An ongoing dialogue on HIV/AIDS, infectious diseases,
December 8th, 2019
A Midyear Letter to First-year ID Fellows — With Sympathy, Gratitude, and Hope!
Dear First-Year ID Fellows:
Right around now, some of you might be feeling a bit prickly. The workday is long, the supply of daylight dwindles daily, and the cold winds blow in from the north. While friends outside of medicine gear up for holiday time off, your plans might include some hospital coverage. Some of you have already worked Thanksgiving Day (and we thank you for that).
This testy feeling is totally understandable and appropriate — we definitely get it. Doing ID consults on hospitalized patients is hard — doing them during the first year of ID fellowship particularly so. For the record, let’s explore the reasons:
- Nobody gets ID consults on straightforward cases. I’ve said it many times, but it bears repeating — if the diagnosis is clear, the treatment going fine, and the patient improving, they won’t call you. Remember the Four States of Clinical Medicine? If not, here’s a reminder:
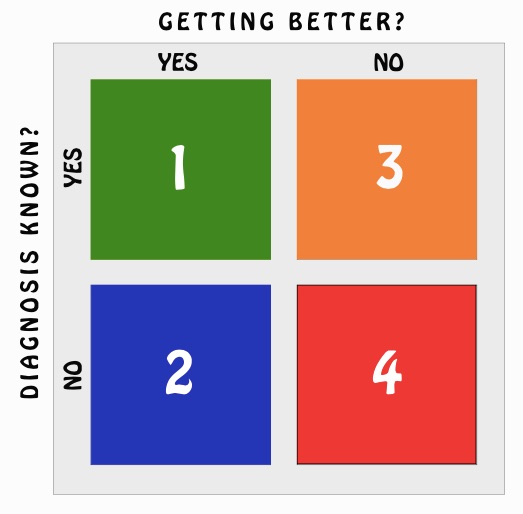 Maybe someone set up a clinical obstacle course just for ID, because all your consults come from Boxes 2, 3, or (shudder) 4 — actually, most from Box 4. Our job: move the patient back to Box 1 (best) — or at least Box 2 (second best) or Box 3 (third). Not always easy.
Maybe someone set up a clinical obstacle course just for ID, because all your consults come from Boxes 2, 3, or (shudder) 4 — actually, most from Box 4. Our job: move the patient back to Box 1 (best) — or at least Box 2 (second best) or Box 3 (third). Not always easy. - Certain ID consults challenge our emotions as well as our intellect. The previously healthy young person with a poor-prognosis hematologic malignancy and fevers despite broad antibiotic and antifungal coverage. The elder matriarch or patriarch of the family with a devastating stroke and recurrent aspiration, large family huddled in the room. The young man (it’s usually a man) with a spinal cord injury from a gunshot wound and severely infected pressure ulcers. The too-late HIV diagnosis with progressive multifocal leukoencephalopathy (PML) unresponsive to antiretroviral therapy. The person with diabetes who continues to lose their battle with vascular disease, requiring multiple amputations. Substance use disorder and all its various infectious complications. Wow, ID consults can induce sadness.
- Most surgery goes well — but when it doesn’t, the ID part is particularly painful. I have enormous respect for my surgical colleagues, who do things for patients I could never do in a million years. But when surgery goes wrong, and there are infectious complications, can anyone find a tougher role for the ID consultant than this? Since we’re on the floors more than the surgeons, sometimes it feels like we bear the brunt of the patient’s and their family’s disappointment and anger as much as — if not more than — the surgeons themselves. I doubt that’s true, but it can feel that way. Ouch. Particularly Ouch! when you’re a first-year ID fellow.
- There’s a ton we don’t know — and not knowing what we don’t know is part of being a first-year fellow. Back when I was a clinical fellow, I rounded repeatedly on a sick patient in the ICU who had fevers every single day. He had been admitted around the time of the signing of the Magna Carta, so it had been a lengthy hospital stay, to say the least. Despite our meticulous care and trying every antibiotic strategy known to humankind, every day — another fever. You know the case — a Fever of Too Many Origins. Frustrated, I repeatedly turned to my attending for help. Surely this esteemed ID faculty member with years of experience will solve the endless fevers problem. His response? “Sometimes we don’t know what’s going on, but we have to keep on trying anyway.” Not particularly articulate, but … Yep.
- Different supervising faculty have different expectations. Just when you’re getting comfortable with Dr. Attending #1, who wants short notes, targeted histories, just the antibiotics, only the WBC and creatinine, and then your bottom line impression and plan, along comes Dr. Attending #2, who wants every detail of the history, including every infinitesimally small data point — all the medications (with doses), all the labs (including the calcium and troponin), all the micro, and all the imaging, culminating in a note with the length of Mandell, Volume 1. (That’s 1919 pages, in case you’re wondering.) What’s the right approach? That’s the problem — there is no right approach for everyone. Just different clinical styles — but you, First-Year Fellows, are the ones who have to adapt.
Despite the above challenges, I hereby boldly proclaim that there is reason for optimism and genuine hope.
Reason #1: You are nearly half-way done. The end of this month is not just holiday season; it’s also the 50% mark on your first year. (I did the math.)
Reason #2: Your replacements are on the way. Match Day was last week. New fellows are really coming, and coming soon!
Reason #3: The hospital is quiet during holiday season. Yes, superstitious clinicians never make such optimistic predictions — but aren’t we people of science? Speaking as someone who has worked Christmas nearly every year since the start of the Clinton presidency, I can assure you that the hospital census goes way down in late December.
Reason #4: Free cookies, cakes, candies, and other snacks. These will start magically appearing on the hospital floors any day now, culminating in a peak supply on December 25.
Reason #5: The days will soon start getting longer. Sometime right after December 21, 2019, the Earth’s axis will gradually start tipping a bit more toward the sun each day. Promise!
Reason #6: You have already learned a tremendous amount of clinical ID! It is remarkable how steep the learning curve is for you ID fellows. Only around 6 months into your training, you frequently arrive at diagnoses and recommendations for consults that require little, if any, modification from us attendings. Your histories draw information from the patients, the families, and the outside hospitals; you relay our thoughts accurately and concisely to the referring teams. Cases that previously would have been overwhelming you now handle with aplomb. Keep up the good work, we appreciate it!
Reason #7: A man can play “All Star” on melons. If that’s not reason for optimism, what is?
(Start at 1’40” if you’re having a busy consult day.)
(Four States of Clinical Medicine graphic by Anne Sax.)


YES! I love everything about this, not the least of which being the ‘melon cover’ of Smashmouth! Thank you Dr. Sax for another poignant and extremely well timed Blog entry! This 2nd year Fellow appreciates it!
thank you