An ongoing dialogue on HIV/AIDS, infectious diseases,
March 4th, 2018
Winner of ID Cartoon Caption Contest #3, and Here’s #4 Just in Time for CROI
One of the challenging aspects of writing this blog is that there is so much interesting material in the ID/HIV world that sometimes I forget to cover critical items.
Example: the winner of the most recent ID Cartoon Caption Contest, which I’m embarrassed to admit, has been awaiting its announcement since late 2016.
The winner:
It’s a great caption, trouncing the very strong competition of 3 other finalists by garnering 62% of the vote.
But I confess we here at NEJM Journal Watch were torn between this one and “Have you tried switching him off and back on again?,” which we thought would finish stronger than its 13% of the total vote.
Concerned, we asked our crack team of cybersecurity experts to investigate further, and we’re proud to announce there was no Russian meddling in the voting process. Hence, the winner is clear.
So congratulations to Steve V., who submitted the top caption! As I’m sure he’s aware, he’s the winner of a lifetime free subscription to this blog, good in all 50 states and US Territories. If Steve V. is from another country, he can continue to access the blog provided he has a valid yellow fever vaccination certificate.
Now, onto the next contest. Some of us in the ID/HIV world will be coming to Boston for CROI this week, but fortunately my skilled collaborator Anne Sax not only isn’t attending CROI, she also has no idea what “CROI” even is.
Working together (my idea, 100% her drawing), we’ve come up with the doctor-patient encounter displayed below, perhaps inspired by last week’s Nor’easter.
As before, write your proposed caption in the comments section, or pop it on my Twitter feed — or, if you’re feeling shy, email it to me at id.caption@yahoo.com.
February 25th, 2018
Is Self-Administered Postexposure Prophylaxis Another Viable Option for HIV Prevention?
Most of the pivotal trials of pre-exposure prophylaxis (PrEP) have used daily therapy.
The lone exception is the IPERGAY study. Men at high risk for acquiring HIV took two tablets of tenofovir DF/emtricitabine (TDF/FTC, Truvada) before sex, and one tablet the next 2 days.
The strategy was highly effective in preventing HIV acquisition, and intermittent PrEP is endorsed as an option in France, where the study was conducted.
(About that name — it stands for Intervention Préventive de l’Exposition aux Risques avec et pour les Gays. I have it on good word from the lead investigator that they can say it in French without smiling.)
The main concern some have raised about the IPERGAY results is that participants had relatively frequent exposures (a median of 4/month), enough so that sufficient tissue levels of TDF/FTC could be maintained.
But what about even less frequent high risk exposures, say a few of times a year? Daily PrEP for these patients seems like overkill, and intermittent PrEP may not work. Might they benefit from a different prevention strategy?
A group in Toronto just published a novel approach to these patients — instead of giving them PrEP, they are recommending on-demand postexposure prophylaxis (PEP).
(In the paper, they call it “PEP-in-pocket,” or “PIP,” but I don’t think we can tolerate another one of these single syllable abbreviations in HIV prevention that begins with “P.”)
From 2013–2017, two clinical sites identified relatively low-risk individuals from those who were initially referred for PrEP.
The preventive strategy consisted of prescribing a 28-day supply of TDF/FTC plus dolutegravir, with instructions to start it as soon as possible if the patient had what they deemed to be an exposure that might transmit HIV.
Thirty such people were identified. In the follow-up period, 4 of the 30 initiated PEP on their own, all doing so within 10 hours of the exposure. Each reported good adherence to their treatment, and were closely followed-up.
All who started preventive medications were seen in clinic within a week for clinical evaluation and blood work. There were no HIV seroconversions in 21.8 person-years of follow-up.
Of course, the small size of the study, and its retrospective, non-comparative design hardly are sufficient to incorporate this strategy into guidelines.
Nonetheless, there are several advantages to this on-demand PEP strategy. These include avoiding daily exposure to medications, lower drug costs, reducing emergency room visits, and still providing some preventive intervention, just in case. Individuals who start on-demand PEP multiple times can be transitioned to PrEP, which is what happened to 4 of the patients in this study.
I look forward to hearing more about this approach — and I’d be saying that even if the senior author weren’t a graduate of our ID fellowship program!
(Nice work, Isaac.)
February 19th, 2018
Can We Solve the Morass of Outpatient Intravenous Antibiotic Therapy?
If you want to get an ID doctor riled up, here are a few reliable strategies:
- Get an ID consult on a complex patient just to summarize the chart for your discharge summary.
- Endorse the view that procedural doctors deserve their vastly higher salaries than MDs in cognitive specialties.
- Prescribe azithromycin for patients with bad colds.
- Discharge a patient from the hospital on intravenous antibiotics when an oral antibiotic would work just as well.
I’ve not hidden my distaste for unnecessary “outpatient parenteral antimicrobial therapy,” or OPAT on this blog, once devoting a whole post to oral antibiotics with excellent absorption.
It’s not just the inconvenience and potential dangers (blood clots, secondary infections from the IV catheters) of OPAT that I dislike. It’s also that there is essentially no support (read: money) for the clinicians charged with monitoring these complex patients, or for coordinating the many people who may be involved in their care.
Payers certainly don’t pay doctors or nurses for the substantial phone time, emails, and faxes that each OPAT patient generates. This may motivate some doctors to schedule unnecessary outpatient visits for these cases — otherwise they’d get nothing.
And since nobody is paying anyone to oversee the care of OPAT patients, there’s often a “Who me?” approach to their follow-up that is neither good for patient care or the morale of their providers.
Or just as bad, there are too many cooks in the kitchen, and no one is quite clear who’s responsible for what.
A recent post on the IDSA website by ID doctor Parker Hudson detailed this thorny issue perfectly:
Our OPAT program spends a disproportionate amount of time trying to track down labs/levels from patients on IV antibiotics who were discharged to SNFs [skilled nursing facilities]. Despite our orders and requests, most of these values are interpreted and managed by medical directors and not sent back to us — the ID docs writing the orders and following up the patients.
What followed were literally dozens of comments from other ID doctors with similar problems, problems we certainly experience on a daily basis with our OPAT program as well.
To illustrate the complexity, here’s a case — and then a very simple poll.
A 57-year-old man with diabetes and chronic renal disease is referred for admission by his primary care provider (PCP) with 2 weeks of progressive back pain, and found to have spinal osteomyelitis secondary to MRSA. A peripherally inserted central catheter (PICC) line is placed, and because of severe ongoing pain, he is discharged on hospital day 5 to a skilled nursing facility to complete 6 weeks of parenteral vancomycin and to receive physical therapy. At the time of discharge, his ID consultant (who does not do outpatient ID care) recommends that safety labs be done twice weekly, and vancomycin levels once weekly. An outpatient appointment with a different ID doctor is scheduled for 4 weeks later, as well as with his PCP.
Now, take the poll — and if you have a moment, provide the rationale for your answer in the comments section. Bonus points for any practical solutions to the OPAT morass — they would be most welcome!
February 12th, 2018
Shingles Vaccine Video, New Name for C. diff, Flu B Rising, and More — A Pre-Valentine’s Day ID Link-o-Rama
With Valentine’s Day and early spring training baseball both on the horizon this week, it’s obviously time for an extra special ID Link-o-Rama.
On to the links, with a bonus non-ID section and a highly recommended video at the end:
- The ACIP issued its official recommendations for herpes zoster (shingles) immunization. Preferred: the new recombinant zoster vaccine, abbreviated RZV, for people 50 and older. They do not recommend it (yet) for immunocompromised individuals — stay tuned. Does the recommendation include our stable, on-therapy HIV patients, who in increasing numbers are over 50? I say “Yes.”
- The new zoster vaccine is very “reactogenic.” Pain and swelling at the injection site, malaise, generalized aches, symptoms sometimes bad enough to interfere with daily activities. The incidence of these side effects is much higher with RZV than with the live virus vaccine, presumably due to the adjuvant that makes it so immunogenic — and effective. Warn your patients! And as noted above, I strongly suggest all clinicians watch the video, which is embedded at the end of this post — it’s highly informative and useful.
- CDC has issued dietary advice for Valentine’s Day. I’m a huge fan of the CDC, the people who work there, and the excellent work that they do. But boy, this link is no fun at all.
- Multiplex respiratory panels face off in a head-to-head study. Isn’t it extraordinary that we can make a definitive diagnosis of what causes respiratory infections with a single nasopharyngeal swab? Nineteen different pathogens in this particular panel. The key to getting these tests more broadly adopted is decreasing the cost of implementation. Nonetheless, this approach is (in my opinion) the future, especially from a hospital infection control standpoint — even though for most of these viruses, there is no available therapy.
- In this terrible flu season, should we be choosing one type of flu vaccine over another? In the absence of head-to-head trials, it’s difficult to make an official endorsement. But as this interesting piece notes, there are differences between the available vaccines, differences that may lead to different rates of protection. Credit to Helen Branswell, a local journalist who has done superb reporting on the flu this year.
 As the flu season progresses, a higher proportion of cases are due to influenza B. Our local surveillance data mirror this national trend. Good news for those of us who have been vaccinated, as the vaccine appears to be more protective against influenza B than H3N2. And if you haven’t had your vaccine yet, it’s not too late — and please, don’t listen to this advice!
As the flu season progresses, a higher proportion of cases are due to influenza B. Our local surveillance data mirror this national trend. Good news for those of us who have been vaccinated, as the vaccine appears to be more protective against influenza B than H3N2. And if you haven’t had your vaccine yet, it’s not too late — and please, don’t listen to this advice!- More testing for C. diff artificially increases the rate of diagnosis. Nucleic acid testing for C. diff identifies carriers as well as people with the disease — hence the more we test, the more non-disease cases we “diagnose.” This finding is important, as healthcare associated infections such as C. diff are a major hospital quality metric. (Note I avoided writing the full first name of C. diff, very much intentionally as a protest about the discouraging news in the next link.)
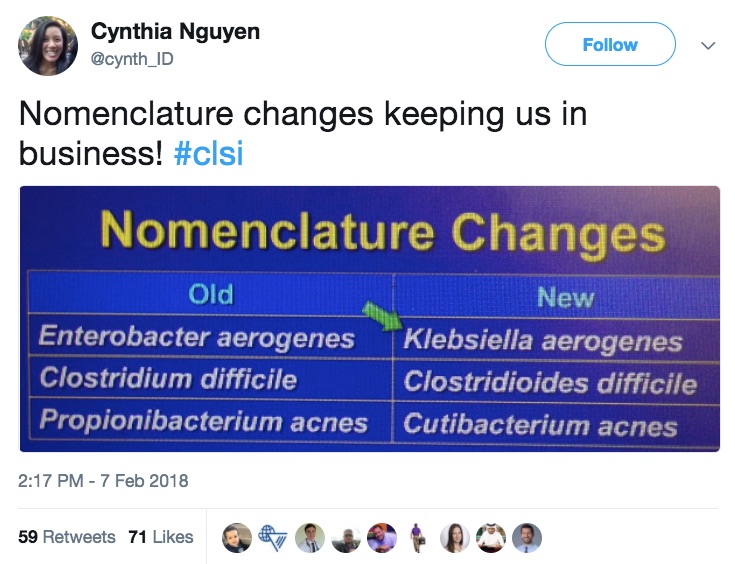
- Clostridium difficile is now Clostridioides difficile. So says the Clinical and Laboratory Standards Institute (CLSI) in an update issued last week. If that’s not bad enough, Enterobacter aerogenes and Propionibacterium acnes also have new names. Sigh. I remember when Stenotrophomonas maltophilia was Xanthomonas maltophilia, those were the days. And whatever happened to Xanthomonas, anyway? Loved that word.
- FDA approves bictegravir/FTC/TAF for initial and switch HIV therapy. Now come two inevitable questions: 1) When will my patient’s insurance/ADAP/etc. cover it? 2) Who came up with that brand name? Biktarvy, jeepers.
- Elsulfavirine, an investigational NNRTI, is also approved for HIV therapy. OK, OK, so it’s approved in Russia, not here. Here’s a clinical trial comparing it to efavirenz from last year’s CROI.
- Adjunctive rifampin does not improve outcomes in MSSA bacteremia. Important negative randomized clinical trial. Although better approaches to this life-threatening condition are needed, imagine if this became standard of care — the drug interaction challenges would be nightmarish.
- Rabies immunizations given in U.S. emergency rooms can be shockingly expensive. Since the ER is where most people go after possible rabies exposures, this cost is an important barrier to a lifesaving intervention. Another excellent example of how our byzantine and opaque healthcare “system” (I use the word loosely) can lead to outrageous charges — the patients are the ones who suffer.
- Streptococcus pneumoniae as the cause of community-acquired pneumonia continues to decline. It’s gone from over 90% in the pre-antibiotic era down to 10–15% today, a remarkable drop attributed mostly to immunization practices. Higher in Europe, where pneumococcal vaccine used less often. Great figure here.
- In a prospective study of community acquired pneumonia, clinical symptoms did not predict etiology or outcome. Seems that the “atypical” in “atypical pneumonia” applies only to the extra-pulmonary manifestations of Mycoplasma (e.g., rash, hemolysis, neurologic disease, et al.) — which are very rare.
- A brief course of empiric antibiotics in the ICU does not appear to cause harm. The study suggests this “just in case” administration of broad spectrum therapy is fine, provided treatment is stopped when cultures are negative, or narrowed once a pathogen emerges — a good role for antibiotic stewardship teams.
- Invasive dental procedures may be associated with a significantly increased risk of streptococcal prosthetic valve endocarditis. The statistical acrobatics done in this complex cohort study notwithstanding, the results suggest a fraction of endocarditis cases are attributable to invasive dental work. The study furthermore found no protection from prophylaxis. However, given the limitations of the observational design, this should not change our practice — prophylaxis for this high-risk group is still indicated.
- More evidence that cefazolin is safer than anti-staphylococcal penicillins. In this meta-analysis of 14 studies, the point estimates all favored cefazolin. It’s unlikely anyone would fund a randomized clinical trial, but that would be most welcome. For now, I am switching patients from oxacillin to cefazolin as soon as bacteremia clears.
Ok, non-ID section — a few medical, one not medical at all.
- Here is a brilliant summary of how doctors assume predictable roles when discussing “code status” with their patients. Several recognizable types here. We can all learn something about improving our approach with this difficult conversation.
- This American wanted narcotics after her surgery in Germany, but all she got was herbal tea. Congratulations to the author for adopting the perfect tone in this very funny commentary — one that says quite a bit about how we ended up in such a mess with opiates in this country.
- Medical students forced to use fax machines are perplexed by this ancient technology. That headline reads like an Onion piece, but it’s true! And when I first wrote about this anachronistic practice over 4 years ago, never did I think it would remain so firmly entrenched in how we communicate. Is there no end in sight?
- A person is ranking all 205 Beatles songs. This effort joins prior similar lists, like this one, of 213 songs — about which I have major disagreements on his rankings. This time the anonymous author is posting a new one almost every day, which adds to the fun. For Beatles fans, be warned — a huge time sink!
Pitchers and catchers, music to my ears!
And take it away, Dr. Fryhofer — nice job on this video!
https://www.youtube.com/watch?v=GTDqY8WM-dk
January 28th, 2018
Apple Wants to Build an Electronic Medical Record — Here’s Where They Should Start
If you want to get a bunch of clinicians riled up — make them really mad — ask them to describe the problems with their current electronic medical record.
So when a company like Apple announces it plans to introduce an electronic medical record of sorts, we should rejoice, right?
This is the company, after all, that leveraged the Think Different and It Just Works slogans to boast about how easy their products are to use.
However, before we can celebrate that a famous tech giant will solve the EMR quagmire, remember that this is the same battlefield that has so far flummoxed Google and, to some extent, Microsoft.
Both those tech giants have struggled to bring sense, accuracy, and usefulness to the chaos of our medical information. The million lines of code written by their software engineers may live somewhere on hard drives and servers, but they are little more than historical records of a failed enterprise.
Think the software equivalent of Napoleon’s invasion of Russia. Ouch.
Given these past lukewarm approaches (some would call them out-and-out failures), I’d recommend that Apple not be too ambitious.
Instead, they should focus on information that is simple, highly useful, and lends itself perfectly to a unified electronic medical record.
Not only that, it’s ID-related. And every clinician and patient will benefit.
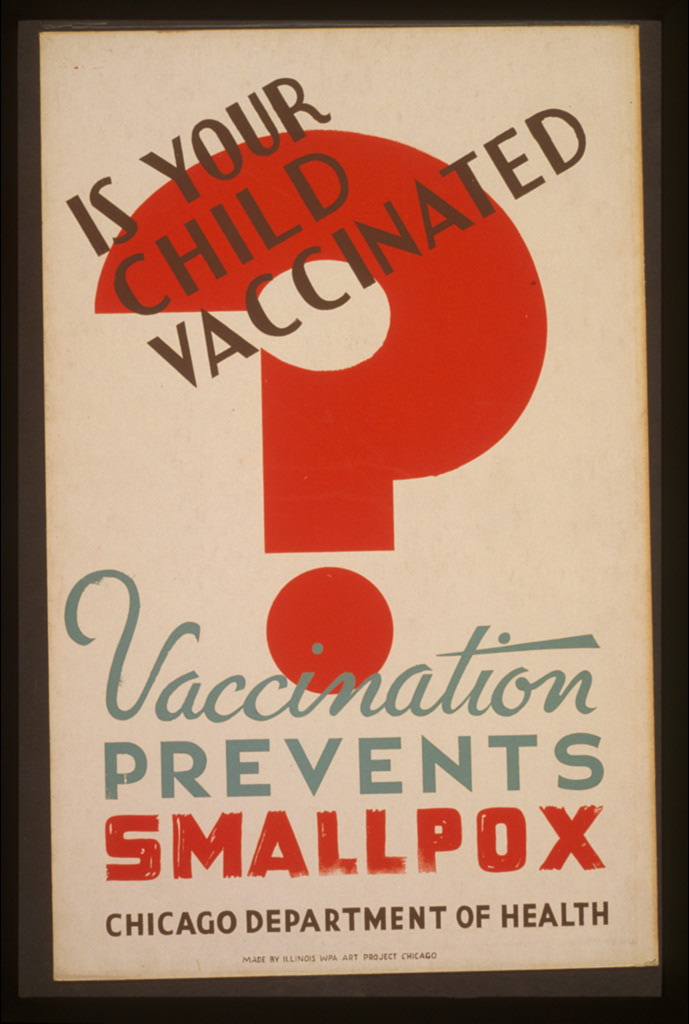
Apple, please build us a Universal Immunization Record.
Here are the features of this must-have service.
- Every person would have access to their record through a user-friendly secure access. No complicated password requirements.
- Information would instantly synchronize across multiple locations, akin to what Dropbox has perfected (and has been widely adopted by other cloud systems).
- Patients would grant access to their clinicians or other vaccine stakeholders (schools, occupational health departments, immigration offices), who would be able instantly to review and to update the information.
- It will be entirely agnostic about operating system, platform, or device.
Just think how care would be transformed with a widely adopted Universal Immunization Record.
- No more ambiguity about school entry requirements or hassles about forms.
- Which pneumococcal or meningococcal vaccine has been administered? Sudden clarity.
- The problem of employee influenza vaccination tracking — solved.
- International immunization records will easily cross borders — no passport required!
- Pharmacy or health department or employer gave your patient a vaccine? No problem, now you can find it.
- Using antibody titers as a marker of prior immunization? A thing of the past — and good riddance, it’s fraught with false negatives.
- Possible vaccine repetition, “just in case”? Whether on the inpatient service, in outpatient clinics, in travel clinics, or in emergency rooms, say goodbye to this wasteful practice.
Apple, you might be tempted to add a few bells and whistles to this straightforward immunization record — say a list of medications, or allergies, or lab results, or surgical procedures, or (heaven forbid), doctor notes.
But you need to walk before you can run, so I strongly suggest you keep things as simple as possible.
Start with the vaccines. Master that first.
You could even argue that, with vaccines so globally valued (minus the anti-vaxxer fringe), that this Universal Immunization Record will be your company’s thank you gift to humankind for buying so many of your products.
A little something you can do with that nearly 1 trillion dollars you have lying around for a rainy day.
January 21st, 2018
Curbside Consults Complex and Silly, the Medicolegal Angle, and a Whole Podcast About Curbsides
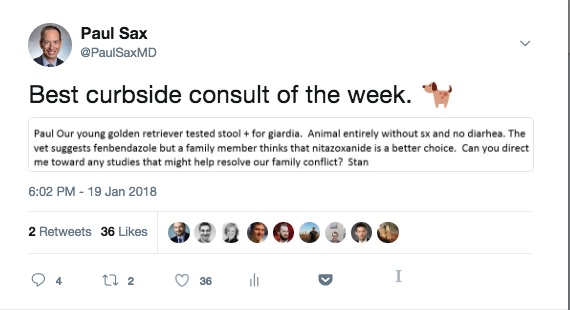
Curbside consults are much on my mind this week for several reasons.
First: I received an extremely complex curbside — a case of an HIV patient (from another state) who experienced treatment failure, had developed multi-class resistance, including integrase resistance (hate that), and now faced a tricky treatment regimen.
The email was a good 300 words long and included 4 resistance reports. Phew.
But what an interesting case! The requester was, to their credit, extremely polite and grateful, which is always appreciated.
Second: Another clinician sent me a curbside that was completely the opposite — something relatively concise, and straightforward, but alas I couldn’t be of much help given the unusual patient profile.
Doubt there will be a HIPAA violation here if I share:
Third: Medscape recently reviewed the medicolegal aspects of curbside consults, an area of significant concern among ID doctors who lead the world in this activity. It’s an excellent, authoritative piece, though unfortunately the net effect could be to make one terrified of providing informal advice to our colleagues — something quite useful both to them and their patients.
Take a look at this definition of a legally safe curbside consult:
A curbside consultation refers to a consultation where the patient isn’t identified; where the specialty physician typically doesn’t review the chart, doesn’t meet with the patient, doesn’t talk to the patient, and doesn’t examine the patient; where the specialty physician doesn’t have any direct or contractual agreement with the treating physician or the hospital where the treating physician is working; where the specialist physician doesn’t bill for his services; and where the treating physician is free to accept or reject the specialty physician’s advice.
Yikes, those are a lot of criteria! Oh well.
Fourth: These general internists do a whole podcast of curbsides, on multiple medical topics — so much so that they call themselves The Curbsiders! No actual patients are discussed, of course, just imaginary ones (and no golden retrievers either).
It’s a terrific show for people in both hospital- and outpatient-based practice, and they invited me on recently to do one on ID Pearls. We covered cellulitis, Lyme, C. diff, flu vaccine, travel medicine, antibiotic allergies — in short, the very stuff we ID docs are curbsided about all the time.
Highly recommended.
Have you listened to our latest episode? ID virtuoso @PaulSaxMD takes us through a wide aria of infectious disease topics.https://t.co/58qrfTHOU0 #FOAMed #infectiousdiseases #puns pic.twitter.com/UL2cPiBiTC
— The Curbsiders (@thecurbsiders) January 16, 2018
January 13th, 2018
Just Wondering: Antibiotics for Cough, PJP vs. PCP, TB-Sniffing Rats, Raw Water, and Other Quick ID Items to Ponder
Just think, by the end of next week, we’ll be nearly 6% done with the new year. How time flies!
For the various items below, if people know the answers, or want to speculate, have at it in the comments section.
- For patients with a nagging cough, what is the median time before they receive an antibiotic? I’m referring to actual clinical practice, also known as “the real world.” And break it down between adults and kids, please.
- And for these same treated patients, what percentage receive azithromycin? One estimate has it as 99.9621%.
- Since vancomycin plus piperacillin-tazobactam increases the risk of acute kidney injury, does this mean less empiric “Vancosyn” in acute care hospitals? Anecdotally, I think it’s having an effect at our hospital — time will tell.
- When will PJP replace PCP as the preferred abbreviation for Pneumocystis jirovecii pneumonia? More and more residents and fellows seem to be using the former, so that day will come soon. Sorry old-timers!
- In low TB prevalence regions, what percentage of patients admitted to the hospital with a low clinical suspicion of TB but who undergo a TB rule out “just in case” actually have TB? One estimate has it at 0.0379% (the inverse of the azithromycin estimate above … shocking coincidence). Only our careful Infection Control colleagues can say if this is worth it.
- When will improved approaches to Lyme testing be available in the clinic? Whether it’s serologic tests, or metabolic changes, or (even better), a reliable PCR or antigen test, here’s hoping this happens soon. Spoiler alert if you haven’t listened to this podcast — and what are you waiting for? — but this is my least favorite test.
- Will the new zoster vaccine be more broadly adopted than our current one? It’s more effective, more cost-effective, and will be easier to store and distribute, but vaccine acceptance is a tricky business. Factors will include ACIP guidelines, cost and insurance coverage, post-approval safety, and marketing — both to clinicians and direct to patients. Speaking of zoster…
- Why do so many patients think you can “catch” a case of shingles from someone else? Not referring to primary acquisition of VZV in a non-immune person — that of course can happen. I mean someone getting shingles (zoster) shortly after seeing another person with shingles. Patients continue to think this even after the whole difference between chicken pox and shingles is explained.
- Did anti-vaccine stupidity reach a new high with this recent Australian case? The father, who had measles as a child, stated he passed on his “natural immunity” to the disease to his children, so they didn’t need the vaccine. Yikes. (H/T to Keith Law for the link.)
- What proportion of ID doctors just say “isavuconazole” rather than the full name, “isavuconazonium”? This critical (and I mean critical) issue came up right after it’s approval, but now that it’s been out for a while, I’m thinking nearly all of us say the shorter “isavuconazole” — which isn’t so easy to say itself.
- Why can’t there be a single meningitis vaccine that includes all five serotypes? No doubt there is some immunologic reason, right? Or is it part of the great conspiracy to make meningococcal immunization guidelines as confusing as possible?
- Does oseltamivir actually work? Depends who you ask. Efficacy debates notwithstanding, we sure use a whole lot of it.
- Is there any medical reason to use the TDF versions of the elvitegravir- and rilpivirine-containing single tablet treatments for HIV? I can’t think of one; always surprises me when encountering someone who hasn’t switched.
- What’s the correct dose of daptomycin? Now for the quick answer: Nobody knows!
- Has the price of any other other oral antibiotic ever dropped as fast, and by as much, as linezolid? A year ago, two weeks of linezolid cost $3600; today it’s $150. Wow.
- How many people need to respond to a piece of academic spam — a bogus meeting invitation, or a predatory journal request for submissions — for these emails to become profitable for the senders? There has to be a number, or else this annoying stuff wouldn’t proliferate so wildly.
Per Journal of Infectious Diseases Editor-in-Chief Marty Hirsch, a short list of copycat predatory journals over the years — with my personal, all-inclusive favorite highlighted! #academicspam pic.twitter.com/4Xy7VEpDnw
— Paul Sax (@PaulSaxMD) December 31, 2017
- What’s the best way to explain to patients the difference between “TARGET NOT DETECTED” and “VIRAL RNA DETECTED BUT BELOW THE QUANTIFIABLE RANGE OF THE ASSAY”? There has to be a better way than using these words — especially since the clinical relevance is definitely below the quantifiable range of this clinician.
- Does anyone really understand why ampicillin and ceftriaxone are synergistic against enterococci when given together? The standard explanation is a combination of complete and partial inhibition of various penicillin binding proteins. Confess I still don’t quite get it, since the organism is intrinsically resistant to ceftriaxone, but maybe that’s just me.
- What explains the media fascination with the giant rats that can diagnose TB? Sure it’s interesting the first few times, but it seems we’re treated to a piece on these clever critters on a regular basis. The Guardian is particularly impressed — “Slow news day? I know, let’s run another piece on the TB-sniffing rats.”
- How long before we see a serious infection linked to “raw” water? As with the anti-vaccine movement, this pseudo-scientific effort to replace tap or standard bottled water with “off-the-grid” H2O includes a potent mix of homeopathy, paranoia, marketing, and charismatic zealots, with no political persuasion spared. Buyer beware!
Since we finished with a bit of homeopathy, here are three enjoyable debunking pieces — How to Counter the Circus of Pseudoscience and Top Ten Signs Your Detox May Be a Scam. and (coinciding marvellously with the football playoffs), Tom Brady is Trying to Kill You.
Of course these pieces typically preach to the choir, but they sure are gratifying to read.
And our fungal friend Candida makes a predictable appearance early in the second one!
January 4th, 2018
What’s Your Favorite Diagnostic Test in Infectious Diseases? Another Fantasy Draft
 If you’re wondering what to do while hunkering down during the “Bomb Cyclone,” here’s just the thing — the latest podcast on Open Forum Infectious Diseases.
If you’re wondering what to do while hunkering down during the “Bomb Cyclone,” here’s just the thing — the latest podcast on Open Forum Infectious Diseases.
(Remember — that’s “O-F-I-D”, not “Oh-FID”.)
Again, I welcome my friend and colleague Rebeca Plank, and this time we’re picking our Favorite Diagnostic Tests in ID.
While winter storm Grayson gives us blizzard conditions and zero visibility outside, inside you’ll sip hot cocoa, pull the blanket around your shoulders, and thrill to our selections.
We choose our top 3 favorite tests, our least favorite test, and something we wish we had in clinical practice now that we lack.
Please listen! And let me know:
- Your favorite and least favorite ID diagnostic tests.
- What should we draft next?
Meanwhile, here’s someone who knows what to do today.
https://twitter.com/CUTEFUNNYANIMAL/status/948170043350769664
December 24th, 2017
On-Service Digest, December 2017 — Plus a Holiday Song
You youngsters out there might not believe this, but there was a time when passing out copies of published papers — actual hard-copies — was a major part of the teaching hospital experience.
Now that this tree-destroying practice is over, many still regularly cite published studies on rounds. The goal is to provide some guidance and reason to clinical practice — that has to be better than the less rigorous approach of applying anecdote to an amorphous blob of clinical data.
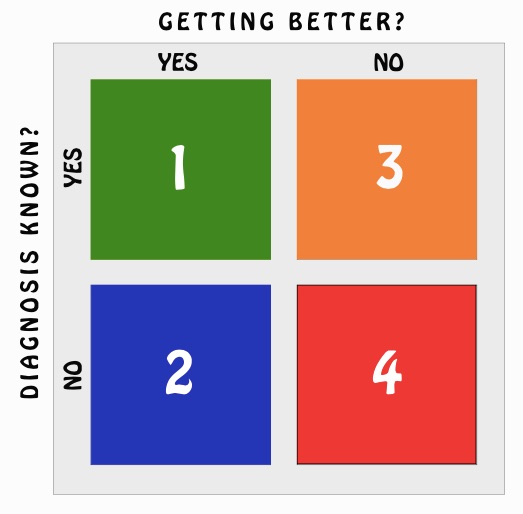
In other words, taking care of patients is hard, and never more so than when seeing ID consults. After all, no one ever consults ID when the diagnosis is clear, the treatment straightforward, and the patient improving.
Remember that at your next salary negotiation!
Here, then, are a bunch of studies that came up in the past few weeks while seeing consults with an outstanding first-year ID fellow — who is now happily away on holiday, and hence might even have the time to read them!
- Penicillin reduces the risk of recurrent cellulitis. In many ways this is an ideal clinical trial. It takes a highly relevant clinical question — should patients with recurrent cellulitis take daily penicillin? — and then answers it in a double-blind, randomized study. The results showed that the penicillin treatment group had nearly a two-fold reduction in the risk of subsequent cellulitis, with no major drug toxicity. This is a particularly useful strategy for patients with recurrent cellulitis due to lymphedema, venous insufficiency, or obesity, infections which are mostly caused by beta strep.
- The optimal duration of therapy for gram-negative bacteremia remains unclear. Amazing how many ID consults focus on this how long should treatment continue question, and also amazing how few controlled studies answer it. So we’ll have to revert to observational studies. Here’s one paper that says 7-9 days is fine for gram negative bacteremia; but here’s another paper that says two weeks is better. Oh well, better consult the rules! And on this topic of treatment duration …
- Four days of antibiotics is just as good as eight for intraabdominal infection, with one big caveat. In contrast to the first study cited above (the penicillin one), this trial is of relatively little use to us ID doctors. And here’s the reason — it included only patients if “they had undergone an intervention to achieve source control.” In other words, these are emphatically not the sort of patients with abdominal infections who need ID consults, and the surgeons understandably rarely ask for our input. Oh well.
- Two-drug treatment with dolutegravir and rilpivirine maintains virologic suppression as well as 3-drugs. This is a particularly useful regimen for hospitalized HIV patients who develop acute renal issues, as both drugs are hepatically metabolized. Importantly, we need to check first that they’re not also receiving PPIs, which are contraindicated with rilpivirine, and that they’ve not failed treatment in the past with NNRTI resistance. And while it’s now available as a single pill, I doubt most hospital formularies are stocking this as of now. The two little separate pills will be just fine until then.
- Mycoplasma has many extra-pneumonic complications. Encephalitis, transverse myelitis, hemolytic anemia, myopericarditis, erythema multiforme, Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis — you name it. Apparently, mycoplasma-related SJS has more prominent mucosal and eye involvement and frequently milder skin findings, prompting the designation of “Mycoplasma-induced rash and mucositis” or “MIRM”. Who knew?
- Oxacillin/nafcillin vs cefazolin for serious Staph aureus infections: The Debate Continues. On the one hand, there is the “cefazolin inoculum effect” of the staph beta lactamases, which theoretically could reduce cefazolin activity more than oxacillin/nafcillin in high-burden infections. Certain cases suggest this might be clinically relevant. On the other hand, there are several uncontrolled studies (here and here for example) showing that outcomes of long-term cefazolin treatment is better than oxacillin/nafcillin. Plus, cefazolin is better tolerated, and much easier to administer. Randomized clinical trial, anyone? Until then, perhaps the optimal approach is to use oxacillin initially, then switch to cefazolin once the infection is controlled.
- Primary prophylaxis for M. avium complex is still recommended in the DHHS Guidelines, but not the IAS-USA Guidelines. My take? There has never been a study of primary MAC prophylaxis in the ART era, and furthermore we want to avoid azithromycin monotherapy in someone with undiagnosed MAC, right? So count me on the IAS-USA Guidelines side. More on this issue here.
- There is still no better paper on ICU Infectious Diseases than “Fever of Too Many Origins.” I’ve covered it before, but it’s worth revisiting this outstanding perspective every so often. It brings some sanity to this challenging endeavor of seeing febrile patients in the ICU, or at least provides a group therapy session. It’s brilliant, so read it!
Happy Holidays! Please enjoy my favorite seasonal song that, in contrast to many other of the other ubiquitous holiday tunes, does not grow tiresome on repeated hearing.