An ongoing dialogue on HIV/AIDS, infectious diseases,
April 8th, 2024
The Rise and Fall of Paxlovid
It’s been quite the ride for our “preferred” outpatient therapy for COVID-19, nirmatrelvir with ritonavir — much better known as Paxlovid, so allow me the license to use the licensed name.
Let’s recap the astonishing success and now failure of this intervention (some dates approximate):
- December 2021, the FDA issued an Emergency Use Authorization for Paxlovid: Action is based on the efficacy shown in the EPIC-HR study of high-risk outpatients with COVID-19. Compared to those receiving placebo, Paxlovid-treated participants had an 89% reduction in risk of hospitalization or death. Exciting times.
- Early 2022, that annoying rebound thing. No, it’s never been quite clear whether Paxlovid caused rebounds, or just didn’t prevent them, or whether it just happened in those people for whom COVID-19 illness lasted longer than the treatment’s 5 days (a large group!), but regardless — it was a major disincentive to clinicians and providers alike.
- December 2022, the protocol for the EPIC-SR in “standard risk” outpatients was amended to increase the sample size. Though an interim analysis suggested such patients would benefit from treatment, the change in sample size signaled that such a benefit observed in this analysis might be small — or nonexistent.
- August 2023, the negative results of EPIC-SR were posted on clinicaltrials.gov. Yes, these results have been in the public domain since last summer.
- Last week, the disappointing EPIC-SR results appeared in the New England Journal of Medicine. This is the primary endpoint (from the Research Summary):
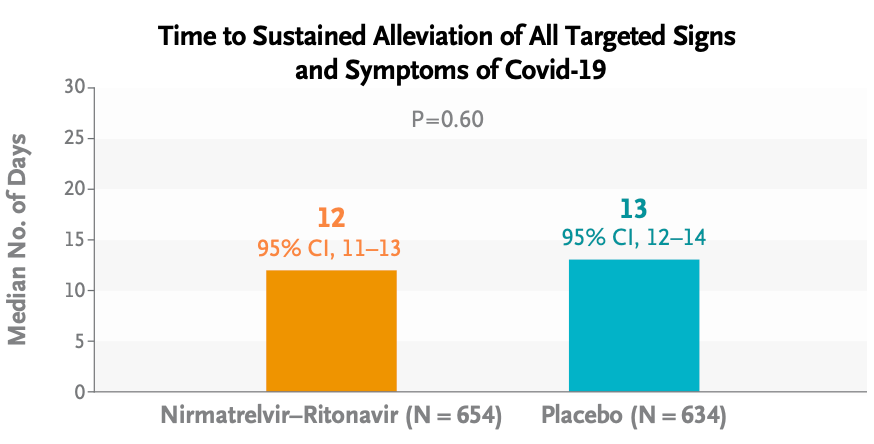
Oh well.
It wasn’t all bad news for treatment: Risks of severe outcomes (hospitalizations, ICU admissions, or deaths) were very low overall — hooray! — and numerically lower in the Paxlovid group; medical visits were significantly lower as well. However, as anyone who has taken Paxlovid can attest, the taste alone could have made study participants aware that they were already on treatment, hence discouraging them from seeking further evaluations.
What about rebounds? From these limited data, it appeared there was no difference:
By day 14, viral load rebound had occurred in 4.3% of the participants in the nirmatrelvir–ritonavir group and 4.1% of those in the placebo group; symptom rebound occurred in 11.4% and 16.1%, respectively, and symptom and viral load rebound together occurred in 1.2% and 0.5%, respectively.
So where does that leave us right now? There’s no doubt that the EPIC-SR data further confirm that this treatment has many limitations. Here’s a teaching slide I recently made:
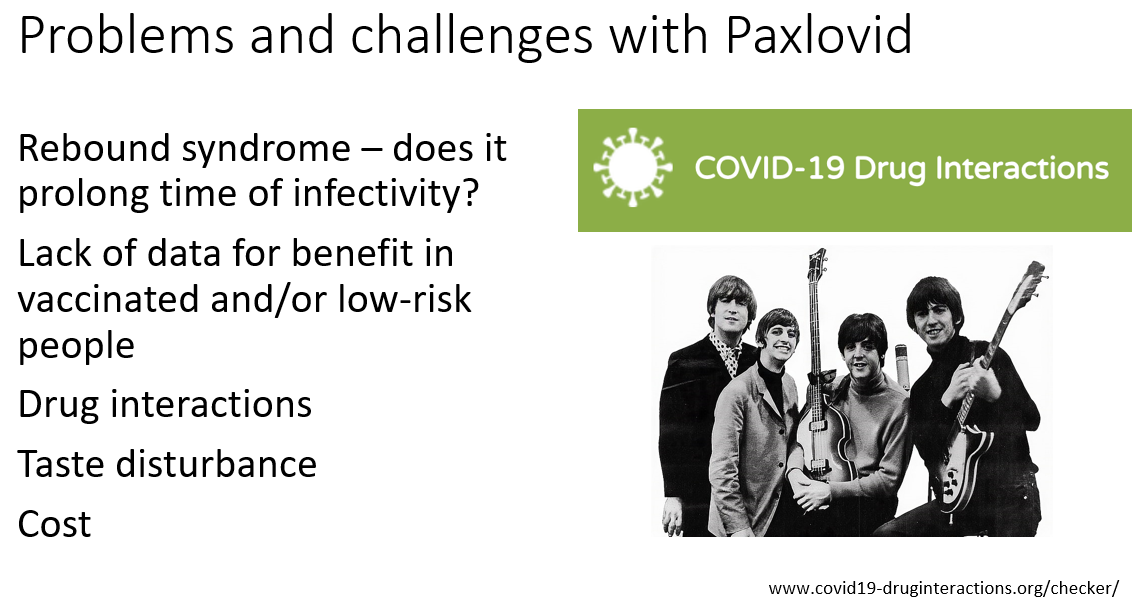
(If you’re wondering about the picture of the Fab Four, I can’t reference anything based in Liverpool without citing two of its spectacular exports — the Beatles and the University of Liverpool drug interactions checker!)
But before we completely abandon Paxlovid for outpatient use, let’s remember that our options for outpatient treatment of COVID-19 remain highly limited. Furthermore, people at high risk for adverse outcomes still require hospitalization and still die from this infection — as they do from other viral respiratory illnesses. As a result, based on EPIC-HR, these EPIC-SR data, and the observational studies, I’d still recommend treatment for this very high-risk group.
For others? Allow me to quote (with his permission) my smart colleague Dr. Athe Tsibris, a virologist who sent me this email after his own unfavorable experience with treatment last fall — the subject line read “Boo Paxlovid”:
Hi Paul,
Having just gone through Paxlovid rebound with my 1st covid infection (I held out as long as I could!), I’d like to share an entirely unsolicited observation and two rants:
1. The dose and/or duration is clearly wrong. Started within 48hrs of symptoms and rebounded – documented with daily antigen tests – harder than then original infection!
2. The company line of 2% incidence of rebound is laughable
I would not take Paxlovid again. I understand the limitations of human psychology, but for someone very low risk like myself, I don’t know how hard I’d push it on similar patients
Athe
For low-risk people, I totally get it.
Meanwhile, the gargantuan PANORAMIC study of Paxlovid in outpatients has closed to enrollment, with data collection continuing until September. Will this study provide any further evidence of the benefits or risks of treatment?
Regardless of the results, I do hope that the appetite for better treatments for COVID-19 remains, as this virus isn’t going anywhere.


“Furthermore, people at high risk for adverse outcomes still require hospitalization and still die from this infection — as they do from other viral respiratory illnesses” with or without treatment, I might add
Would qid nirmatrelvir alone be better tolerated and more effective?
In my whole ID career, I have never encountered a field with data as contradicting as COVID-19 therapy. Influenza could be able to compete closely. Numerous studies, including double-blind RCTs with remdesivir and numerous other medications, have produced varying and occasionally contradictory findings.
It is really difficult to understand the science behind COVID-19 treatment.
I would say, “No benefit in vaccinated and/or low-risk people (AI)” instead of, “Lack of data for benefit in vaccinated and/or low-risk people”.
Having said all of this, it is also necessary to recognize the integrity of disclosing unfavorable findings in industry-sponsored RCTs that have such a significant financial impact. However, although EPIC-SR took several months to publish from August 22 to April 24, EPIC-HR was released in a matter of days.
I made that slide before publication of the EPIC-SR study!
-Paul
I agree, Josep Libre.
We had such vigorous scientific debates during the early days/years of HIV/AIDS, resulting in rapid advancements of our understanding of opportunistic infections and immunology of AIDS, compared to historical standards.
In my long career in ID, I’ve never seen anything like what we’ve seen and continue to see related to the COVID-19 pandemic—suppression of broad, open, transparent scientific debate, and flawed/weak science behind favored treatments and vaccines. The FDA has been inexplicably slow to act on other potential therapies.
IDSA and ID leaders have not advocated publicly for robust data driven COVID-19 decisions/policies as CDC and our government have so badly failed our country, ignoring and even silencing highly qualified experts who were recommending a better path from summer 2020. Our most vulnerable populations, including lower income school children and their families, have been most harmed as a result.
It’s been heartbreaking as an ID physician to see our profession not step up to this challenge, but, rather, fold under the pressure of politics.
drb219@gmail.com
I hear you and agree
the struggle with new disease becoming a political and possibly financial free for all has been disheartening Think the damage to health care practitioners will exceed the cost of covid itself. I question things I never questioned before and yet I have seen scientific fraud. but it was caught and dealt with. This was a tsunami
I’m a Family Doc, so I’m not an expert on bugs. But, I suspect there is so much contradictory information because of various vaccine histories of the patients and various strains of the virus. I think we need for someone to come up with new ideas in ID trials, where we can test treatments as the background information changes. For instance, we should be able to do a quick flu vaccine trial every year, turn the results around by mid-Fall. Do the same with COVID and COVID therapeutics. Isn’t this what the CDC should be doing, before we spend millions of dollars every year on a new public health campaign for each disease? Is there any way to get better information?
Lots of good ways to check for DDIs. Just curious, Dr. Sax, why the plug for Liverpool?
You are correct, many good ways. But I’ve found that for the disease areas they focus on — HIV, HCV, and COVID — nothing is quite as clear or well-referenced. (Plus, I like the Beatles.)
-Paul
And Home of the Liverpool Soccer Team ⚽
Thanks for this blog post, Paul. It helped clarify a confusing situation. I wish I weren’t so skeptical about biomedical treatments for COVID (and other medical conditions), but the rise and fall of Paxlovid demonstrates to me that what we confidently recommend to patients is often wrong. -Phil
The data are all over the place. It’s frustrating and difficult to imagine why length-of-treatment studies have not been published. It’s probably more effective to treat for 10 days if you’re going to do it, but we have should have had those results by now. Even the data regarding post-infectious sequelae are inflicting. Still, can you really feel good about withholding Paxlovid in people 65+ with co-morbidities? At least have a conversation.
Paul, before we give up on Paxlovid, we need to look at the major flaws in this study, as outlined by Drs. Gandhi and Hirsch in the accompanying editorial. My main concern is that the median age of subjects was only 42, and only 5% were over 65. Less than 2% had heart or lung disease. This study doesn’t give us much, if any, information about the patients most at risk for bad outcomes if they get Covid-19. Thoughts?
Agree! Which is why I wrote this:
The study was called “SR” for “standard risk”, which is why there weren’t more high risk people in the trial.
-Paul
I would also point out the constant, increased exposure of the general public and of healthcare workers in pharmacies due to the filling of prescriptions of Paxlovid. Pharmacy workers are exposed to Covid at least daily because patients come in for their Paxlovid for themselves. Some providers give patients paper prescriptions that must be turned in to the pharmacy before they are filled, causing numerous exposures during that process. The patient then thinks they are going to sit in the waiting area for 45 minutes to an hour, right next to the patients who are elderly or immunocompromised who are waiting for Covid vaccinations. Even if this portion does not occur and it is sent electronically, most Paxlovid patients pick up for themselves, standing in line for how long, surrounded by other pharmacy patients and other passersby to check out at the register. They are then presented to the pharmacist who unknowingly come upon the patient within 2 feet without any warning and no opportunity to put on any protective equipment (not that we even have any protective equipment anymore, all the plexiglass has been taken away everywhere and KN95 masks are no longer provided by employers). So for Paxlovid to *possibly* shorten the duration of symptoms by a single day weighed against the number of infections caused by a single person being prescribed Paxlovid, I think it should be taken off the market. These scenarios, the lack of conscientiousness and concern for others, and lack of efficacy make Paxlovid a threat to public health.
This is a good point. Why is it that one needs to have a confirmed case of Covid before Paxlovid can be prescribed? Right now doctors can only prescribe it for patients with documented Covid. Patients at high risk should be able to get a prescription ahead of time so they have it in hand and can start Paxlovid on day 1 after testing positive. They shouldn’t have to wait in line in a pharmacy when they at risk of spreading the disease and likely feeling very sick.
Before taking it off the market (perhaps throwing away the baby with the bath water) ought we not to examine good data on the high risk patients most likely to benefit from it ? I can certainly see your reluctance to expose low risk patients, but they are also the ones least likely to have benefit from any treatment. If those over 75 with lung or heart disease or obesity have a number needed to prevent a hospitalization of 30 or 50 or 100 might that not at some point cause you to treat them? How about we spend more effort getting data on the high risk patients before allowing the minimal benefit in low risk patients to cause us to abandon the drug.
Thanks for this post. Another frustrating issue with this treatment is that after administering so many doses to standard risk folks, the medical profession has yet more egg on its face in the treatment of COVID. I’ve already heard comments that we were somehow colluding with the pharmaceutical industry. Ugh. Paul, can you delineate with which groups you will continue with Paxlovid treatment?
Amusing. No one should care (much) about time to alleviation of symptoms. The endpoint that affects society and the individual alike is prevention of severe disease (+ hospitalization and death). In easily identifiable high risk patients, the data is clear. The rest is just noise.
Cool that we now know R/N is pretty worthless for simply making people “feel better,” so we won’t waste inventory and money on simple palliation. PCN doesn’t do much to reduce strep symptoms but that’s not why we write it. The benefit in reducing the incidence of rheumatic fever (i.e., “severe disease”) is worth it.
This clickbait title risks clinicians under prescribing this medication, and your protestations that (paraphrasing) “I wrote people should still use it” don’t fly…that paragraph is buried so deep few will see it. How about “Ritonavir/Nimeltravir is ineffective for symptom relief, but high risk patients still benefit”? The use of brand names takes away from your message as well, but in this case perhaps that’s for the best.
Dr St: You are being very snarky to Paul Sax, a wonderful person who does not deserve such a a dismissive tone. He’s doing the hard work of communicating the best information he can obtain in the setting of a very confusing public health crisis. Say on, Paul.
Dr. St. I agree with every word you said. We should emphasize the importance of preventing severe disease, not bury this benefit of R/N in an article that broadly characterizes the medicine as irrelevant (i.e. “the fall”).
The link in Dr Sax’s bullet #5 goes to the older EPIC-HR from 2022 that had positive results. The link to the current EPIC-SR is https://www.nejm.org/doi/full/10.1056/NEJMoa2309003
Thanks, fixed it!
There has been a hint that perhaps paxlovid may decrease the chance of acquiring long covid. Given this possibility and the data we have to date regarding benefit of keeping HIGH RISK patient out of the hospital and from dying there still seems to be a role in select patients. I share the data we have at the moment with colleagues, patients, and friends who ask including pros and cons. Then patients can decide their own risk benefit. I’m a fit, healthy, fully vaccinated 66 year old male. I personally would lean toward taking paxlovid as I consider long covid a dreadful potential illness and hospitalization undesirable. But I can respect the opposite view as well. The science of covid is break neck and I think genuinely the cdc, fda, and individual clinicians and practitioners have tried to interpret it along the way as best as possible. I don’t buy that politics pushed an agenda or any of the conspiracy bs. Tens of thousands of people were being hospitalized and dying weekly in the beginning and we did what we could as information came along. With hindsight and the threat lessening substantially we should learn where improvements are possible for the next pandemic not trash talk the whole effort.
I agree with you 100%. The risk of severe disease and long COVID should not be diminished.
I am over the age of 75 and I have had Covid 3 times in the past two years. With the help of Paxlovid,
each episode was brief and mild. I think this is because of 2 actions that I took. Two of the Covid attacks were while I traveled out of the country. I therefore carried paxlovid with me and started taking it within minutes after a positive Covid test; not waiting 5 days to start the medication.
I took the full dose for three days, and then one dose per day for four more days for a total of seven days. This reduced the side effects and prevented rebound. I believe that starting Paxlovid quickly after testing positive, and extending the days of medication to 7 made the drug optimal for me.
I always refill the prescription whenever I use the drug, so it is always quickly available if needed.
I was fully vaccinated and got COVID in July 2022. I took Paxlovid on the day that I got fever. I was miserable and had fever for 2.5 days. 99% Paxlovid helped with shortening symptoms. No side effects from Paxlovid. I would take it again without any doubt. I wasn’t dying, I just felt sick. On a sample size of one Paxlovid helped a lot.
The tragedy of the Covid pandemic, in my humble opinion, was not about treatment but rather about the failure, and lack of public understanding of our Public Health system in this country. Sure, Public Health has always been the step-child of Medicine, but we really saw that play out over the pandemic. I heard people say they thought Public Health was health care for the poor. Basic public health measures were not well explained or widely and properly practiced. I don’t fault those trying to do their jobs, but rather the lack of adequate funding and support for their efforts. And that must be in place before a pandemic, rather than trying to build the ship at sea. Are we any better prepared for the next pandemic? I’m not sure we are.
If you read the actual initial testing report prior to the FDA approval, there was significant concern raised for risk of mutation of host DNA and thus increased overall cancer risk with taking Paxlovid. However, the panel understandably concluded-if taking this medication in patients with an ACTUAL high risk for death and poor outcomes, they would recommend the Drug for use in THOSE populations for treatment of (the much more fatal strain) if Covid-19.
Initially prescribing this medication to our patients was very limited to these clear high risk populations, but eventually everyone/anyone could get paxlovid, with significant marketing “If it’s covid….Paxlovid” and the like.
Has anyone looked at this data, and seen any concern for possible increased lifelong cancer risk involved with taking this medication, as expressed by the researchers in the testing panel prior to FDA approval?
At the first sign of any respiratory symptom, including sore throat or runny nose, or diarrhea, I start testing for COVID daily. I then test daily for 4 days. On the 4 occasions that I have tested positive (usually after air travel or a cruise, though fully vaccinated), I take my first dose of Paxlovid within the hour. All symptoms are 95% improved within 48 hours. No recurrence. No long COVID.
This is very different from the 3 to 5 days of symptoms before starting the drug allowed in the studies I’ve seen.
I will continue to recommend Paxlovid and recommend that patients test early and test often and get on the medication ASAP after testing positive. A prescription is just a phone call away and the drug store is nearby in our part of the world.
I have a history of asthma. When I had COVID paxlovid was a wonder drug. Symptoms settled overnight. No rebound. Would take again.
Lali Sekhon MD PhD MBA
Paul, would you mind commenting on which groups you would give Paxlovid to at this point? What is your current threshold for “high risk”? Also, I have been giving Metformin along with Paxlovid to reduce the risk of long COVID…is this still advisable? Thank you!
The group at highest risk of severe infection is over 65. The older, the greater the risk. How does a study in a group with few such patients address the need for paxlovid for those patients? Along with comments in this string, Michael Osterholm in a recent podcast advised caution in applying data from this study to patients over 65. In short, we should take care to avoid the classic pitfall of “extrapolation beyond the data points.”
Interesting.
I don’t see the data on hospitalization and mortality here. Is there any data?
As it often said the only thing worse than NO data is BAD data. Careful review here reveals significant flaws in the information and interpretation.
Paxlovid made a huge difference to our COVID symptoms for my husband, me and even my son who was at high risk for complications. Fever spikes began coming down very quickly and symptoms improved. Rebound was mild. Taste was not a big deal especially for those of us who have ever taken metronidazole.
Bottom line: Paxlovid helped prevent an escalation of our symptoms, recovery was much quicker than it would have been, taste and rebound were hardly an issue given what we were dealing with.
Is this an opinion or assessment of data in so far? The CDC recently reviewed the data on COVID rebound with R/N and found no significant difference between R/N and no treatment. We are even provided an anecdotal personal account by an MD, how relevant is that? Preliminary data show less hospitalization and death and that’s all we have so until more numbers come in why continue to speculate. It’s a sad day with medical journals use headlines as attention getting tools conveying the wrong conclusion. Why are we calling this the “fall” of R/N? I recently had COVID despite vaccination and being a healthy 71 yo, felt better day after, then rebounded day 9. I’m not sorry I took it because I may have avoided a trip to the hospital, a ventilator, or death. Those who are impatient for conclusive data will have to wait.
The indication for Paxlovid was for older individuals and sicker individuals. My issue is with the significant number of medication contraindications and the minimal benefit.
Please note and hopefully accept the experience of a physician who is faced with adults whose lives have been taken from them by the debilitating neurologic symptoms of “long COVID” for whom I have had extraordinarily positive results with Paxlovid taken in bursts over up to a month. Returns to their previous emotional and physical capacities are seen. The NIH is beginning a large study via Harvard and Duke using a course of 25 days of Paxlovid to establish the validity of what other physicians as well as myself have already found.
I have personally seen, as primary initial diagnostician, over 5000 cases of COVID in the field since Feb, 2020.
Gregg Grinspan, MD
All I know is that when I took it (for both acute and rebound) it worked within 24 hours. I would take it again in a heartbeat!
Without pointing fingers, I despair when I think how this experience will arguably leave us LESS prepared politically and a socially with the next inevitable pandemic. There will always be gaps in knowledge and tough choices in such situations, but I fear we have now changed from a society that when push comes to shove, follow CDC/expert etc recommendations in the midst of limited knowledge during a novel a public health crisis , to a society that that will disregard such advice until proven otherwise. The lay public is simply unequipped to make those distinctions, but the public at large seems to think it is. The root cause is our declining level of education at large in an increasingly diverse nation layered onto our historic libertarian, skeptical independent nature.
Personal experience, (N of 1) but TWO episodes, high risk by virtue of age and diagnosis thought associated with impaired immunity. Both times tested within 24 hours of symptoms, started Paxlovid within 36 hours of symptom onset. Symptoms essentially RESOLVED within 12 hours of first dose both times. Symptoms recurred at 3 to 4 days after last dose, were associated with repeat positive test, and lasted 3 to 4 days (but were never anywhere near as severe as the original onset). And yes, the dysgeusia is very irritating.
Hi all good comments. As an NP and not in ID – two thoughts come to mind. – one -reasonable minds can disagree. and two – if excellent medical ppl cant agree — it is certainly confusing what to recd to patients and even for our selves !!
I sadly got covid three times. – not until 4/23 when my clinic stopped masking and I traveled. (ugh masked ! ) Up until then I thought I had a covid super power, I took Pax twice but not the last time and feel fortunate to be fine. ,,,
Agree different strains most likely and luck too,
The FIRST TIME I was SICK ! but stayed out of ER !
I just wish the public had more faith in medical ppl. and I blame that on Trump (sorry had to get that out lol ).
Paul, I’m afraid that your title and most of your article feed into the political and conspiracy theorists view of COVID, whcih is still resulting in the majority of deaths from covid- the data seem to show that the people who are dying from COVID are those who did not get vaccinated and those, usually with high risk, who did not take Paxlovid.
I don’t think, as your title suggests, that Paxlovid has failed, but rather that we have defined who benefits from it and who doesn’t. Burying the benefit in a hidden paragraph surrounded by the negative data does you and everyone a disservice.
I am a relatively healthy 72 y/o PA who was unscathed during the pandemic, despite working in a major NYC hospital. On a Thursday morning this past February, while being fully vaccinated, I awoke with mild URI symptoms and self tested positive for Covid. I began Paxlovid that evening as I had been on Simvistatin and needed to wait. By Friday, the symptoms worsened, similar to the flu. On Saturday I was totally asymptomatic and stayed that way thereafter with a faint positive test on Sunday and negative the following days. I am not sure about what may have happened without Paxlovid, and the taste was so off putting that I considered not completing the full course. Even though I did, I wonder how many patients who experience rebound did not finish the full course of the medication. I completely agree that not enough is being done to further develop better treatment options.
Standard protocol should be 10 days therapy. In my own limited experience this prevents rebound.
Re effectiveness in vaccinated patients. Real-world cohort studies show effectiveness of Paxlovid against disease progression: Israel (78% vaccinated or previously infected, age >65, hospitalizations cut by 73% and deaths by 79%); New England (all vaccinated, age >50, 40% and 71% respectively); Colorado (78% vaccinated, 55% and 85%), and Southern California (94% vaccinated, cut progression by 79.6%). The refs are https://www.nejm.org/doi/full/10.1056/NEJMoa2204919, https://www.acpjournals.org/doi/10.7326/M22-2141, https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(23)00011-7/fulltext, https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(23)00118-4/fulltext
There’s no conspiracy; just the usual tension between underfunded objective science and well funded pharmaceutical research. May I remind us of the debacle of remdesivir? After a very disappointing trial on hospitalized patients, where it failed help any patient oriented outcome (no change in intubation or mortality), IT WAS STILL APPROVED and endorsed as treatment, to the immense financial benefit of Gilead. However, it took two more years for there to be a trial showing that it reduced hospitalization and death by a substantial amount if given early in the outpatient setting. If Gilead had been told their drug was ineffective from the start for hospitalized patients, maybe they would have been more eager to push through trials for outpatients, and we could have gotten some benefit from remdesivir, and paid billions to Gilead for something useful, like saving lives. I agree- likely it is time to stop prescribing Paxlovid to the healthy vaccinated individual. But the unvaccinated or unhealthy- we do not have the data. I’d be a bit surprised that it helps much in any but the most immunocompromised vaccinated individuals, and would love to see the data. I have no idea why anyone prescribes oseltamivir to anyone- it has never shown a benefit in reducing hospitalization or death, not even when influenza was H1N1. Yet it remains a recommendation.
There is a bigger cognitive error that our profession, the pharmaceutical industry, and our government health leadership are all making: maybe we should call this error the kitchen sink phenomenon. Whenever something is scary, bad, or deadly, we become willing to throw anything at it, including the (useless) kitchen sink. Or in this case, remdesivir used in a pointless way, or overuse of Paxlovid.
How, in the future, can we avoid this error?
Hi, Paul,
This discussion confirms what I do now and my impression that the sequence of events during the pandemic was best efforts in a terrible time.
We all have perspective and some time under our belts. However, scientific community, I believe, is still sluggish with practical guidance.
I just saw Paul at the Jimmy Buffett celebration of life in LA last week! So thank you for your article and for your Fab Four reference from one Paul fan to another!
I had all the vaccines. My one trip out of the country resulted in my first bout of Covid. I took Paxlovid and felt better in 24 hours. Second bout after attending a crowded Christmas concert I did the same thing, same result. Being 70 with Crohns disease I did not want to take chances.
I am a family doctor who treats patients who are over 50, obese, heart or lung patients, or diabetics with paxlovid. No hospitalizations or deaths from COVID since last year when I started. Enough said ( for me)