in this setting, but it’s obviously pretty darn rare.
ant couples not using condoms when the infected partner is on suppressive ART [1019LB]. Perhaps eventually someone will report another case of HIV transmission in this setting, but it’s obviously pretty darn rare. - In the PROMISE study of prevention of mother-to-child transmission [31LB], TDF/FTC was associated with a significantly higher risk of neonatal death or very pre-term labor than ZDV/3TC. (Both were given with LPV/r.). Results unexplained — and reinforce that there still isn’t a perfect treatment for pregnant women with HIV.
- Infant outcome data from this observational study in Botswana from over 1000 pregnant women receiving TDF/FTC/EFV during pregnancy are quite reassuring [878]. Could this ironically turn out to be safer than TDF/FTC + boosted PIs?
- Now for post-exposure prophylaxis (PEP): In this Australian study [958], TDF/FTC/RPV for non-occupational PEP was safe and well tolerated, with excellent adherence. I’ve never used it for this purpose, but it makes a lot of sense — one prescription, one pill, rare severe adverse events, relatively low cost.
- More on non-occupational PEP [961]: Beware unrecognized acute HIV infection in these very high risk individuals, which presents several management challenges — especially after PEP is started. And they call it “PEPSE” (post-exposure prophylaxis after sexual exposure) in Britain — rhymes with the soft drink.
- Phenomenally good news about occupational transmission of HIV in the United States [1027], which has become vanishingly rare — only one case since 1999!
- Late diagnosis of HIV — meaning when a person already has AIDS — is down significantly here, but still occurs in 1 out of 5 new diagnoses. Check out the wide variation based on region [999].
- Interesting survey on how often HIV tests are done at visits to U.S. doctors’ offices. Guess what, it’s done very infrequently: 0.7% of visits [1082]. One tough question — given the wide variation in HIV prevalence, what is the right number?
- On the laboratory side, this is how HIV testing should be done [621]: 4th Generation antibody/antigen screen, then confirmation using a newer HIV-1/HIV-2 differentiation assay called “Geenius.” And no Western blot!
- HPTN 065 [29] is a fascinating (and long-awaited) study of the effect of financial incentives on linkage to care, virologic suppression rates, and continuity of care. Initial linkage and virologic suppression overall weren’t better with the money, but the financial incentives did improve treatment outcomes in the smallest sites and those with the lowest baseline suppression rates. Continuity also improved. Seems this should be a targeted intervention for our most difficult patients, right? The Freakonomics people would love this one.
- TEMPRANO was an incredibly ambitious, important study done in the Cote d’Ivoire testing two interventions in a factorial design: Immediate vs WHO-recommended ART and 6 months of isoniazid preventive therapy (IPT) vs none [115LB]. Both the immediate ART and the IPT significantly improved outcomes, and the former even did so for those with CD4 cell counts >500. Seems we’re just now waiting on the START study results …
- 3TC and FTC are often used interchangeably, but they are not quite the same drugs. In this analysis from the Netherlands [566], the nod goes to FTC, especially in NNRTI containing regimens.
- Wouldn’t it be great if you could objectively assess adherence in your patients with low-level viremia? This clever study [117] found that untimed drug levels strongly predicted the subsequent risk of virologic failure.
- A single-tablet regimen containing elvitegravir, cobicistat, and FTC, and tenofovir alafenamide (TAF) was noninferior to one containing TDF [113LB], with less effect on kidney function and bone [143LB]. (Disclosure: I was the presenting investigator on the latter study.) Seem likely that these safety benefits will play out to be meaningful in long-term treatment, and in those with risk factors for renal disease right now. The TAF regimen is currently under review by the FDA.
- Here’s another study showing that in second-line therapy, those with more resistance at baseline “paradoxically” have better virologic outcomes than patients with less. Lessons: 1) adherence matters A LOT; 2) NRTIs retain activity even with resistance; and 3) our resistance algorithms derived in the 1990s are lousy.
- The LATTE study [554LB] looks at oral cabotegravir plus rilpivirine as a maintenance strategy, mostly in anticipation of these two being used as long-active injectable agents. Since the last presentation, the 96-week data show this is still performing as well as EFV-based standard treatment. But in a glass half full/half empty result, two additional patients have failed, both with NNRTI resistance. (The first failure had both integrase and NNRTI resistance.)
- Remember the maturation inhibitor bevirimat (R.I.P.)? The second generation compound BMS-955176 looks much more promising [114LB], with retained activity even against viruses with baseline gag polymorphisms (the Achilles’ heel of bevirimat).
- If you’re using dolutegravir after failure of raltegravir or elvitegravir, resistance at Q148 plus two other mutations will significantly reduce DTG activity[609]. Otherwise the drug should be active.
- Is the risk of endstage liver disease in HIV/HCV coinfection reduced in the current ART era? Unfortunately no, says this Canadian analysis, making treatment of HCV in this population still critically important [638].
- In the ION-4 study for HCV genotype 1 or 4, sofosbuvir/ledipasvir for 12 weeks had a 96% HCV cure rate. The study included some very treatment-experienced patients and 20% overall had cirrhosis [152LB]. The one baseline characteristic predicting treatment failure was black race, many of whom were receiving TDF/FTC/EFV — raising questions about a possible pharmocogenomic issue leading to the interaction.
- Adding SOF/LDV to a TDF/FTC, boosted PI containing regimen increases TDF levels by 30-60%[82]. If there are baseline renal issues, probably best to switch ART before starting this HCV treatment if possible — and if not, either use a different HCV therapy (the pariteprevir/ombitasvir/etc combo if on ATV/r, or one of the few remaining indications for pegIF/RBV + SOF), or monitor renal function closely.
- In the ALLY-2 study for HCV (any genotype), sofosbuvir plus daclatasvir for 12 weeks cured 97% of coinfected study subjects, treatment naive or experienced [151LB]. An 8-week course in treatment naives was less effective (76% cure). Daclatasvir (an NS5A inhibitor) is currently under review by the FDA.
- Here’s a surprising but important negative study result: body composition (in particular regional fat gain) was not significantly different between raltegravir, atazanavir/r, and darunavir/r-based regimens [140]. Lipoatrophy may be rare, but fat accumulation (especially visceral) remains a common problem, one that discouragingly cannot be directly ascribed to any specific medication or drug class. And note that both this study and the next one on rosuvastatin were led by Grace McComsey from Case Western, clearly one of the field’s best clinical researchers.
- Rosuvastatin slows progression of carotid intima media thickness [137] and atorvastatin reduces non-calcified coronary artery plaque volume [136]. Large study of pitavastatin in HIV infected patients who otherwise wouldn’t qualify for statin therapy due to start soon.
- If you thought the NA-ACCORD analysis of abacavir and cardiovascular risk [749LB] would settle the issue of whether the drug leads to increased cardiovascular risk, no such luck: Some of the study’s analyses showed a significant association between abacavir and MI, others did not. I was reluctant to use the drug in patients with high CV risk before CROI 2015, and still am.
- Cumulative exposure to tenofovir — and even more so atazanavir — increases the risk of chronic kidney disease [142]. Suspect the latter is not well known to many HIV clinicians, but this is not the first time atazanavir has been implicated.
- More on the renal and bone safety of TAF [795]: Patients with mild-moderate renal disease (estimated GFR 30-69) who were switched to “ECF-TAF” had stable renal function, improvement in urinary protein, and an increase in bone mineral density. Note that these are exactly the kinds of patients for whom TDF and ABC treatment are currently problematic, as they may have both renal disease and CV risk factors.
- Respiratory isolation in possible TB cases in the USA is a huge pain — it makes care more difficulty, delays discharges, and is certainly no fun for the patient and providers. And of course the vast majority don’t have TB. In this important study [824], two Xpert tests ruled out active TB as effectively as 3 sputum smears. Note that the test just got approval for this indication — hope our hospital adopts this testing soon!
- It’s not a randomized clinical trial, but this systematic review [837] found no evidence that early ART worsens outcome of cryptococcal meningitis in high income settings.
- And while we’re on the topic of cryptococcal meningitis, how about a little sertraline, which seems to speed fungal clearance? Folks, we have a winner of of this year’s most surprising “off target effect” [838].
- Next to some cure studies: A toll-like receptor 7 agonist given to SIV-infected monkeys on suppressive ART did two things: 1) triggered easily measurable viral “blips”; 2) lowered SIV setpoint after stopping ART compared to monkeys receiving placebo [108]. Could this be a treatment that both stimulates and reduces the viral reservoir?
- The zinc finger nuclease approach to modifying CD4 cells is making slow progress — now with cyclophosphamide to enhance engraftment [434].
- Here’s a detailed virologic analysis of a patient who experienced virologic rebound after stem cell transplantation from a CCR5 negative donor. Appears there was pre-existing X4 using virus, which was “selected” by the CCR5 negative cells [431]. Original case reported here. This report states that there have now been 7 attempts to cure HIV via this approach, and obviously thus far only one success. Tough work.
- Some excellent plenaries (among those that I saw): Raphy Landovitz on PrEP (with very nifty PowerPoint skills), Steve Grinspoon on cardiovascular disease, Rick Elion on treatment as prevention, and David Cooper on the history of HIV treatment.
Now, about Seattle. I first visited this city in the early 1980s, and it has of course boomed since then, with many more sensational restaurants, high-rises, more traffic, hipsters (though increasingly priced out of living there), and encouragingly much greater access to it’s beautiful waterfront. A spectacular city, with a terrific convention center.
And it’s of course the home of Boeing, Microsoft — Bill Gates gave a talk at CROI in 2002 — and Starbucks, and if if you’re used to the generic Starbucks on your street corner, in your strip mall, or in your hotel lobby, they have some Starbucks in Seattle that look like coffee museums.
We’ll see you next year in Boston, my home town. And let the record show that there has never been a CROI in Boston that was in any serious way hampered by the weather.
Fingers (numb though they might be) crossed.