An ongoing dialogue on HIV/AIDS, infectious diseases,
May 23rd, 2010
Dengue in the News … Again
The recent dengue cases acquired in Florida prompted me to think of two things.
First, is this really a surprise? Dengue has become increasingly common in the Caribbean, the mosquitoes that transmit the virus are widespread in the United States, and it’s not as if there’s some sort of microbiologically (if that’s a word) impermeable barrier between the islands in the Caribbean and our southernmost states:

Add a dose of climate change (not mentioned in the MMWR editorial — just a hunch), and bingo, the perfect recipe for tropical diseases in the Continental 48.
Still, many kudos to the astute ID doctor in Rochester NY who made the diagnosis:
During this third visit [to her primary care doctor], a consulting infectious-disease specialist raised the possibility of dengue infection, despite no recent travel by the patient to a known dengue-endemic area.
Hey, this is why they pay us the big bucks!
The second thing I thought about was another time dengue was the headline in MMWR. Anyone remember the really big news in MMWR when the lead was “Dengue type 4 infections in U.S. travelers to the Caribbean”?
May 18th, 2010
Electronic Medical Records and (LONG) ID Notes

When it comes to writing consult notes, it often seems as if we ID specialists have a blatant form of obsessive-compulsive disorder. Every detail is fair game — travel history, dietary habits, all sorts of seemingly trivial exposures, and of course microbiologic data stretching back to the Cretaceous period.
I’ll never forget receiving sign-out from the graduating first-year ID fellow when I started my fellowship. It included a photocopy of a consult note she had written the day before on a woman with fever after gallbladder surgery.
In five pages of meticulously-detailed prose, there was this memorable item from the Social History:
Two pets at home: a dog (Rusty) and cat (Cleo); both are healthy.
Good news for Rusty and Cleo! But what could this possibly have to do with post-operative fever after gall bladder surgery? Even if you allow that perhaps she was suffering from some bizarre post-cholecystectomy zoonosis (if there is such a thing), why was it necessary to cite the pets’ names?
Electronic medical records have, if anything, made matters even worse for the detail-obsessed. The ability to cut and paste endless reams of data into a note is irresistible to most ID docs.
It leads to a bizarre paradox where the more information in the note, often the less useful it is — a phenomenon expertly dissected over here on the always-interesting KevinMD blog. Says guest writer Jaan Sidorov:
[A doctor] had received a copy of a lengthy consultant-physician’s documentation involving one of his patients and was astonished by the blob of past data, prior notes, test results, excerpts, quotes, interpretations and correspondence that had been replicated word-for-word in the course of “seeing” his patient. The terse portions describing what the patient actually said, what the consulting doctor actually examined and what the diagnosis and plan were were inconspicuously buried toward the end of the EHR document.
And you know what’s most maddening? Under the current “guidelines” for coding and billing, there are true incentives — both financial and regulatory — to write this kind of text-heavy note, one heavily infused with templates and boilerplate language. The more complexity the better!
Here’s a proposal: the goal of a consult note should be concise documentation of what you think, and why, then what you’re recommending, and why.
I’m sure Rusty and Cleo would agree.
May 9th, 2010
Amusing Medical Cartoons … and Humor in Medicine
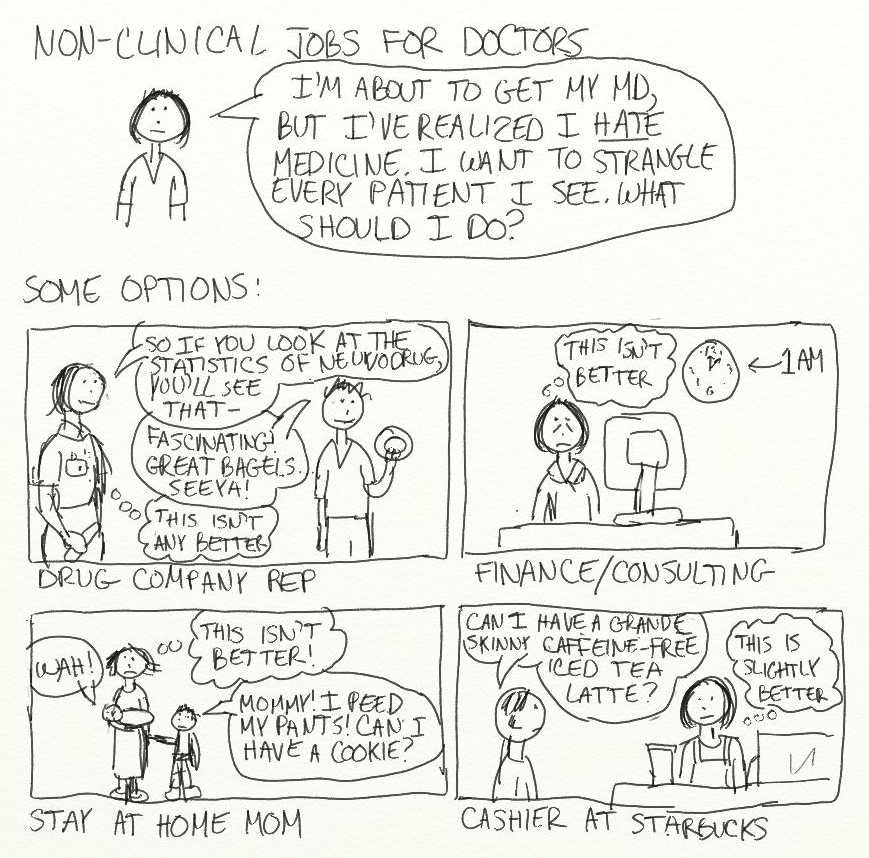 Someone pointed out this cartoon to me.
Someone pointed out this cartoon to me.
What an eloquent depiction of the interior dialogue of a young doctor as she considers various non-medical careers.
Brilliant!
Which led me to thinking more broadly about humor in medicine, about which I quickly remembered that anyone writing about humor (as opposed to writing humorously) will be instantly unfunny.
Sorry.
So let me be brief, and say that I hung around with a bunch of people in college who made cartoons like these their principal means of communication. And that crude art notwithstanding, there’s a real talent to to it.
And most of these are great.
I wonder what she/he (I assume she?) thinks of ID specialists …
May 4th, 2010
Zoster Vaccine Underutilized
 From the Annals of Internal Medicine:
From the Annals of Internal Medicine:
Eighty-eight percent of providers recommend herpes zoster vaccine and 41% strongly recommend it, compared with more than 90% who strongly recommend influenza and pneumococcal vaccines. For physicians in both specialties [Internal Medicine and Family Practice], the most frequently reported barriers to vaccination were financial.
From my admittedly biased perspective as an ID doctor, recommending the zoster vaccine is a no-brainer. The cases of zoster I see are severe, and complicated, and people with post-herpetic neuralgia (who sometimes find their way erroneously to our clinic) are miserable.
But I’m also biased in that I’m not in a private, independent practice, and hence not responsible for getting reimbursed for giving a vaccine with irregular insurance coverage and finicky storage requirements.
So my guess is that were the vaccine universally covered (i.e., “free”), that there would be much broader uptake.
After all, for most Americans over 60, which is more likely to prevent illness — the zoster vaccine or the tetanus booster?
April 24th, 2010
Choosing an Official State Microbe
 Wisconsin has selected Lactococcus lactis as its official state microbe:
Wisconsin has selected Lactococcus lactis as its official state microbe:
The people of the state of Wisconsin, represented in senate and assembly, do enact as follows: SECTION 1. 1.10 (3) (t) of the statutes is created to read: 1.10 (3) (t) The bacterium Lactococcus lactis is the state microbe. SECTION 2. 1.10 (4) of the statutes is amended to read: 1.10 (4) The Wisconsin Blue Book shall include the information contained in this section concerning the state song, ballad, waltz, dance, beverage, tree, grain, flower, bird, fish, animal, domestic animal, wildlife animal, dog, insect, fossil, mineral, rock, soil, fruit, and tartan, and microbe.
As any self-respecting Packer fan could tell you, Lactococcus lactis is a critical part of making cheese, in particular the state’s famous cheddar.
And though the bill passed last week, I have three remaining very important questions:
- What were the other contenders? When I think Wisconsin and microbes (which I do several times a day), probably the first bug that occurs to me is Borrelia burgdorferi (Wisconsin is a notable non-New England/Mid-Atlantic epicenter for Lyme Disease), followed shortly thereafter by Diphyllobothrium latum (think various marinated and uncooked fish popular in northern European diets). Did these get any votes?
- What will Massachusetts choose? I could see Erysipelothrix rhusiopathiae, though perhaps Maine has a stronger claim to this lobster-related bacterium than we do — we’d better have a back-up in place, such as Babesia microti or Cyclospora cayetanensis, though for the latter the reference might be a bit obscure.
- Will other states go for the obvious choices? Legionella pneumophila for Pennsylvania, Coccidioides immitis for Arizona, Vibrio vulnificus for Louisiana, etc. You get the idea.
Finally, note that Wisconsin has both a state mineral and a state rock. In these tough economic times, you would think one or the other would be sufficient.
April 22nd, 2010
Should Transmission of HIV be a Crime?
 Not according to Journal Watch editor and New York Times writer Abigail Zuger, writing here in the Times. She’s referring to the recent Darren Chiacchia case, where his former partner has filed a legal complaint that Chiacchia did not disclose having HIV — potentially a first-degree felony in Florida.
Not according to Journal Watch editor and New York Times writer Abigail Zuger, writing here in the Times. She’s referring to the recent Darren Chiacchia case, where his former partner has filed a legal complaint that Chiacchia did not disclose having HIV — potentially a first-degree felony in Florida.
Were it a matter of science alone, all those AIDS statutes could be rescinded tomorrow. But the science was only a small part of the panic that created them. And effective treatment has not altered the rest of that potent emotional brew: the virus still sows terror, uncertainty, shame and endless complications, whether the infection is concealed or revealed…
Now we think we know better, but do we really? We blame that coughing woman in the subway for our cold, the giant meat company for our food poisoning, all manner of chemicals and electromagnetic radiation for our cancers, and fast-food outlets for ourdiabetes and heart disease. We cannot experience illness without casting around for blame.
Yet at the same time we believe deeply in prevention. Surely if we watch our diets and get our mammograms and colonoscopies, wash our hands, take whatever vitamin is foremost in the news and eat our burgers well done, we can avert bad things. Whole generations have now grown up knowing that sensible people “play safe,” with the overriding implication that if you catch a sexually transmitted disease, you have no one to blame but yourself.
Then the key point:
And so whose fault is a new H.I.V. infection, really? Is it mine, for giving it to you, or is it yours, for being stupid and cavalier enough to get it?
(Sorry for the lengthy quotes, she’s such a great writer it was irresistible.)
I mostly agree with Abbie that effective treatment of HIV has changed the risk equation profoundly, and that what originally motivated these laws — transmission of HIV was murder! — no longer holds. But remember that some (most?) might think that transmission of any infection — herpes, syphilis, MRSA, salmonella from peanut butter, hepatitis A from spinach — is potentially a crime, provided there’s evidence of deceit or negligence.
And people holding this view will continue to see these HIV statutes as completely justified. As a result, don’t expect them to be removed from the books anytime soon.
April 10th, 2010
Why Are Doctors Still Carrying Beepers?
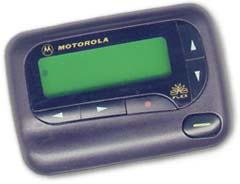 I was going through security at the airport the other day, and tossed my beeper into one of those gray bins — along with the device that should make the beeper superfluous, a cell phone.
I was going through security at the airport the other day, and tossed my beeper into one of those gray bins — along with the device that should make the beeper superfluous, a cell phone.
“I didn’t know anyone used beepers anymore,” said the 30-something guy behind me.
What could I say? That doctors also use typewriters, buggy whips, and ice boxes?
But those are really the wrong comparisons — better is something more early-90s, like this “mobile phone.” For a while back then, beepers were quite the status symbol among the junior high school set — especially if they were made of clear, teal-colored plastic.
And while teenagers have long ago moved on, virtually every doctor I know still carries a beeper. One of my un-named colleagues (at and un-named hospital in an un-named city) became so frustrated by having to carry two devices that he hacked into his hospital’s paging system. He now gets pages on his cell phone as text messages.
(He says texts over cell phones are sent via the same technology as pages. Who knew?)
This article discusses some reasons why beepers have certain advantages over other wireless systems. But that was two years ago, and given advances in cellular technology, I find it hard to believe those advantages wouldn’t quickly be overshadowed by all the obvious benefits of a cell phone, particularly a modern smart device.
I, for one, would be happy to trade mine in. Just say the word.

 Over on our Journal Watch AIDS Clinical Care site, we did a
Over on our Journal Watch AIDS Clinical Care site, we did a 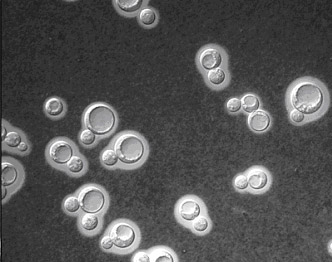 In the ongoing debate about when to start antiretroviral therapy in our sickest patients — those with acute opportunistic infections — comes
In the ongoing debate about when to start antiretroviral therapy in our sickest patients — those with acute opportunistic infections — comes  =
= .031, by log‐rank test). The risk of mortality was almost 3 times as great in the early ART group versus the delayed ART group (adjusted hazard ratio, 2.85; 95% confidence interval, 1.1–7.23). The study was terminated early by the data safety monitoring committee.
.031, by log‐rank test). The risk of mortality was almost 3 times as great in the early ART group versus the delayed ART group (adjusted hazard ratio, 2.85; 95% confidence interval, 1.1–7.23). The study was terminated early by the data safety monitoring committee. Over in Journal of Infectious Diseases, the MERIT study
Over in Journal of Infectious Diseases, the MERIT study 