An ongoing dialogue on HIV/AIDS, infectious diseases,
February 21st, 2015
Fusobacterium, Pharyngitis, and the Limits of Limiting Antibiotics
 A paper on pharyngitis in young adults, just published in the Annals of Internal Medicine, is creating a controversy in the intersecting worlds of primary care and Infectious Diseases. The first author is Robert Centor, of the famous Centor criteria that assess the likelihood of group A strep. He’s been writing about our need to expand diagnostic considerations in sore throat for several years, starting with this excellent editorial.
A paper on pharyngitis in young adults, just published in the Annals of Internal Medicine, is creating a controversy in the intersecting worlds of primary care and Infectious Diseases. The first author is Robert Centor, of the famous Centor criteria that assess the likelihood of group A strep. He’s been writing about our need to expand diagnostic considerations in sore throat for several years, starting with this excellent editorial.
The Physician’s First Watch summary of the new paper was spot-on, so I’ll just quote them here (bolding mine):
Some 310 young adults (aged 15–30) presenting with pharyngitis at an Alabama university clinic underwent polymerase chain reaction testing for bacteria in throat swab specimens; 180 asymptomatic students were also tested. Fusobacterium necrophorum was identified in 21% of patients with pharyngitis (and 9% of asymptomatic students), while group A streptococcus was found in just 10% of patients (and 1% of asymptomatic students). Clinical presentations were similar for F. necrophorum and group A strep.
From the perspective of patient management, there are two interpretations circulating about this paper — one that it encourages antibiotic prescribing, the other that it does no such thing.
The controversy is nicely encapsulated in this comment on a listerv (remember those?) for pediatricians, which was shared with me from a very reliable source (she didn’t write the comment):
OMG! So if it is cultured [sic] from the throat, it is the cause of the infection,right? So now everyone who has this in their throat and doesn’t feel well needs antibiotics, right?
Allow me to take both positions:
Pro Antibiotics: Some really terrible exudative pharyngitis in young adults is group A strep negative. This study shows that fusobacterium is more common than strep in this age group. We know it can cause peritonsillar abscess and, even worse, septic jugular vein thrombophlebitis (Lemierre’s syndrome), both of which are preceded by sore throat — and both of which are more common than acute rheumatic fever. If we treat the really sick teenager and young adults who are group A strep negative with an antibiotic with activity against fusobacterium — penicillin and other beta lactams, please, not azithromycin — not only will these youngsters get better faster, but we can prevent potentially life threatening complications.
Versus:
Anti Antibiotics: Most pharyngitis is causes by respiratory viruses. There is no way to detect fusobacterium as a cause of pharyngitis in clinical practice, so if most cases get treated “empirically”, this will be massive unnecessary treatment. Detection of the organism by polymerase chain reaction in the study does not prove that fusobacterium is the cause of the pharyngitis, especially since it’s found in a not insignificant proportion of asymptomatic individuals (9%). There is furthermore no proof that treatment of fusobacterium will hasten symptom improvement or, more importantly, prevent Lemierre’s.
The latter position was nicely articulated in an accompanying editorial in the Annals written by my colleague Jeffrey Linder — a primary care physician who has published extensively on this subject and admittedly a much more reliable expert on the topic than I.
But let me risk taking a position slightly different from Jeff and, I’m sure, many of my ID brethren, one that I confess is rooted not so much in data but in experience caring for several young adults with Lemierre’s. Importantly, Jeff and I don’t disagree — it’s more a matter of emphasis.
Remember this — patients with Lemierre’s are often critically ill. They frequently require ICU care, have high spiking fevers with staggeringly high white blood cell counts, and invariably have multiple septic pulmonary emboli with potentially other metastatic sites of infection, including the brain.
It’s a terrifying illness — these are most commonly previously healthy high school and college-age kids, so the stakes are high. No, we don’t know that treatment of severe pharyngitis “caused” by fusobacterium will prevent Lemierre’s, but doesn’t that make biologic sense?
So let’s go with the pediatricians’ common-sense approach to clinical care, and make a decision about antibiotics based on that sixth sense of “is the kid really sick?” If so, go with some penicillin — especially if at the first encounter they didn’t get treated, and then they come back a few days later even worse.
Or, if you prefer, listen to the guru of pharyngitis himself, Dr. Centor, and his interpretation of national guidelines:
We believe that following the American College of Physicians/Centers for Disease Control and Prevention guidelines endorsed by the American Academy of Family Physicians would decrease the risk of Lemierre syndrome in adolescents and young adults. Using these guidelines, physicians can choose to prescribe antibiotics for patients with a pharyngitis score of 3 or 4 (three or four of the following: fever, absence of cough, tender anterior cervical lymph nodes, tonsillar exudate).
Makes sense to me.
February 15th, 2015
Should Antibiotics be Part of End-of-Life Care?
There’s been some truly outstanding work done recently on end-of-life care, and how we deal with it — or more accurately, how we typically don’t deal with it until the very last moment, at which time often many unfortunate decisions and events occur. Here are three I can strongly recommend:
- Roz Chast’s Can’t We Talk About Something More Pleasant? is probably the most widely read book among my circle of friends right now, as many of us have parents of a certain age. Chast is a cartoonist best known for her distinctive squiggly cartoons in the The New Yorker — here’s one of my favorites — and is already familiar to many ID doctors because of her morbid fascination with dreadful diseases, some of them infections. But this extended memoir about her aging parents is a remarkably ambitious book, by turns funny (of course), moving, and ultimately heartbreaking, especially when touching on the fraught relationship she had with her mother.
- If drawings aren’t your thing, then give Atul Gawande’s Being Mortal a shot. In his usual clear prose — which miraculously reads neither overly technical to the lay public or overly simple to health care providers — he deftly lays out what many of the challenges are in the care of both the elderly and the terminally ill. For example, how can we negotiate the conflict between personal freedom versus safety in our loved ones who have such a limited time to live? If 90-year-old Uncle Milton with severe congestive heart failure wants to eat pickles, but pickles contain too much salt for his diet, should we stop him? The recent Frontline about Atul (we’re on a first name basis, brush with greatness) and his book make me hope that his sensible voice will lead to progress in this difficult part of health care.
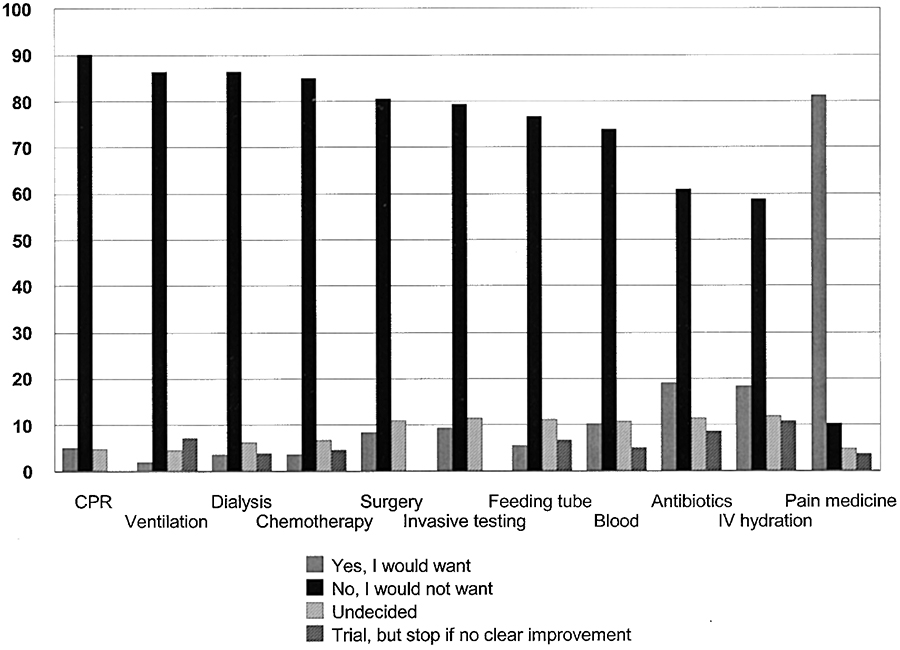
- Finally, if you’re looking for a terrific podcast, check out this Radiolab piece called Dead Reckoning. The first part is about surviving rabies — good stuff for ID doctors, and yes, we’re that bizarre — but the piece finishes in more familiar territory, dealing with medical options at the end of life. In a section called “The Bitter End”, it cites a now famous study done of Hopkins med school graduates, demonstrating that doctors say they would forego end-of-life treatments if they had an incurable brain disease (something akin to dementia) — a big contrast with the people interviewed on the street, most of whom want all this stuff. The end-of-life treatments these doctors considered are shown in the figure below:
Note the ninth one on this list — antibiotics — and consider a scenario that no doubt will be familiar to doctors and nurses the world over, and not just to ID doctors: The patient who has metastatic cancer, or advanced dementia, or irreversible advanced heart or lung disease, and the decision has been made to withhold CPR, mechanical ventilation, tube feeding, and dialysis.
But antibiotics? They often remain an option to the very end, frequently in the face of other conditions with terrible prognoses and little chance for reversal. Those recurrent urinary tract infections, aspiration pneumonias, infected pressure sores, and other indignities of our failing bodies can be treated with antibiotics (though with progressively less effect) — but to what end?
So read the case, take the poll, then listen to the Radiolab piece.
A 94-year-old woman with advanced dementia is referred to the hospital from her nursing home because of fever and a change in mental status. At baseline, she can sit in a chair but cannot walk, feed, or bathe herself; she can respond to simple questions, but has little spontaneous speech. She has an existing DNR order — no CPR or intubation. There have been two admissions to the hospital over the past six months (pneumonia, urinary tract infection), after which she returned to the nursing home. In the emergency room, her evaluation is notable for a fever and somnolence. The urinalysis shows 50-100 WBC. The health care proxy, who lives in another state, is unavailable.
February 8th, 2015
Snowstorms-a-Plenty ID Link-o-Rama
 A few items to discuss as we settle in for yet another Boston megastorm:
A few items to discuss as we settle in for yet another Boston megastorm:
- The measles outbreak continues to bring forth excellent commentaries on the selfishness of vaccine-refusers, with this one from Frank Bruni one of my recent favorites. Question: Will it take a hospitalization — or even worse, a death — of an American child with measles to stop this ridiculousness?
- This piece in the Wall Street Journal describes the negotiations going on behind the scenes between pharmaceutical companies and payers regarding HCV therapy. I’m sure something like this has happened before in non-ID fields (Oncology or Rheumatology would be my best bet), but I have never experienced anything like this as an ID doctor — meaning, both the clinician and the patient seem to be completely left out of the discussion. Hello? Can anyone hear us?
- Can a fecal microbiota transplant from an overweight donor lead to obesity in the recipient? That’s the implication in a case report over in Open Forum infectious Diseases. While the case does not prove causality (other factors could have contributed to the weight gain), the plausibility of the FMT leading to obesity is at the very least suggested in the clinical course and supported by animal data where indeed the microbiome plays a major role in metabolism. Don’t miss this excellent editorial from real experts in the field.
- More evidence that booster vaccines for hepatitis B are probably not needed, at least according to a study in health care workers. It’s that “long-lasting amnestic response” — meaning even when antibodies decline, exposure to the antigen is rapid and protective. The hepatitis B vaccine was an extraordinary and unheralded major advance in safety for healthcare workers.
- There are lots and lots of strange bacteria in the NYC subway, says this fascinating, much-publicized and (let’s face it) extremely unsurprising report published in Cell. Best part: “Almost half of all DNA present on the subway’s surfaces matches no known organism.” If I might make a personal comment: when my family moved to New York City in the 1970s, there were no doubt even more bizarre microbes living down there. Anyone have a spare autoclave?
- The coformulations of atazanavir/cobicistat and darunavir/cobicistat are now available. Definitely more convenient to have them together (avoiding selective skipping of ritonavir), and if they’re price-equivalent to the separate dosing of the drugs, then they eventually will be widely adopted. Otherwise — and especially with the approval of generic ritonavir — they could face a tricky pharmacoeconomic challenge. Now throw in 300 mg of lamivudine and pull of a GARDEL study equivalent, now that could be transformative.
- Wonderful “Call to Arms” about the crisis facing Infectious Diseases by Ron Nahass, who in our field is something of a true visionary: He understands — and fortunately can communicate — the value of ID doctors independent of billing units in a fee-for-service environment. Required reading for the gloomy ID doc (and there are lots of us out there). My favorite line: “Develop a true value of our intellectual capital.” In other words, get paid for being smart, not for doing a procedure.
- Being cold could increase the chances of catching a cold. Score one for common wisdom!
As the latest storm intensifies up here in Boston, it’s worth disabusing the world at large of the perception that the whole Northeastern United States has the same weather. Today the high temperature in Washington DC was 68 — yes, you read that right — Philadelphia had high 40s and obviously no snow, and New York (funky subway bacteria notwithstanding) had a dreary but otherwise very manageable winter day.
Here, it’s 15 degrees, and 12-18 inches of snow are expected over the next 24 hours.
Speaking of snow — here’s something to do in your spare time:
January 28th, 2015
Quick Question: Should We Still Be Recommending This Year’s Flu Vaccine?
From a football-obsessed primary care provider, written to me on one very snowy day in New England:
Hi Paul,
I’ve been reading about this year’s flu vaccine, and how ineffective it is. Not surprisingly, my patients have been hearing this too, and it has only increased their reluctance to go through with it. Should I just cut my losses and stop recommending it this year? Seems we have much more important things to worry about, such as measles in Disney and deflated footballs.
Go Pats!
Kerry
p.s. I think the Pats are really geniuses. And they realized that if they pump the balls to 11.5 PSI right before the game, then heat them (microwave? hair dryer? ) to get up to 12.8 PSI, then hand to the refs who measure at at least 12.5 PSI, then let them cool down for a while. And, as with taxes, if it doesn’t say you can’t do it, then you can do it. Genius.
Dear Kerry,
The quick answer is yes, we should still be recommending it, but I share your pain. (I mean about the flu vaccine, not about Deflategate.) My experience this year is that when I suggest a flu vaccine, my reluctant patients not only decline, but look at me as if I’ve recommended that they undergo a colonoscopy without sedation. You must be kidding me, everyone knows this year’s vaccine is a dog.
 So why recommend it? First, it still works some of the time, even if the H3N2 match isn’t good (there are influenza B strains as well that are included in the vaccine). 23% effective is better than nothing, which means that these 23% not only won’t get sick with flu themselves, but they won’t spread it to the people who are the most vulnerable (the very young, the elderly, and pregnant women).
So why recommend it? First, it still works some of the time, even if the H3N2 match isn’t good (there are influenza B strains as well that are included in the vaccine). 23% effective is better than nothing, which means that these 23% not only won’t get sick with flu themselves, but they won’t spread it to the people who are the most vulnerable (the very young, the elderly, and pregnant women).
Second, there’s really nothing else out there that works, unless you want to take oseltamivir continuously, all flu season — this is not recommended, and would be very expensive. I suppose our patients could seal themselves off in a polyurethane bubble until Spring — which would be particularly difficult if they like to ski.
Third, there’s at least a little evidence that even if the flu vaccine doesn’t work, it might attenuate the severity of clinical influenza, reducing the risk of pneumonia and hospitalization. As an optimist, I plan to believe this last item until someone proves it’s not true.
Your email also gives me a chance to link a truly outstanding review over on Medscape called, Why is Influenza So Difficult to Prevent and Treat? It’s an interview with two experts in the field, Drs. Andrew Pavia and Gregory Poland, and really the title should have been expanded to “Why is Influenza So Difficult to Predict, Prevent, and Treat?” I always get asked about the upcoming flu season by my friends, and the honest answer is — WE HAVE NO CLUE.
The Medscape piece is top-notch, a very readable update on these issues. I learned a lot about this tricky infection, including the key fact that if we delayed choosing the strain for next year’s vaccine for a few months, we’d probably have a better vaccine match from year-to-year. Plus I was introduced to the seat belts analogy, which goes like this: “Seat belts may not protect from high-speed crashes all the time, but some protection is better than none.” Exactly!
So go ahead and continue to recommend it. I find that if my patients balk, I don’t push it, but better to have a uniform medical position on flu vaccine than to waffle.
And about that game on Sunday — 20 days until pitchers and catchers report for Spring Training.
January 21st, 2015
No Response
 Not surprisingly, it’s a sad, sad day at the Brigham. Yesterday a man walked into the hospital and shot one of our cardiac surgeons, then shot himself. Both died.
Not surprisingly, it’s a sad, sad day at the Brigham. Yesterday a man walked into the hospital and shot one of our cardiac surgeons, then shot himself. Both died.
Amidst the grief, horror, and shock that we all are feeling, I was also reminded of the year I spent working in England before going to medical school. Somewhat to my surprise, I found myself frequently defending our country against the numerous criticisms directed at the United States by my (mostly) good-natured English colleagues and friends.
Many of the critiques centered around food and drink — but not all.
- “Sax [last name a sign of affection, very Public School], how could you Yanks eat that vile peanut butter [or beef jerky, or Velveeta Cheese, or corn dog, or crispy bacon]?
Response: Hey, some of those things are great — I love peanut butter, and bet you would too if you tried it. And as for our crispy bacon, it’s way superior to the greasy soft stuff you guys serve with breakfast. And don’t get me started on marmite — disgusting. - “Sax, seems like America is a vast place, vast in both landscape and human girth. Is it because everyone eats at McDonald’s every day? I guess your only monarch is Burger King.”
Response: My apologies for McDonald’s (which, for the record, seems to have caught on quite nicely in your country too), but you must understand that American cuisine is as varied as our waistlines. - “Sax, why does American beer look, smell, and taste like watered-down piss?”
Response: Why does British beer smell and taste like wet shoes? Warm wet shoes, no less. - “Sax, how can you live in a country so barbaric, so uncivilised, that any madman can get a gun and go out and shoot someone?”
No response.
Just sadness.
January 18th, 2015
Opposition to HCV Screening Raises a Few Interesting Points — But Has Some Really Wacky “Facts”
 Over in the British Medical Journal, there’s a provocative editorial entitled, “Is widespread screening for hepatitis C justified?”
Over in the British Medical Journal, there’s a provocative editorial entitled, “Is widespread screening for hepatitis C justified?”
Based on the title alone, you can guess the authors’ answer to that question — a resounding “No!”
By taking this position, of course, they are opposing some very data-driven and well-respected arbiters of policy and clinical practice. These include not only the Centers for Disease Control — which started recommending universal screening in 2012 to people born between 1945–1965 (the years of peak incidence) — as well as the World Health Organization, and, for good measure, those staggeringly data-driven folks from the U.S. Preventive Services Task Force (USPSTF).
Remember, these USPSTF guys are a scrupulous bunch, opposing many forms of screening for insufficient evidence. Just the very fact that they endorse HCV screening is almost reason enough to accept it as worthwhile. Indeed, they reversed their earlier opposition to HCV screening with their latest review — and did so even before interferon-free therapies became standard of care!
(Why is it so hard to say and write that combination of letters? — “USPSTF” reminds me of the confirmation codes that the airlines use for flights.)
The key points of the of the BMJ opinion piece go like this, roughly in order:
- The natural history of hepatitis C suggests it is generally benign.
- Achieving a “sustained virology response,” or SVR, is only a surrogate marker for the important clinical endpoint of liver disease. Proof: Some people who achieve SVR still go on to have decompensated disease and hepatocellular carcinoma.
- SVR does not mean HCV is cured anyway.
- Screening will be dangerous because the treatment could be more harmful than the disease; we also need long-term safety data on the newer drugs.
- Before we adopt widespread HCV screening, a large randomized trial should be done comparing broad to risk-based screening, with clinical outcomes as the primary endpoint.
There’s always room for some dialogue in any policy statement, and the editorial does raise some important points.
But let’s take these above positions one at a time:
- Most people with HCV will never develop clinically significant liver disease. Yes, this is true, but HCV is still the leading single cause of end-stage liver disease leading to liver transplantation in the USA; HCV can furthermore cause numerous non-hepatic complications; and a chronic infection with high rates of ongoing replication is probably bad for general health, which almost certainly accounts for the higher rates of fatigue, nausea, pain, and decreased quality of life in those with HCV versus those without.
- SVR is only a surrogate marker. If you’re a real skeptic, you’d argue that the better clinical outcomes observed in patients who achieve SVR versus those that don’t might be confounded by their better health at baseline. On the other hand, many believe that the benefits of SVR have been convincingly shown through clinical cohorts, adjustment of baseline characteristics, and improvement in liver histology among those who achieve SVR. And what about those patients with SVR who still get liver-related illness? Most had advanced liver disease before they were treated — one could argue that if they’d been diagnosed decades earlier and cured, their liver disease never would have happened.
- “Sustained virological response is not a cure,“ writes the paper confidently. This is certainly a minority view, and seems to be based on the existence of case reports of late relapses, with a frequency of no greater than 3% (and probably lower). Isn’t the very existence of these papers good evidence that most of the time SVR is a cure? Why would any of them be published unless they were exceedingly rare events?
- Treatment is harmful — in most patients, more harmful than the disease. For currently relevant treatments, they cite this paper, where “3% of participants taking sofosbuvir experienced serious adverse events compared with 1% in the peginterferon plus ribavirin arm.” But these data are for any serious adverse event, not just those that are drug-related. Bad things can happen to patients who are in clinical trials, especially trials that include patients with chronic diseases — it doesn’t mean the drugs caused them. In trials of newer HCV drugs, especially those that don’t include interferon or ribavirin, serious adverse events that are conclusively drug-related are extraordinarily rare. And one last thing: No review of HCV therapy today should list side effects of telaprevir or boceprevir as a reason for avoiding treatment (both are cited). These drugs are no longer recommended — and the former isn’t even available. Even interferon is rarely indicated today.
- We need to do a large randomized strategy trial of broad versus targeted HCV screening with clinical outcomes. It’s true we do not definitively know that broad screening will prevent liver disease or death beyond a risk-based approach. But unfortunately, patients can be infected with HCV (and unaware of that fact) for decades before showing up with advanced liver disease. Seems that a cheap, reliable blood test is highly justified when we now have such safe and effective treatments.
I agree with the authors that longer-term follow-up data of treated patients are needed, especially using our currently available drugs.
The good news is that with thousands taking of advantage of HCV therapy — including many patients who could never be treated in the interferon era — and with over 90% of these patients cured (there, I said it), we shouldn’t have to wait long.
January 7th, 2015
Are the STI Screening Guidelines for Gay Men Overkill? (And Pedro Video.)
 Our “healthcare system” recently distributed a set of guidelines entitled, Primary care for gay men: screening and treatment recommendations.
Our “healthcare system” recently distributed a set of guidelines entitled, Primary care for gay men: screening and treatment recommendations.
It included, among other things, recommendations for screening for sexually transmitted infections (STIs) and anal cancer. The former it adopted from CDC guidelines, which are this this:
Screening at least once a year for syphilis, chlamydia, and gonorrhea for all sexually active gay, bisexual, and other men who have sex with men (MSM). [Emphasis theirs.] MSM who have multiple or anonymous partners should be screened more frequently for STDs (i.e., at 3-to-6 month intervals)
The anal cancer screening guidelines were kind of made up — pretty much like all recommendations for this form of cancer, since we don’t have solid data linking screening to a reduction in cases of invasive anal cancer and/or death. But in essence the guidelines recommend annual screening with anal pap smears for HIV positive men, and to “consider” screening HIV negative gay men every 2-3 years.
(Brief reminder here: Cancer screening — prostate, breast, colon, lung, ovarian, you name it — is kind of a complex issue. That, my friends, is so far the understatement of this baby year. In short, just because we can screen for some cancers, doesn’t mean we should. )
Anyway, the release of these guidelines prompted an email from one of my colleagues, a primary care physician, as follows:
I was reading the guidelines regarding recommendations for STI screening in all MSM (including annual HIV, urethral/rectal GC/chlamydia swabs, pharyngeal gonorrhea swab and syphilis testing) — is this something that you recommend in practice? I have a number of MSM patients in monogamous relationships so my approach has been to screen if new partners, etc. — and I have not been screening for everything, e.g., asymptomatic pharyngeal gonorrhea… seems silly, what’s the evidence?
They are also recommending consideration of anal pap 2-3 years in MSM who are HIV negative… Is that something you recommend? I worry that the benefits of downstream evaluation/treatment are not clear. Thanks so much for your wisdom!
Emily [Not her real name #1]
Moments after this Emily query, along came this, from a different physician-colleague, who is a gay man:
Hi Paul,
Wondering what you think of these recommendations for STI and anal cancer screening for gay men. I can tell you that my PCP read aloud the guidelines from his computer screen during a routine office visit. He did not ask me about specific risk behaviors and did not take a sexual history, but recommended anal pap because “according to the guidelines” I should have it done. Because I respected and liked him so much, I did not object, even though I thought it was a ridiculous waste of time and money. It would be helpful to know the strength of the evidence for doing an anal pap in HIV-negative men.
Charles [Not his real name #2]
So what’s going on here? Why did both these smart doctors — one as a clinician, the other as a patient — question the guidelines?
As usual, when faced with this kind of clinical quandary, I turned to the most brilliant person I know about patient dynamics, challenging encounters, and the mysterious emotional world of the people we see in clinic — our extraordinary social worker Susan Larrabee. Here’s her comment, quoted in full since it gets “right to the heart” of the issue, if I may use a phrase commonly employed by one of my favorite writers.
Is it possible some MD’s avoid difficult conversations (i.e. conversations they are uncomfortable having) by doing tests? And perhaps some of these same MDs are making these recommendations? I’m not above this in my own life, especially with my teenage kids and their visits with their pediatricians… they’re certainly not telling me (or maybe not their doc) everything. That is to say, there are many difficult conversations and many ways to compensate for our discomfort or the discomfort of our patients, with over-testing perhaps being one.
Susan [her real name]
This is, of course, exactly the issue. In fact, if one reads the guidelines carefully, it includes this key phrase: “these recommendations should be tailored to an individual patient’s risk profile.”
In other words, you can modify the screening according to the risk behaviors of the patient — but only if you take the time to assess it. Cynics will say that everyone lies about their sexual behaviors, but do we know if that’s really true? Better to ask and to talk about this stuff than just proceed blindly.
Speaking of brilliant, I enthusiastically agree that Pedro Martinez deserved his first-ballot induction into the Hall of Fame. (OK, admittedly a sudden transition, hence the Dominican Republic flag above.) He was perhaps the most extraordinary pitcher I’ve ever seen pitch live, and I’ve seen this guy, this guy, and this guy too.
Baseball fans, see what you think:
December 30th, 2014
Common Curbsides: The Patient with “Recurrent Zoster”
 Just in time for the New Year celebration, here’s a curbside consult I’ve received several times, probably because the answer isn’t in most textbooks. As usual, the actual question is slightly edited, as well as lightly (and affectionately) annotated:
Just in time for the New Year celebration, here’s a curbside consult I’ve received several times, probably because the answer isn’t in most textbooks. As usual, the actual question is slightly edited, as well as lightly (and affectionately) annotated:
Hey Paul — Quick question [of course] — I have a patient with a history of irritable bowel, otherwise well, who had shingles on her lower back a few years ago, approximately L5-S1. It was pretty bad, but ultimately improved on Valtrex. Since then she’s contacted me several times with recurrent zoster in the same distribution, each time it improves with more Valtrex. She’s not immunocompromised, HIV negative, not on steroids, etc.
Should she be on chronic suppressive treatment? If so, what drug and what dose? And how long should she be on it? Any role for the shingles vaccine? [Hey — you said “Quick question” — not “questions”! She’s only 42.
Thanks!
Anita [not her real name]
There’s a reason doctors have questions about their patients with frequently recurring zoster — it’s because the entity doesn’t really exist. That makes finding guidance for management extremely difficult!
Even a single recurrence is fairly uncommon in the same dermatome — an outbreak may boost native immunity — which is why patients with a history of shingles were not included in the pivotal study of the live zoster vaccine.
Recurrent zoster is rare enough that some question whether it makes sense to give the vaccine to people with a history of shingles, though in my experience these are understandably the patients with the greatest motivation to get vaccinated, so I’m glad the guidelines do endorse this practice. And one population-based study did find that a single recurrences of zoster occurred in people with a history of shingles at about the same rate as an initial episode. Prolonged pain was a risk factor for having another episode.
So if it isn’t recurrent zoster most of these patients are experiencing, what is it? So far all of the cases I’ve been referred have been one of these three things:
- Herpes simplex. This is far and away the most common mimicker. Obviously the skin lesions can look a whole lot like zoster, and since HSV is usually found in the oral or anogenital areas, the clinician and patient just don’t think about it when clusters of vesicles crop up somewhere else. (It’s what our very young patient summarized above had, of course.) Establishing the diagnosis is usually straightforward, either through a careful history or viral culture/DFA of an active lesion. Warning — some people with a history of “recurrent zoster” aren’t too thrilled to hear they have herpes instead, especially of the Type 2 variety, so caution when informing him/her of this diagnosis. All kinds of relationship turmoil can ensue.
- Post-herpetic neuralgia complicated by “neurodermatitis.” I put that last word in quotes, because that really isn’t the most common use of the term, but it truly fits. Here’s what happens — the patient with zoster has, as a manifestation of post-herpetic neuralgia, tingling and itching at the site. He/She then scratches and picks at it relentlessly, until the skin is red and bumpy — which is then mistaken for “recurrent zoster.” These itchy red bumps really look nothing like shingles, and of course are associated with no viral replication, but the location right at the site of prior shingles fools people.
- Wolf’s isotopic response. I’m lucky to have a brilliant dermatologist as a colleague; he clued me in to this oddly named entity, which is a fancy way of saying “a new skin disease at the site of an already healed, unrelated disease.” Turns out herpes zoster is the most common initial skin lesion, and then a whole host of other things can occur in that same site. Despite the name, it has nothing whatsoever to do with radioactivity, but sure will impress your friends if you mention it in casual conversation.
I’m sure this short list isn’t comprehensive, but you get the point. If you and the patient think it’s recurrent zoster happening over and over again, it almost certainly is something else, and the three entities listed above are a good place to start.
December 20th, 2014
New HCV Option Effective, Safe, Well-Tolerated — And Use Will Likely Be Driven by Payors
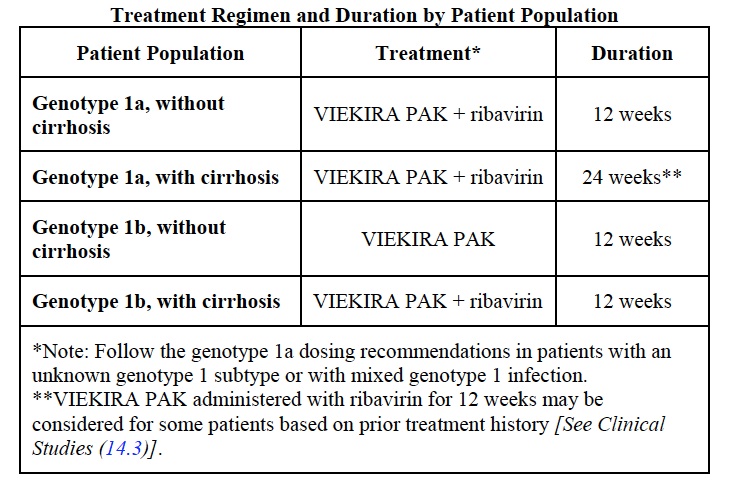
As expected, the FDA approved the next treatment option for HCV on Friday — “Viekira Pak”, a (sometimes complete) regimen consisting of ritonavir-booted parataprevir and ombitasvir given as a two pills once a day, plus one pill of of dasabuvir given twice daily. It is indicated for treatment of HCV genotype 1.
For those of you mechanistically inclined, parataprevir is a protease inhibitor, ombitasvir an NS5A inhibitor, and dasabuvir the first approved non-nucleoside polymerase inhibitor. Ritonavir is there for PK boosting.
Cure rates have been outstanding — 90% and higher — and severe adverse events rare. All good news so far.
So what’s the issue? The full prescribing information is here, but this is the key table:
Obviously, many patients will require concomitant administration of ribavirin, which makes this a considerably more complex regimen than the sofosbuvir/ledipasvir combination pill that has been available since October. Two other disadvantages include more drug-drug interactions (ID/HIV doctors are certainly familiar with ritonavir), and the potential for broader antiviral resistance if the treatment fails.
Whether these make a difference or not in clinical practice is a key unknown. But you can bet good Hanukkah gelt that payors are highly motivated to find out. Here’s some proof.
Hey, Happy 20th Birthday to this classic:
December 14th, 2014
2014 Top Stories in HIV Medicine
Boy do we love end-of-year “Best of …” and “Top Stories of …” lists! Love them! They never gets old! Until January, that is.
My own particular favorites are the Best Movies of the Year lists, since for whatever reason it always seems like some masterpiece slips by. Missed it! So we leave it up to the list-makers, either critics or review-aggregating sites, to remind us. Then we can print out the page, post it next to some Netflix- or other gizmo-enabled viewing device — and, if you’re like me, watch hardly any of the films, since if they were that good and the premise appealed to us when they were first released, then we’d have seen them already in the theater. Oh well.
(While I’m on the topic: There are literally dozens of Best Movie lists to choose from — hey, a list of lists! — just select your source: Rotten Tomatoes, Metacritic — which for the record I like more than Rotten Tomatoes, even though it’s less well known — New Yorker, New Yorker again, New York Times, some other city’s newspaper’s opinion, (LA and Boston haven’t weighed-in yet), IMDB, and Little White Lies, which gave us the nifty video at the end of this post.
Anyway — back to ID/HIV. For the last several years, the nice folks over at Medscape have allowed me to post brief videos on various HIV-related topics, including a “Top Stories in HIV” one each December.
These are decidedly low-budget affairs, shot on a antiquated Flip (remember those?) knock-off and usually set in my dining or living room. Here’s the most recent one, and for a special treat filmed this time on location on Tahiti.
(Actually, it’s my office.)
And since I’ve been told that these clips must be short — optimal length is around 3-4 minutes — allow me use this space to expand a bit more on the choices, roughly divided into Prevention, Treatment, Complications, and Cure. And this brevity definitely doesn’t allow digressions about Best Movies of 2014, or the relative value of metacritic.com vs. rottentomoatoes.com, both of which are probably owned by the same giant media conglomerate anyway.
Sorry, there are only seven. Why is 10 so important anyway?
- A more emphatic recommendation for pre-exposure prophylaxis (PrEP). I initially thought that PrEP was a niche prevention intervention, with the barriers to implementation just too high — the highest-risk patients didn’t get regular health care, compliance would be a chronic problem, and the cost of intervention unsupportable. So what changed? Plenty: a stronger endorsement to use it from CDC; research demonstrating efficacy in gay men even when they are only intermittently compliant; and the results of two other studies (PROUD and IPERGAY, ahem). This has translated into far greater enthusiasm from patients referred to me to discuss the PrEP option — all of the above has made me a believer. Not everyone agrees, of course, most emphatically the head of the AIDS HealthCare Foundation.
- Raltegravir beats darunavir and atazanavir in head-to-head-to-head clinical trial. First presented at CROI 2014, this important study showed that virologic outcomes were the same, but the safety and tolerability of raltegravir meant that overall it was simply better. Note that if subjects wanted to switch therapy — say, for a touch of atazanavir-related jaundice — they were allowed to do so and still stay in study, with the alternative medication provided. This no doubt lowered the threshold for ATV discontinuation substantially, but it is in fact what would happen in clinical practice. Two other quick notes: 1) One could argue that the real winner of this study is, ironically, dolutegravir, which we know is just as good as raltegravir, is once-a-day, and comes in a tiny little pill; 2) this is the kind of large clinical trial that the ACTG does so well — or I should write, did so well, since the research agenda has understandably switched to the next scientific challenges of cure and pathogenesis.
- Two-drug treatment approaches get some traction. While the NEAT study of darunavir/ritonavir plus raltegravir and the MODERN study of darunavir /ritonavir plus maraviroc added still more disappointing data on NRTI-free, two-drug combinations, along came the impressive results of lopinavir/ritonavir plus lamivudine — again just two drugs — in the GARDEL study, showing that less can definitely be more: the two-drug combination was just as effective, and better tolerated. Furthermore, the boosted PI plus lamivudine combination also seemed just fine for maintenance in the SALT and OLE trials. What about integrase/NNRTI as the two drugs? Cabotegravir (744) plus rilpivirine did quite well as maintenance in LATTE-1, suggesting a completely novel approach to less-is-more. This last result has prompted the development of a single tablet of this combination, along with the ongoing work using both of them as long-acting injectables — the LATTE-2 study, for those keeping track.
- Efavirenz associated with a more than twofold increase in risk of suicidality. Ever since efavirenz was approved in 1998, it has been something of a miracle drug from a virologic efficacy standpoint, beating or tying all challengers until it was compared to dolutegravir in the SINGLE study. Sure, efavirenz caused wacky dreams and dizziness, but serious CNS toxicity was difficult to pin down — until now. Acting on a hunch derived from reviewing safety reports from multiple studies, lead-author Katie Mollan designed an analysis that combined several randomized controlled trials, greatly increasing the chance of finding a concerning safety signal, which the paper most certainly did. Results were strengthened by the finding that deaths from injuries or unknown causes were also more common in the EFV-treated subjects. Note that even though the absolute risk of suicidality was low, this is such a serious side effect that it really should give us all pause before prescribing efavirenz to patients with a history of psychiatric illness. (Disclosure — I’m a coauthor on this study.)
- Interferon-free treatment of HCV (finally) arrives. Important because 1) a significant proportion of people with HIV also have HCV ; 2) patients with HIV coinfection now appear to respond just as well as those without HIV (unlike in the interferon days); 3) interferon truly stinks (that was not the first word I typed), and ribavirin isn’t so great either; 4) the first and second generation of interferon-free options — simeprevir plus sofosbuvir then the single-pill sofosbuvir/ledipasvir — are just so amazingly well tolerated; 5) the high cost of something this much better than the existing standard of care raises enormous pharmacoeconomic challenges; and finally, 6) how could the most dramatic advance in treatment of an infectious disease since the discovery of penicillin not be listed as a top story? Enough said.
- Early antiretroviral therapy for cryptococcal meningitis worsens outcomes. The COAT study has pretty much settled this controversial issue, with those given ART early having a 45% mortality at 26 weeks, versus 30% in subjects who waited 5 weeks to start ART. Low WBC in CSF was a particularly bad marker for poor outcome in the early ART group. Right now, cryptococcal and TB meningitis are the only exceptions to the rule that early ART is beneficial in patients with advanced immunodeficiency and AIDS-related complications. It’s likely no coincidence that both are forms of subacute meningitis associated with elevated intracranial pressure, where an increase in inflammation — IRIS — can be catastrophic.
- Curing HIV — it was hard before, now it’s even harder. The relapses of the two stem-cell transplant patients from Boston and the baby from Mississippi underscored that not only will curing HIV be a monumental challenge, but that the necessary step of getting there — a diagnostic test to tell us if our cure efforts are successful — remains an unsolved problem. In other words, all three of these patients had undetectable (or at most extraordinarily low) reservoirs as measured by the most sophisticated techniques. Not low enough, apparently, and not sophisticated enough either. One important thing to keep in mind as this research proceeds: we’ll need to make sure we don’t harm anyone with our investigational cure strategies, as current ART is pretty safe and effective.
Back to Top Movies of 2014, now with a video list. Just put your headphones on first.