An ongoing dialogue on HIV/AIDS, infectious diseases,
July 11th, 2015
Citing WHO Guidelines, Squirrels Protest Latest Virus Discovery
 An open letter to the Editor-in-Chief of the New England Journal of Medicine
An open letter to the Editor-in-Chief of the New England Journal of Medicine
Saturday, July 11, 2015
Dear Dr. Drazen:
On behalf of the International Association of Variegated Squirrels, I am writing to protest the article that appeared in your July 9 2015 issue, entitled “A variegated squirrel bornavirus associated with fatal human encephalitis.”
We variegated squirrels believe the title and content of this paper are stigmatizing to variegated squirrels, and are not in keeping with recent guidance from the WHO regarding best-practices in naming new diseases.
As a reminder, variegated squirrels the world over are trying to counter literally centuries of discrimination and injustice. Indeed, the paper you published includes these chilling sentences:
All three patients [with encephalitis] were breeders of variegated squirrels (S. variegatoides). They were friends, had met privately on a regular basis, and had exchanged their squirrel breeding pairs on multiple occasions.
In our opinion, this involuntary captivity and heartless exchange of fellow variegated squirrels highlights the ongoing challenges we face on a day-to-day basis.
In addition, based on extensive communications I have had with non-variegated squirrels, I am concerned that the paper will have a similarly negative effect on all 200 squirrel species. From the five-inch African pygmy squirrel to the three-foot Indian giant squirrel, all are upset about this stigma by association. And you don’t want to get a three-foot squirrel mad at you, trust me on that one.
Squirrels — variegated and non-variegated alike — have much to be proud of. Before scientists go and name a scary viruses after us, please keep in mind the literally millions of innocent fellow squirrels who roam free, climb trees, nibble acorns and other nuts, and have never transmitted a disease to anyone.
Respectfully,
Rocky
Chairman and Spokes-Squirrel
International Association of Variegated Squirrels
[youtube http://www.youtube.com/watch?v=1EnDwkclDcA&w=420&h=315]
(H/T to Rebeca Plank for the photo and link to squirrel facts.)
July 7th, 2015
For HIV in the USA, Not in Care Exceeds the Undiagnosed — Solutions Welcome
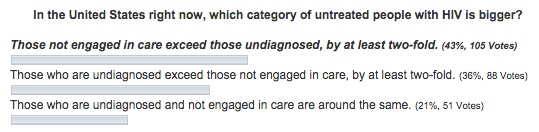
In last week’s post, I asked about two of the key components of the HIV care cascade — the “undiagnosed” vs the “diagnosed but not in care,” and which group was larger in the USA. Here are your answers as of now:
The people who read this site are a pretty knowledgeable group when it comes to issues related to HIV. This is not a blog about collecting beer steins, philosophical ruminations over baseball cards, or knitting, to cite three mentioned to me by patients over the years.
(That middle one is quite something. As is his book, if you’re into that kind of thing. Which I am.)
But more than half (57%) of even this erudite readership got the question wrong — because in the United States, those diagnosed but not in regular care greatly exceed the undiagnosed. It’s by a factor of more than two-fold to one, at least if you believe the CDC data displayed in this nifty video.
In the undiagnosed, there’s been progress: making HIV testing easier has resulted in a great reduction in those who have HIV but don’t know it. The latest data from CDC have just been published, and we’re down to just 14%. Yes, 14% is still too high — and it’s up to 25% undiagnosed in certain regions (we’re looking at you Louisiana) — but it’s a vast improvement over the 30-40% estimates we were seeing 10 years ago.
And in many regions, it’s now < 10%. Meaning that more than 90% of those with HIV know that they have it, and can get on treatment, prolong their lives, and stop spreading the virus to others.
Now, about that much bigger other group — 30-40% or so of those with HIV in the USA — who know they have HIV and aren’t getting care and treatment.
What’s up with that?
Solutions to this problem eagerly awaited.
[youtube http://www.youtube.com/watch?v=CWf5LBfZVGQ&w=560&h=315]
July 1st, 2015
Undiagnosed or Not in Care? For HIV, Which Is the Bigger Problem?
 These days, it’s hard to have a “closed book” examination.
These days, it’s hard to have a “closed book” examination.
The information is everywhere — on your computer, your phone, your tablet — whatever screen happens to be glowing in front of you.
“In the age of the internet, why be wrong?” is something my son used to say as we sat at the dinner table, grappling to remember who was the mother of Perseus, the flight time between Boston and Ft. Lauderdale, or the new name for Haemophilus aphrophilus.
(Still can’t get over that one. And yes, ID doctors have fascinating dinner table conversations.)
So it’s tough to ask you to try and take this quiz without heading over to the CDC and finding the answer. But give it a go because 1) I have a theory, triggered by a patient with advanced HIV disease I just saw in the hospital — which somehow always feels like a failure of our healthcare system — and 2) if you get it wrong, who cares? Nobody will know.
The question is about how we can possibly still have untreated people with HIV in this country, even though the medications are widely available, highly safe and effective, and simple to take. Plus, there are numerous programs in place to ensure that pretty much everyone who needs it can get coverage for treatment.
Is it that they are undiagnosed and hence don’t know that they should be on treatment? Or do they know that they have HIV, but for some reason aren’t engaged in regular care?
June 24th, 2015
Epidemic of Republican Presidential Candidates Shows No Signs of Abating
Chilling news from The Borowitz Report:
The number of official candidates for the 2016 Republican Presidential nomination has risen to thirteen, according to officials at the Centers for Disease Control…
“It might have been misplaced optimism on our part, but we had started to believe that this thing had been contained,” said the C.D.C. spokesman Dr. Harland Dorrinson. “Regrettably, it has not.”
While scientists disagree about how running for President spreads from person to person, most epidemiologists believe that a candidacy needs an environment rich in narcissism and delusion—plus a host to feed on, ideally a sociopathic billionaire.
When I contacted the author regarding this disturbing information, he responded:
You were my target audience for this one.
Does this mean he makes up the news on his site?
I’m shocked to hear that.
[youtube http://www.youtube.com/watch?v=DR01liZXlNE&w=560&h=315]
June 20th, 2015
Alex Rodriguez’ Story Reminds Me of a Case of Scientific Misconduct — Until It Doesn’t
If you’ll forgive me a bit of baseball-related rambling, there’s an incredible story going on this year with the resuscitation of Alex Rodriguez, both as a player and, even more remarkably, as a person in the public eye.
Or, to quote the play-by-play announcer Michael Kay, who on Friday got it perfectly when he commented on A-Rod’s 3000th hit (it was a home run):
In the space of about a year, he’s gone from persona non grata to the Man of the Hour.
To quickly recap A-Rod’s “crimes,” these included the use of steroids to boost performance, lying about it when caught, and then attacking his employers in court in a pointless effort to get his full-year suspension dropped. All that behavior led to the “persona non grata” part of the A-Rod story.
And while there are still some baseball fans who hate the guy (especially around this neck of the woods, see this play for a prime example why), there’s no doubt he’s been cheered plenty this year — cheered perhaps more than any time since the sensational start to his career as a brilliant young shortstop for the Seattle Mariners.
First, he’s having an excellent season, and second (and in some ways even more remarkably), he seems to have undergone a personality transplant. His previously awkward manner now comes across convincingly like sincere humility. Whatever genius is acting as his media coach — or seeing him for psychotherapy — should win a Nobel Prize in … something.
In short, A-Rod has remade his baseball career and, at least partially, his reputation.
Which got me wondering — would we be so forgiving for such behavior in academic medicine? Scientific misconduct, in particular fabrication of research data, has several parallels.
In both settings, the guilty parties start with genuine talent, widely recognized and praised. Soon after start the short cuts to success. And in both, after an initial period of denial, rationalization (“everyone is doing it”), and self-justification (“I am so gifted/brilliant that this is what I would have accomplished/found anyway”), the evidence of guilt becomes overwhelming. This is followed by swift public censure and various degrees of punishment.
The parallels end, of course, with the postscript. A-Rod is getting another chance by many because, well, it’s just a game. And we love comeback stories in sports.
In scientific misconduct — especially the egregious cases — the stakes are too high.
Forgiveness is just not part of the story.
And apologies to one of my readers from Germany, who told me he never gets it when I write about baseball.
June 11th, 2015
Summer Is Almost Here ID Link-o-Rama
I know, I know. You’re sick of hearing Bostonians complain about the winter we just had. But did you know that the weather here didn’t get reliably warm here until, well, this week?
We all have PTSD. Don’t talk to us about anything even vaguely white, flakey, and cold. Yes, we’re afraid of refrigerated coconut.
I’ll stop whining now.
- The spread of MERS in Korea is facilitated by severe overcrowding in hospitals. Who knew that getting a hospital room in Seoul was like trying to get a reservation at a top restaurant in New York City.
- Remarkable paper on survival after AIDS-related opportunistic infections in San Francisco since the beginning of the epidemic. Vast improvement over time, of course, but not uniformly among all OIs — outcomes for lymphoma (especially CNS) and PML are still dismal.
- A short-course of antibiotics (4 days) for abdominal infections seems to be just fine. The challenge, of course, is not with straightforward cases — it’s the ones where “source control” can’t be verified. Or, to quote the fine accompanying editorial, “Early in the 21st century, it seems likely that source control remains a considerable problem in treating abdominal sepsis.” Indeed. So though it’s an important study, I don’t think we’re quite ready to remove this from the unanswerable questions list.
- Like something out of science fiction, this test can tell you every virus you’ve ever been exposed to. Based on personal domestic experience, I would bet pediatricians break all kinds of records for positivity on this one. And how long before you can get this test done at your local CVS? Further discussion here in the New York Times, in case Science isn’t your cup of tea.
- The Sexually Transmitted Diseases Treatment Guidelines have been updated, a heroic effort that will be cited and referred to many, many times. It’s a vast document, so use the above CDC link (which has a Table of Contents) rather than the MMWR one, which doesn’t. Apps coming soon per lead author Kim Workowski.
- Provocative piece on the complex issue of academic-industry relationships, which raises the distinct possibility that anti-industry sentiment might have gone too far in medical research and publishing — a view echoed here by the Editor-in-Chief of the NEJM. Getting this issue reviewed from a different perspective is most welcome, as I can’t imagine how we could have made HIV treatable without this collaboration. Not surprisingly, these views have engendered some controversy, including from former editors.
- Related topic — here’s a fascinating profile of nucleoside-nucleotide guru Raymond Schinazi, the man responsible (to at least some degree) for several groundbreaking HIV and HCV therapeutics. This is not your typical PhD academic scientist — how many have earnings that rival hedge fund managers, George Clooney, or Alex Rodriguez? And who is more deserving?
- Shigella with resistance to azithromycin and quinolones, and widespread resistance of salmonella to quinolones. The news on these enteric bugs keeps getting worse. Thoroughly cook those burgers this weekend!
[youtube http://www.youtube.com/watch?v=pZPlfuJYViE&w=560&h=315]
June 4th, 2015
A Slightly Less Painful Way to Learn the Three-Letter Abbreviations for HIV Meds
 One of the stupid things about being an HIV/ID specialist is the highly arcane code we use to abbreviate HIV treatments.
One of the stupid things about being an HIV/ID specialist is the highly arcane code we use to abbreviate HIV treatments.
Why was zidovudine originally AZT, and now ZDV?
Why is lamivudine 3TC?
And tenofovir TDF?
Of course there are legitimate biochemical reasons why these are the right abbreviations, but they are lost to most of us who do not have degrees in medicinal chemistry.
Which is why I would like to share that someone I know — a highly brilliant researcher with dozens of papers in high-profile journals, innumerable grants and awards, and many successful mentored investigators — can’t keep these abbreviations straight.
Example: He recently shortened rilpivirine to RLP.
Sorry, “RLP” isn’t going to cut it. It’s imaginative, and original (I’d wager no one has ever used it before), and starts with the right letter, but someone of his stature would certainly be expected to know that it should be RPV.
Of course, he’s not the only one who has trouble with these tricky abbreviations. Medical students and residents despair at learning them, and ID fellows struggle as if they were learning the coagulation cascade. I recently had one smart and experienced PharmD tell me they were “alphabet soup”, and that the abbreviations for HIV meds always threaten to make any lecture on treatment deadly boring.
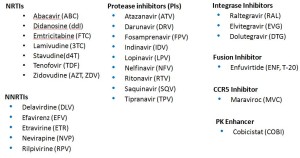
With that in mind, here’s some help. In an effort to help struggling Newbies and Full Professors alike learn these key abbreviations, I’ve pasted below three lists — Advanced, Essential, and Basic HIV Medication Lists.
First, Advanced — the whole kit and caboodle, all 27 medications (click to enlarge):
The secret here is that many of these medications are of historical interest only. You don’t really need to know the lousy old meds that are barely ever used anymore — am thinking of you ddI, d4T, SQV, IDV, DLV…
Sure, many HIV/ID specialists pride themselves on knowing all of them — and even more, that they know the years of FDA approval (of the original drug and coformulations), and the trade names. Most will even know the meds that are no longer available — for example, that ddC was the abbreviation for zalcitibine, a horrible NRTI that had the even more horrible brand name Hivid. Good grief, what were they thinking?
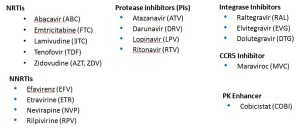
Second, the Essential list — the ones that I’d say are critical to know for most HIV/ID specialists. Note that even though several of these drugs are rarely used any longer as initial therapy (e.g., nevirapine, lopinavir), many patients still are on them and doing great — so you’ll still come across these in practice now and again:
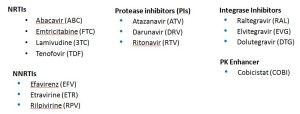
With that second list, we’re down to a mere 18 meds. But it can get even simpler, with the Basic list:
Ah, that’s better — now we’re down to just 14 — the antiretrovirals you’re most likely to encounter actually received by a patient in 2015. One might quibble and say that exclusion of lopinavir and maraviroc was unjust, but hey — we’re talking basic here! Learn these first.
Take it away, Trip.
[youtube http://www.youtube.com/watch?v=uQnDqULwPv4]
May 27th, 2015
START is STOPPED: Study Confirms HIV Treatment Is Beneficial for All, Even Those with High CD4 Cell Counts
The Strategic Timing of AntiRetroviral Treatment (START) study began in 2009, enrolling over 4000 asymptomatic people with HIV and CD4 cell counts > 500, and randomizing them to immediate ART or to wait until the count dropped to 350. Now, from the National Institute of Allergy and Infectious Diseases comes this important announcement:
Though the study was expected to conclude at the end of 2016, an interim review of the study data by an independent data and safety monitoring board (DSMB) recommended that results be released early… Based on data from March 2015, the DSMB found 41 instances of AIDS, serious non-AIDS events or death among those enrolled in the study’s early treatment group compared to 86 events in the deferred treatment group. The DSMB’s interim analysis found risk of developing serious illness or death was reduced by 53 percent among those in the early treatment group, compared to those in the deferred group.
So now we have it — definitive evidence that it’s better to be on HIV treatment than to wait, even for those with normal CD4 cell counts and no symptoms.
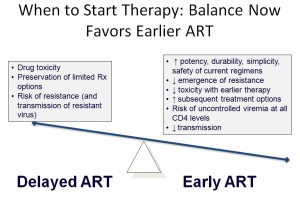
It’s worth revisiting, just for history’s sake, why the START study (which opened in 2009) was even done. Remember that once upon a time — OK, a bit more than a decade ago — we tried to wait long as possible before starting someone with HIV who was asymptomatic on antiretroviral therapy. Wait until CD4 = 350? Or even 200? No big deal, provided they had no HIV-related symptoms and were closely monitored.
Seems impossible now — how could we have done such a thing? A bunch of reasons, most (all) of them irrelevant or disproven over time:
- HIV treatment had short and long-term side effects, some of them potentially severe. This was the primary motivation to wait, and actually quite true in the AZT, d4T, ddI, indinavir, etc., era. Of course much less so now. But in the era of lipoatrophy, lactic acidosis, lipoatrophy, high pill burdens, and GI side effects, it made sense to wait if possible.
- We thought there was no downside to waiting, since the immune function (as measured by CD4 cell counts) would return to safe levels after starting ART. Unfortunately this recovery doesn’t always occur, plus we now know there was irreversible loss of immune function based on CD4 nadir.
- Viral replication without loss of CD4 cells was viewed as benign. The potentially deleterious effects of immune activation and inflammation were barely considered, especially before we know the results of the (similarly named) SMART study of intermittent therapy.
- If we treated “early,” then options for therapy would become limited due to resistance — including when patients really need ART (i.e., have low CD4 cell counts). This view was based on the assumption that treatment failure with resistance was inevitable — turns out it’s not. We furthermore didn’t know that the late 2000s would bring a spectacular flurry of drug development for patients with resistant virus. Finally, it ignored the fact that the best way to avoid having a low CD4 was to not let it drop in the first place!
- No clinical trial proved that waiting was harmful for patients with high CD4 cell counts. Over time, there were three randomized studies supporting earlier therapy (one done in Haiti, the clinical outcomes analysis of HPTN 052, and more recently TEMPRANO) — and a fourth if you count the SMART “naive” analysis. However, doubters maintained that most of these data (SMART excluded) were collected in resource-limited settings, and/or used CD4 thresholds that were too low.
- The full benefit of HIV treatment as prevention was not fully appreciated until HPTN 052. Even though indirect data strongly suggested that HIV treatment would reduce viral transmission, it wasn’t until the results of HPTN 052 became available in 2011 that this extraordinary advantage of being on suppressive therapy really hit home, both for providers and patients. This completely changed the dialogue in the clinic — now asymptomatic people with HIV want to be on therapy, for obvious reasons.
The above advances in knowledge have meant that in the United States, HIV treatment guidelines have recommended that all patients with HIV be treated for several years — specifically:
Antiretroviral therapy (ART) is recommended for all HIV-infected individuals to reduce the risk of disease progression … ART also is recommended for HIV-infected individuals for the prevention of transmission of HIV.
It couldn’t be clearer, but to put it in the way familiar to anyone who’s taught from any “HIV 101” slide set, here you go:
So while the results of the START study are important — and when the full analysis is released, will be fascinating — the study results will not have much of an impact here. Pretty much everyone in care is on therapy already.
The study will, however, have substantial implications globally, where deferring therapy remains a common strategy for patients with high CD4 cell counts.
And score one for Alice Pau and the prescient DHHS Guidelines — they first made this call in 2012. She won’t say, “I told you so,” so I’ll say it for her!
May 21st, 2015
Which Infectious Diseases Do We Fear Too Much? Which Not Enough?
 My friend (and HIV/ID colleague) Mauro Schechter sent me a funny email the other day — from Brazil, where he lives and works:
My friend (and HIV/ID colleague) Mauro Schechter sent me a funny email the other day — from Brazil, where he lives and works:
I just read your post and watched the news clip about Powassan. And you still wonder why we think you Americans are paranoid disease freaks? 65 cases in 12 years in a population of 350 million, and you’re worried??? [The three question marks are his.] Definitely something to get worried about.
Mauro
His last sentence registered 10 out of 10 on the sarcasm meter, and of course Mauro has a point — the risk of getting a severe case of Powassan encephalitis is tiny, even in tick-filled New England. Can’t we Americans find something more appropriate to be afraid of?
On the other side, we’ve had a couple of cases in our hospital, and it really can be quite serious. More importantly, we USAers have a deep-rooted fear of not having enough to fear, and a new tick-related illness fits that void quite nicely — especially on a slow news day.
Which made me wonder — which Infectious Diseases do we fear too much? Which not enough? Here’s a list, compiled with extensive scientific rigor and years (ok, minutes) of painstaking research:
FEAR TOO MUCH:
- Rabies. It’s hard to say that a disease that is nearly 100% fatal and causes thousands of deaths a year can be feared too much, but that’s the bizarre situation with rabies in the United States. The reality is that we have typically 1-2 cases of rabies here each year, and there is no evidence that this is likely to increase anytime soon. Yet think about all those urgent calls, late night trips to the emergency room, and series of rabies vaccine given for possible “occult” exposure to bats. Remember this Canadian study? They estimated that the number of people needed to treat to prevent one case of rabies after bat-in-bedroom-but-no-bat-bite (longest compound phrase I’ve ever written) could be as high as 2.7 million! Not surprisingly, the Canadians no longer recommend rabies vaccine after bats are found in the bedroom. We still do.
- Pharyngitis, possible strep throat in adults. The most feared complication of strep throat is arguably acute rheumatic fever, but: 1) Strep throat is mostly a disease of children and young adolescents, most adults have some viral thing (see below for an important exception); 2) Most acute rheumatic fever occurs in kids as well — even many ID doctors of a certain age (that means older than I) have never seen acute rheumatic fever in an adult; 3) The incidence of acute rheumatic fever has been incredibly low for years in our country, for reasons independent of antibiotic use.
- Conjunctivitis. This ugly, uncomfortable malady makes people really, really scared, and brings out horrible fears of contagion in the school and workplace. You’d think it was a serious, and highly contagious ID emergency. It isn’t.
- Mosquito-related Encephalitis. 2005 was a relatively bad year for Eastern Equine Encephalitis — and there were 21 cases in the whole country. But most years there are only a few, yet this doesn’t stop the near annual news media terror when some mosquitoes test positive. Or a horse dies! Or the mosquito spraying starts! Fear of West Nile Virus means a dead bird can lead to panic, triggering unnecessary calls to the Department of Public Health. Plus there was this bit about canceling high school football. As with rabies, it’s important to acknowledge that these conditions can be incredibly serious, and life threatening — but should they occupy such a big space in our collective fear center?
- Bronchitis. First a little cold, which lingered, but now it’s become bronchitis. Terror, and cue up the Z-Pak!
FEAR TOO LITTLE:
- Influenza. “It’s just the flu”, people say. But people are wrong, pretty much every year. Let’s hope our vaccine gets better — how about one that you only need every five years, not one that needs to be repeated more often than renewing your car’s registration? Progress in the flu vaccine — whenever that happens — will have a transformative effect on community health.
- Clostridium difficile. The emergence of the hypervirulent strain of C. diff should profoundly change the risk vs benefit calculation with any antibiotic prescription. Has it? I know one oral surgeon who will never use clindamycin again, after a “routine” post-operative course caused severe C diff, leading to a colectomy in a previously healthy patient. But how about before the prescription?
- Infectious endocarditis and other bacterial complications of injection drug use. The outbreak of IDU-related HIV in Indiana is appropriately getting plenty of press — HIV is still an incurable disease, much-feared among everyone, including those who inject drugs. But all ID doctors know that the rise in use of heroin has led to a much more pervasive epidemic of endocarditis and other serious invasive bacterial infections. And these are emphatically much harder to treat than HIV, and so much more immediately life threatening. Do people with addiction fear these as well?
- Atypical mycobacteria. There should be a support group for patients with non-tuberculous mycobacterial infections. Pulmonary and non-pulmonary infections from these diverse bugs can be incredibly tricky to diagnose and treat, yet hardly anyone in the non-medical public knows about them. Why is that?
- Fusobacterium necrophorum. The adolescent or young adult with severe exudative pharyngitis, systemic toxicity, and a negative strep test could easily be dismissed as having “only” viral pharyngitis. Yet we now know that a subset will be PCR positive for fusobacterium, the primary cause of septic jugular vein thrombophlebitis (Lemierre’s syndrome), a potentially devastating complication.
- MRSA. New drugs notwithstanding, and even with a decline in incidence (what’s causing that?), MRSA remains the most difficult to treat commonly encountered infection out there. Just ask any ID fellow — what other common infection persists so stubbornly, or recurs so frequently, despite “appropriate” antibiotic treatment?
- Vaccine-preventable diseases of childhood. Self-explanatory.
Would be interested to hear what conditions you think should be on these lists. And as the days grow longer, and we get closer to peak Lyme season, I thought long and hard about where Lyme should go, and concluded it could be on both lists — feared too much by some, too little by others.
See if you can guess why.