An ongoing dialogue on HIV/AIDS, infectious diseases,
April 5th, 2017
Here’s What Happens When You Search “Infectious Diseases” on a Stock Photo Site
Everyone knows a stock image when they see one. The people don’t look real, the activities are staged, and everything has an air-brushed, frozen quality that screams, “This is not a real thing, but we need some copyright-free graphics and this is the best we can do.”
Strangely depersonalized group photos, animals in human activities, and computer-created illustrations just one step up from Clip Art dominate the stock image sites.
Take this one, for example:
Who are these people? They’re in a boring white room, so why are they so happy? The woman on the far left, where did she get that hat? Is that dog as uncomfortable as it looks? The jeans — are they truly worn out like that, or is this a Photoshop acid-wash effect? What’s with the guys and the tongues?
Anyway, thanks to the largesse of the the generous publishers of this site — who are far more famous for their signature product, abbreviated N-E-J-M, than for this silliness — I have access to tons of stock photos. Literally 69 million, if you believe the banner on my (secret) source.
Now 69 million images is a lot to get through, especially if you have to milk the cow, pick up the kids after school, make dinner, and save that poor little dog from that black-hatted woman’s evil clutches.
Fortunately, there’s also a search box to help narrow down things a bit.
And just for fun, I searched “Infectious Diseases”. Here are a select few from the 10,737 that popped up with this query.
Let’s lead off with one for the children:
- Hmm, what have we here? Two kids (assume they’re kids) playing outside on grassy lawn, sharing … “infectious diseases” (lower-case). All in the same cartoon word balloon.
- Is this a harkening back to the days of Chicken Pox Parties? Imagine the Evite.
- Come to think of it, those virions look very influenza-like — let’s hope they’re not H7N9.
- Of course the kids are happy because they’re developing a healthy immune system. More support for the “hygiene hypothesis”!
- Note the hat on the kid on the right, who has chosen a very old fashioned way to dress up as a nurse.
On to Image #2, a workplace scene:
Scene: Inside an office park, Somewheresville, USA. Three young, attractive professionals are walking down the hall reviewing a very important contract, which is kept in a red folder. The topic shifts to their colleague Matt, whom they spot in the distance.
KARLA: Hey, there’s Matt! Can we hide? He has the nastiest cold.
JEFF: I know. I have the cubicle next to him, it’s disgusting. I hear him expelling gunk from his sinuses every five minutes.
CRISTIN: Isn’t there anything we can do?
KARLA: Remember when they thought a camel had MERS in our local zoo? I still have the masks they gave us.
JEFF: Great idea, Karla!
CRISTIN: Here he comes — quick, pass them out!
Matt approaches, and all three put on their surgical masks. He then sneezes noisily into his handkerchief. Screen fades to black.
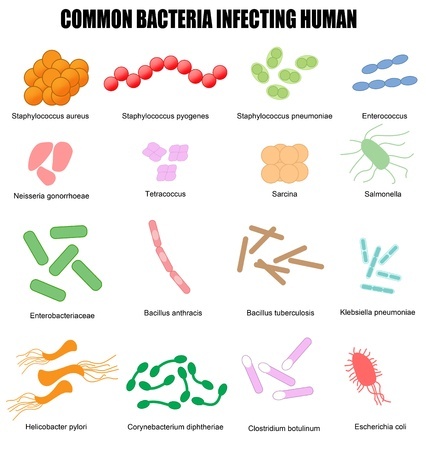
Now for #3, an educational graphic:
Courtesy of a graphic designer named “Roxanne”, I bring you this educational chart, described by her as a “Vector illustration intended for basic medical education (clinics & schools).” But before you use it, here are few important corrections, courtesy of a pedantic specialist in Infectious Diseases.
- Change the title to “Common Bacteria Infecting Human Beings” or “…Infecting People“. English, you know.
- For bacteria #2 and #3, it’s Streptococcus not Staphylococcus. C’mon Roxanne, you knew that.
- “Tetracoccus” and “Sarcina” as “Common Bacteria Infecting Human (Beings)?” You might need Dr. Google to help identify these two (I did), as both are exceedingly rare human pathogens. In other words, they will not be on your ID boards.
- If Bacillus tuberculosis is a name for Mycobacterium tuberculosis anywhere on the planet (besides this poster), this is the first I’m hearing of it.
And Roxanne, after you make those corrections, you can send the royalty check to my home address.
Wrapping up with #4:
… and #5:
Yuck. Highly unlikely we’ll be seeing either of these images on a T-shirt or mug anytime soon.
But maybe that’s just me.
March 25th, 2017
HIV and Hepatitis C Are No Longer the Most Serious Infectious Threats to People Who Inject Drugs
 I had dinner with my daughter Mimi the other evening, and was ruminating about how things have changed since I started work as an Infectious Diseases doctor around 25 years ago.
I had dinner with my daughter Mimi the other evening, and was ruminating about how things have changed since I started work as an Infectious Diseases doctor around 25 years ago.
Here’s an excerpt of our chat:
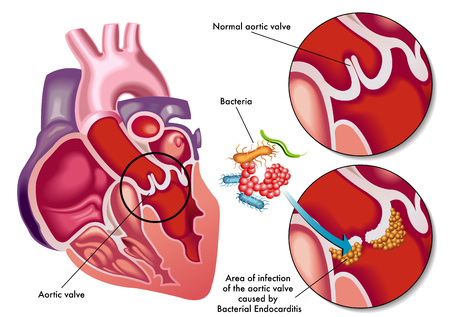
Me: There are way more cases of endocarditis in young people than there used to be, a complication of injecting drugs. People in their 20s and 30s with life-threatening infections, getting admitted to the hospital, needing antibiotics for weeks, sometimes surgery … it’s awful. [I didn’t mean for this to sound like a cautionary speech to my 21-year-old daughter, but reading it now — guilty as charged.]
Mimi: Endocarditis?
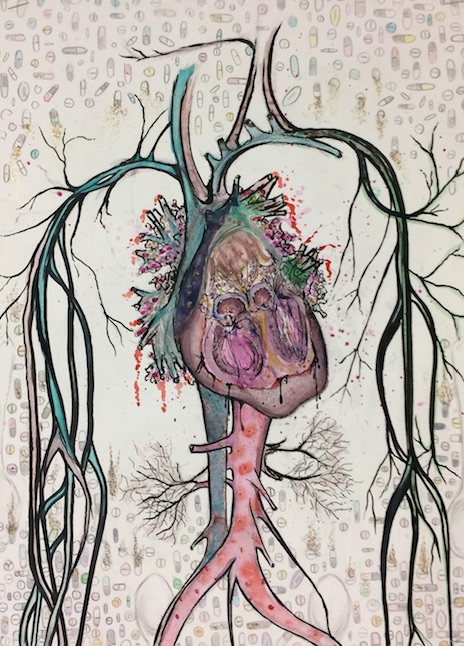
Me: Infection of the heart valves. It’s an incredibly serious problem, much more difficult to treat than HIV and HCV. Even with our best antibiotics, some people need major heart surgery — their lives are never the same. And sometimes the infection spreads through the blood to the lungs, spine, brain… Some even die!
Mimi: I’ve never even heard of it. And we never covered it in high school, and we had a ton of drug talks in health classes. It was all HIV and hepatitis. And overdoses, of course.
Me: Trust me, it’s a terrible problem.
Mimi: I bet if I asked 10 of my smartest friends, most would be like, “What?” Hey, I can’t even remember what you called it, and you just told me. Here, let me check something. What’s the infection called again?
Me: Endocarditis.
Mimi [takes out her phone, does some rapid-fire tapping]: Just did a Google search. “Endocarditis and injection drug use” has 179,000 hits, “HIV and injection drug use” has 1.6 million. And most of the endocarditis ones are in medical journals. Only doctors are going to read those.
Me: How do we get the word out?
Mimi: It needs a better name. Something like Zika — everyone can remember that.
Me: Can I steal that line?
Mimi: Provided there’s proper attribution, go right ahead!
For some context, Mimi is a college junior and, while not medical school-bound, is a smart kid. (Of course she is.) Having grown up with two doctor parents, she probably has a better than average fund of medical knowledge for her age.
But the above conversation exposes a major gap in the lay public’s understanding of the risks of injection drug use — one hinted at recently in a piece on the clinical and ethical challenges of heart surgery for people with addiction.
For whatever reason, endocarditis and other invasive bacterial infections are not nearly as feared as HIV and HCV, despite the fact that the former are far more immediately life threatening and way more difficult to treat.
It’s true even among those who have had endocarditis. One woman told me that the most upsetting part of her prolonged admission (complicated by cavitary lung lesions and spine infection at multiple levels) was not the days of fevers, the pain when breathing, the severe back pain from the infection, back pain that still plagues her.
It was when she found out her hepatitis C test came back positive.
Let’s compare:
- Endocarditis due to Staph aureus: Prolonged hospital stay; 6 weeks of intravenous antibiotics; metastatic infection in the lungs and spine; possible need for valve replacement surgery; possible death.
- Hepatitis C: 12 weeks of one pill a day. Even if untreated, unlikely to cause problems for decades.
Of course HIV is incurable, unlike endocarditis — but it too is treatable with 1 or 2 pills a day, treatment that essentially eliminates the chance of getting sick from AIDS. And in the United States, rates of HIV due to injection drug use are way down despite the opiate epidemic, accounting now for only 6% of new cases.
So why do we have this strange paradox? And does endocarditis need a new, more memorable name? Suggestions welcome.
And remember, Zika is taken.
(Second image courtesy of Kelly Beverly, “Infective Endocarditis”.)
March 19th, 2017
What Health and Human Services Secretary Tom Price Should Be Saying About Required Immunizations
In case you missed it, Secretary of Health and Human Services Tom Price said this past week that the states should make decisions about mandatory vaccination policies.
Here’s the actual clip:
HHS Secretary Tom Price says it should be up to states to regulate whether immunizations are required https://t.co/soyH0YpO5E
— CNN Politics (@CNNPolitics) March 16, 2017
What’s notable here isn’t the content of what he says — the states already make immunization policies — but that he seems to be so carefully parsing his words.
Of course, his reticence might be the result of his belonging to the Association of American Physicians and Surgeons, a group with strong opposition to mandatory immunizations. Or perhaps it’s the well-known views of his boss, who has publicly expressed he’s not so sure about vaccine safety, especially regarding the link to autism.
So in that spirit, if Price is feeling hesitant about expressing his own views, I’m going to offer him some alternative responses to Wolf Blitzer’s queries (plus a few more questions I’ve made up).
Price is, after all, an orthopedic surgeon. Some input from an ID doctor might be welcome, akin to how we assist them in managing a septic hip.
Blitzer: So you believe in immunizations, you believe all children should get a shot for polio, and other diseases?
Neo-Price: Absolutely. We in the Department of Health and Human Services strongly support the state policies that require childhood immunizations. These policies have had a miraculous effect in reducing illness and death, particularly in children, and greatly improve public health for all. Some prevent cancer. They even save money! Talk about a win-win-win-win.
Blitzer: There are some people who argue that it should be up to the parent or parents to decide what’s best for their child. What do you say to them?
Neo-Price: When a policy is good for both the individual child and for society, we have to be firm that it’s enforced. And a critical component of vaccine effectiveness is herd immunity, especially with the most contagious infections such as measles. If we let immunity decline too much in the community, these infections will come roaring back. Let me show you this extraordinary short video:An excellent gif for visualising herd immunityhttps://t.co/OfTnj7HRcH pic.twitter.com/esJN2MKr30
— Educake Science (@educakescience) March 6, 2017
Blitzer: I hear there has been an increase in so called “nonmedical vaccine exemptions” in the United States. What are your thoughts on these?
Neo-Price: Frankly, each nonmedical vaccine exemption is essentially a misguided, selfish decision made by a parent at the expense of both the child’s health and public health. They should be more than strongly discouraged — they should be abolished.
Blitzer: Well said, Secretary! I assume, then, that you do not believe in the link between vaccines and childhood autism.
Neo-Price: Emphatically not. Vaccines are remarkably safe. After the fraudulent paper linking vaccines to autism was published, a torrent of scientific data subsequently found no such link. And the paper, as you know, was subsequently retracted by The Lancet. It’s garbage science.
Blitzer: One last thing before you go — there are some who say the vaccine policies are being set by individuals who have hidden agendas — conflicts of interest with the pharmaceutical industry, or with insurance companies, or are just ivory tower academics who don’t understand “real” people.
Neo-Price: The Advisory Committee on Immunization Practices (ACIP) — which is organized by the Centers for Disease Control, a wonderful government institution — is a prime example of how doctors, scientists, and public health officials can come together for the public good. They carefully review the vaccine safety and efficacy data, and then issue policies that are broadly endorsed. It’s about as good an example as you can find for your tax dollars well spent. Makes me tear up a bit with patriotism just thinking about it.
Blitzer: Thanks very much, Secretary. This has been most educational.
Neo-Price: Thank you for having me on. And let me know if you have any questions about your ACL repair. I am an orthopedic surgeon, after all.
My hunch is that Price will appreciate my articulating his position on vaccines more clearly. You’re welcome.
If not, I’d better watch out — orthopedists are much bigger than ID doctors.
Save
March 14th, 2017
Poll: Should We Allow 24-Hour Shifts Again For Interns?
 Over on Boston’s NPR site, I wrote a piece about the decision by the Accreditation Council for Graduate Medical Education (ACGME) to allow 24 hour (or longer) work shifts again for interns.
Over on Boston’s NPR site, I wrote a piece about the decision by the Accreditation Council for Graduate Medical Education (ACGME) to allow 24 hour (or longer) work shifts again for interns.
My goal in writing the piece was to relay what I experienced doing these long shifts way back when during my internship — the good and the bad.
Not surprisingly, most of the comments I’ve received from non-MDs are highly skeptical that there could be anything good about working such a long shift. And if you listen to the linked radio segment on the site, you can sense the incredulousness of the hosts, neither of them doctors. Their tone is practically dripping with, “You’ve got to be kidding me.”
From my friends and colleagues in medicine, however, what I wrote seems to have resonated — here are a few of the emails I received:
“Great piece on 28 hour shifts! Wonderful description of our days as interns. Forwarded to my daughter who is in her third year of med school.”
“Paul, I loved reading your piece. I had the same set of experiences and thought you captured the highs and lows perfectly. Thanks!”
“GREAT piece…I wish I could call you ‘old’ [ahem] but, alas, that was me in that description of internship too.”
“Your article – truly wise and wonderful, by far the best treatment of such a complicated topic that I have read, ever (I crossed out in years).”
“Spot on, Paul! We learned the cycle of illness, both to recovery or to progression of disease. And, we were the patient’s doctor from day one.”
I don’t cite those just to toot my horn (obviously that’s a little bit of it), but also to emphasize that this experience we had with long shifts wasn’t exclusively terrible. Some good came out of it as well.
But did these positives actually outweigh the very substantial negatives, which I also outlined in that piece? I just don’t know, and hence am not sure if the ACGME should be applauded for allowing more flexibility in training, or — and this is the mainstream view — should they be criticized for bringing back work shifts that put patient safety in jeopardy?
Since I’m now back with this readership, I’m dying to know what you think. Based on the NEJM Journal Watch sophisticated reader metrics, you are predominantly practicing clinicians — doctors, nurses, PAs. And we also know that 22% of you have dogs, 14% cats, 6% both, and 0.0412% have ferrets. (Yuck.)
Please read the piece, vote in the poll below, and feel free to provide your comment or comments. We’ll stratify the results by pet ownership.
Thank you.
March 5th, 2017
High-Dose Flu Vaccine, Robert De Niro Challenge, Antibiotics for Colds, and More: March Comes in Like a Lion ID Link-o-Rama
 Here are a few ID/HIV items blowing around the neighborhood on this, a bitterly cold and windy first weekend of March (at least here in Boston):
Here are a few ID/HIV items blowing around the neighborhood on this, a bitterly cold and windy first weekend of March (at least here in Boston):
- Compared with the standard dose vaccine, the high-dose flu vaccine reduced deaths among older adults. The benefit was seen in the 2012-13 flu season, but not 2013-14. The authors speculate that the circulating strain (H3N2) and low overall effectiveness in 2012-113 explain this discordance. Notably, ACIP still does not formally endorse any particular vaccine for the elderly, but I’m becoming a believer in the high-dose strategy.
- A mother recounts her experience raising a child with congenital CMV infection. This is a skillful and moving description of congenital cytomegalovirus, and the strange obscurity of the virus that “causes more birth defects in the United States than any other nongenetic disease.” That it remains so relatively unknown is a perplexing paradox (especially in the Zika era) — one she artfully explores.
- There’s an estimated 20-fold increase in certain birth defects in pregnancies with Zika infection. Approximately 6% of the babies had microcephaly, neural tube defects, eye defects, or other central nervous system (CNS) problems. Long term follow-up, of course, may identify additional abnormalities.
- Not all infections related to thorn injuries are sporotrichosis. In fact, the number of sporotrichosis cases in this series of over 1000 patients with thorn injuries was (wait for it) … zero. Oh well, guess common things are common.
- Does our president have neurosyphilis? Yes, syphilis is the “great imposter”. Yes, it sometimes can be difficult to diagnose. Yes it can cause bizarre behavior. But good grief, this is an extreme form of medical speculation. For the record, 5 different people sent me this link (you know who you are).
- This site catalogues all the major HIV clinical trials. Under the direction of François Raffi, Anton Pozniak, and Pedro Cahn, ARV-Trials.com is helpful source if you can’t remember the difference between the MERIT, MOTIVATE, MONET, MONOI, MONARK, and MODERN studies. Of course you remember all the ACTG study numbers — but if not, you can find them there too. Site is also kind of a throwback to 1990s web design, in case you’re feeling nostalgic.
- Drug development for hepatitis C is a risky business. Not only that, even established “blockbusters” face declining sales. Incentives in our healthcare “system” can sometimes be truly perverse — and boy, is this cartoon apt. (And brilliant.)
- Vancomycin is better than metronidazole for C diff — again. I can’t think of any reason to use metronidazole for patients who actually have C diff, the real thing. Those who are just PCR positive with minimal symptoms — which really should be called pseudo-C diff — usually don’t require any treatment.
- RFK Jr and Robert De Niro offered $100,000 to anyone who can prove vaccines are safe. Darn, this pediatrician has already nabbed the prize. Guess De Niro has already made Raging Bull, now he’s making Raging Bulls–t.
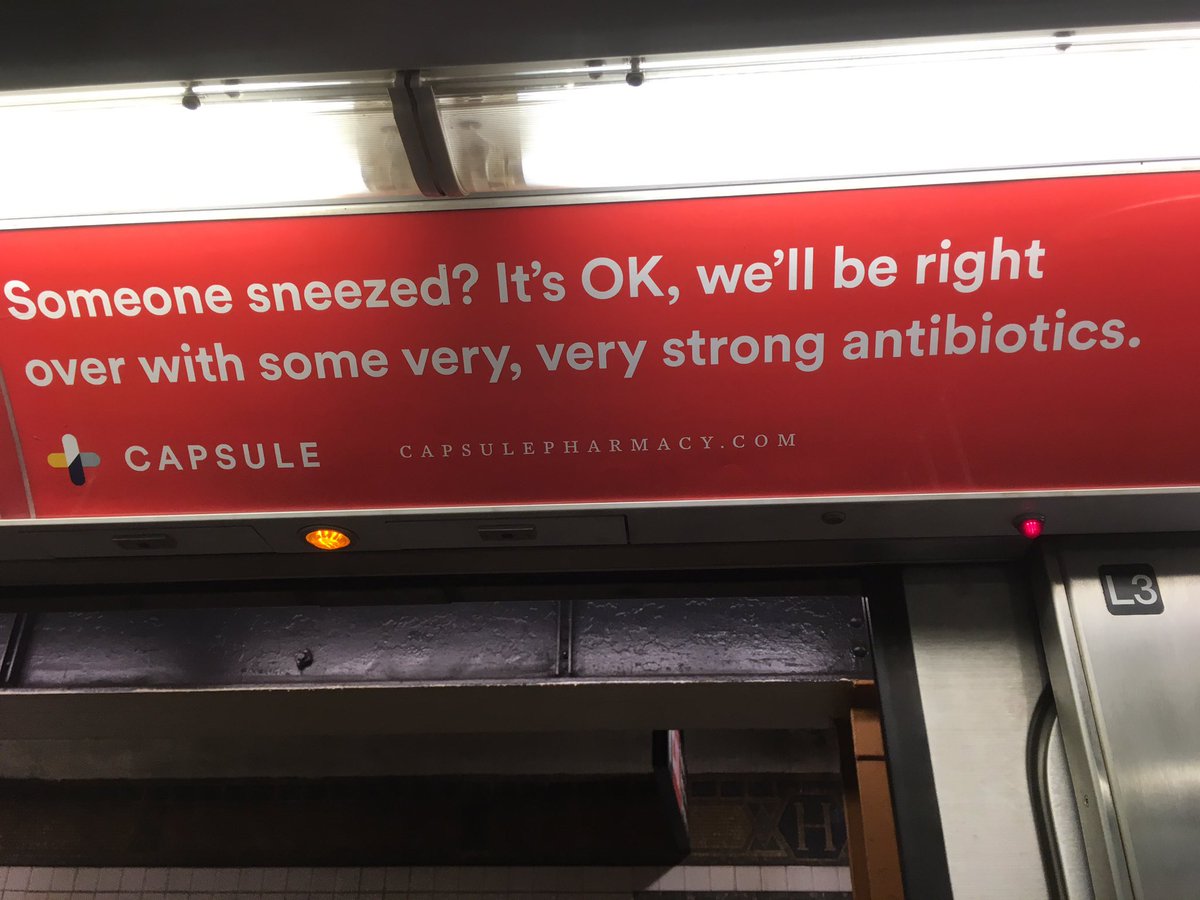
 This pharmacy’s ad campaign on the NYC subway advocates “very, very strong antibiotics” since “someone sneezed.” News flash: Antibiotics don’t work for colds, no matter how “strong” they are. See image at top of this post, proving that I didn’t make that up. And it looks like another one of their ads isn’t too popular right now either. I love you too, by the way.
This pharmacy’s ad campaign on the NYC subway advocates “very, very strong antibiotics” since “someone sneezed.” News flash: Antibiotics don’t work for colds, no matter how “strong” they are. See image at top of this post, proving that I didn’t make that up. And it looks like another one of their ads isn’t too popular right now either. I love you too, by the way.- Here’s an interview with Dr. Brad Spellberg on the importance of antibiotic stewardship. He’s one of the top figures in this field right now, and is very compelling on the subject. Imagine a world where all antibiotic use in the hospital is restricted to ID approval, analogous to chemotherapy for oncologists. And no, he wouldn’t like those NYC subway ads either!
- Short-course empiric gentamicin added to broad spectrum therapy for patients with sepsis did not improve outcomes. Gentamicin-treated patients did have more acute renal injury, even though the median duration of therapy was only 2 days. This was once a common practice in our hospital, where one of our residents used to call it “death gent”, for obvious reasons. Seems now we can all stop doing it!
- Yes, there’s an E. coli O157:H7 outbreak linked to a product called “I.M. Healthy.” It’s soy nut butter, in case you were wondering. No word on the company’s web site whether the post-recall I.M. Healthy will be called “I.M. Now Healthier.”
- Matt Iseman won Celebrity Apprentice. And why, you must be wondering, is that being mentioned in an ID blog? Turns out he’s the son of Mike Iseman, the noted tuberculosis expert. And before he (Matt, not Mike) became a comedian, he had another job.
Only 28 days until Opening Day!
(Hat tip to Chuck Daley for this last item.)
February 26th, 2017
Improving Outcomes with ID Consultation: Three More Papers For the Collection
 Several years ago, one of my very brilliant colleagues posed an interesting question.
Several years ago, one of my very brilliant colleagues posed an interesting question.
Why do ID specialists even exist?
“After all,” he said in an accent that happens to be a distinctive mix of several former British colonies. “There is nothing we do that other doctors couldn’t also do, provided they had the motivation.”
He had a point — with no required endoscopic tool, special catheter, expensive imaging device, or other arcane gizmo, the basics of ID clinical practice are available to everyone:
- Take a careful history. And I mean careful. Read this.
- Do a targeted exam. Self explanatory.
- Meticulously review the available data. OK, obsessively review it, to the point of almost meeting DSM criteria. Turn out the lights when you’re done, it’s getting late.
- Communicate with everyone. Go to radiology and review the films. Look at the ECHO with the cardiologists. Ask the surgeons what they saw in the OR, what they did, and why. Use your friends in the microbiology lab to make you look smart — same with the pathologist who interpreted that biopsy. Call the referring doctors to get their thoughts. Get permission to check with the wife or husband or sister or brother or son or daughter or friend about what they think is going on. If it’s some obscure infection, reach out to the local/national/international expert and find out what he or she would do. Folks, this stuff is gold.
- Put it all together. Voila, the assessment. Say what you think is going on, and why. Use all your internal medicine training, because not everyone with a fever or an elevated white blood count has an infection, not everyone with a red leg has cellulitis. Best if these impressions are relayed directly — in spoken words — to the consulting clinicians, and then concisely summarized in the note.
- Make clear recommendations. Start with the diagnostic tests, then the therapeutic recommendations. Put it in list form to make it easy to follow.
- Collect your big paycheck. Kidding.
Back to my colleague’s point — any clinician could do these things.
But since items #1-6 above are our standard operating procedure, and we want to justify our existence, there’s a growing body of literature that correlates care provided by ID doctors with better outcomes.
And recently we have three more to add to the pile:
- Infectious diseases specialist management improves outcomes for outpatients diagnosed with cellulitis in the emergency department. That’s the title of the paper, which sums up the findings nicely. In more detail, ID care was associated with lower likelihood of recurrence, of hospitalization, and receipt of less empiric broad-spectrum therapy. And here’s a bonus — the ID consultants “identified cellulitis mimickers allowing for care of the true issue.” Love that.
- The more ID doctors living in a region, the more likely a patient will avoid amputation for diabetic foot ulcers. I like the fact that the authors used “geographic density” of ID doctors, as this accounts for both formal ID consults and the informal advice given to clinicians, something we do frequently. How to summarize this benefit? Here’s one amusing way:
- In cryptococcal infection, ID consultation is associated with improved survival. In this retrospective cohort of non-HIV related cryptococcal disease, mortality was 27% for those with ID consultation, versus 45% for those without — even though patients with ID consults had a higher fungal burden and were more likely to have CNS disease. (Quick query — given the inevitable complexity of cryptococcosis, can you imagine not wanting an ID consult? Jeeze.)
A couple of final thoughts about these studies.
First, note that these three papers span very different aspects of ID cases — the routine (cellulitis), the common but complex (diabetic foot ulcers and osteomyelitis), and the rare but life-threatening (cryptococcal disease).
Second — aren’t we’re lucky to have have such a diverse, interesting field?
Hey, it’s Oscar Night! Miss this guy:
[youtube https://www.youtube.com/watch?v=AH46OAmKNCw&w=560&h=315]
February 19th, 2017
Really Rapid Review — CROI 2017, Seattle
 The Conference on Retroviruses and Opportunistic Infections (CROI) returned to Seattle this past week for its 24th meeting. It’s the 4th time CROI has been held in Seattle, an excellent city for a meeting of this size, which includes “only” 4200 people. The convention center is pleasant and user-friendly — big but not cavernous, actually encourages interactions with colleagues — and there are numerous hotels and restaurants within walking distance, plus more Starbucks per square foot than any place on the planet.
The Conference on Retroviruses and Opportunistic Infections (CROI) returned to Seattle this past week for its 24th meeting. It’s the 4th time CROI has been held in Seattle, an excellent city for a meeting of this size, which includes “only” 4200 people. The convention center is pleasant and user-friendly — big but not cavernous, actually encourages interactions with colleagues — and there are numerous hotels and restaurants within walking distance, plus more Starbucks per square foot than any place on the planet.
From a content perspective, the big change for CROI 2017 was the return of numerous studies on antiretroviral therapy, studies involving both approved and investigational agents. The last several years, by contrast, had relative dominance of pre-exposure prophylaxis and hepatitis C studies. With PrEP, one had the sense at the meeting that we’re now waiting for the next strategies (long-acting injectables, for example).
As for hepatitis C, well that’s been all but solved (except for the implementation part). How do you improve on 97%-plus cured. Hooray!
On to the summary, a Really Rapid Review™ of the most interesting studies at the conference (at least from one perspective, ahem). Links are to the conference website (as usual excellent), abstract #’s are in brackets, and be sure to check out some of the oral presentations here. The list is roughly organized into epidemiology/prevention, treatment, cure, and opportunistic infections. Please tell me what I missed in the comments section.
And, because I was involved in a few of the studies listed below, for full disclosure I’ve inserted a special Puppy text emoticon to draw attention to that fact. ੯ੁૂ‧̀͡u (Make sure you click on them. Woof.)
- New HIV infections in the USA continue to decline [30]. From 2008–2014, the annual number of HIV infections dropped 3.6% per year, and the percentage of persons with undiagnosed infection declined at around the same rate. That’s the good news. The bad news is that new infections continue to increase in young black and Hispanic men who have sex with men. For the record, we’re down to 37,600 cases/year in the USA, and I expect this will continue to drop since PrEP use didn’t really start until 2014.
- Among participants in the HIV Outpatient Study, the proportion of time spent with HIV RNA > 1500 has dropped dramatically since 2000 [31]. This higher proportion of diagnosed, treated, and suppressed patients must be the primary reason why HIV incidence has declined in the USA.
- Doxycyline administered as post-exposure prophylaxis reduced the incidence of chlamydia and syphilis among participants in the IPERGAY PrEP study [91LB]. No effect on gonorrhea. Significantly more GI adverse events in doxycycline recipients. Interesting results — but definitely not enough evidence yet to make this a policy recommendation, a fact stressed by the lead author, Jean-Michel Molina.
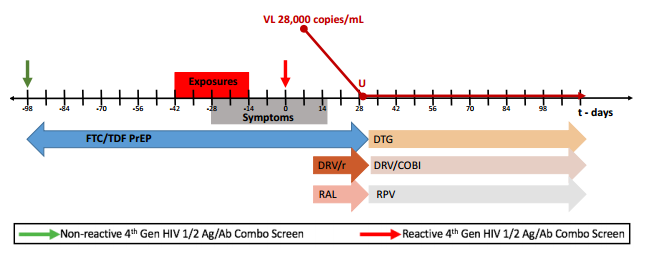
- A case of PrEP failure occurred despite good adherence and no transmitted resistance [953]. The case illustrates the likely importance of “inoculum” in PrEP failure — the person had a very high number of potential exposures. It’s worth looking at the full poster presentation, as the clinical and laboratory manifestations of acute HIV infection were unusual, possibly influenced by being on TDF/FTC.
- In treatment-naive patients, the investigational NNRTI doravirine was non-inferior to boosted darunavir [45LB]. 84% vs 80% < 50/copies at week 48, with a trend toward doravirine being better with very high (>500,000) baseline HIV RNA. Favorable aspects of this treatment included once-daily dosing, few CNS side effects, and a better metabolic profile that darunavir. Only 1 of 364 doravirine-treated patients developed resistance, a low number for NNRTI strategy; none did in the darunavir arm. And note the abbreviations — “DOR” vs “DRV”! A coforumulated DOR/TDF/3TC tablet is in development. ੯ੁૂ‧̀͡u
- In virologically suppressed patients with no history of resistance, dolutegravir plus rilpivirine maintained virologic suppression as well as continuing current therapy [442]. 95% < 50 in each study arm at week 48. Only one of 513 patients in the DTG + RPV arm failed with resistance (she clearly stopped therapy). There was a slightly higher rate of discontinuations due to adverse events in switchers (3% vs <1%), likely at least in part due to the open label design. Note that this is a rare success for an NRTI-free treatment strategy, a fact emphasized by Jose Arribas in his outstanding oral presentation on treatment simplification. A coformulated DTG/RPV tablet is in development, to be used in follow-up studies.
 In a phase 2 double-blind clinical trial, bictegravir + TAF/FTC was comparable to dolutegravir + TAF/FTC [41]. Responses 97% and 91% at week 48, respectively; more details in the published paper. Bictegravir is an investigational once-daily, unboosted integrase inhibitor with activity against wild-type and most resistant viruses and few predicted drug interactions. A coformulated BIC/TAF/FTC tablet is in development — and being used in the phase 3 program, which is fully enrolled. ੯ੁૂ‧̀͡u
In a phase 2 double-blind clinical trial, bictegravir + TAF/FTC was comparable to dolutegravir + TAF/FTC [41]. Responses 97% and 91% at week 48, respectively; more details in the published paper. Bictegravir is an investigational once-daily, unboosted integrase inhibitor with activity against wild-type and most resistant viruses and few predicted drug interactions. A coformulated BIC/TAF/FTC tablet is in development — and being used in the phase 3 program, which is fully enrolled. ੯ੁૂ‧̀͡u- In a single-arm study, dolutegravir plus lamivudine maintained virologic suppression [458]. Study included 110 patients with no history of failure and who tolerated an 8-week “lead in” of DTG + 2NRTIs first. One virologic failure (no resistance), one almost failure with low-level viremia. Comparative clinical studies ongoing. Study is called “LAMIDOL”, which sounds like a skin cream.
- Dolutegravir monotherapy increases risk of virologic failure and resistance [451LB]. So we now have several studies that show this strategy to be a bad idea. To quote the abstract: “The genetic barrier of DTG monotherapy is insufficient to allow for maintenance monotherapy.” Here are more details on the resistance pathways in several other studies. Let’s stop doing this, ok? Thoughtful editorial to this effect by Joel Gallant says the same thing, though much more eloquently.
- Transmitted drug resistance did not reduce antiviral efficacy in this large treatment study [43]. This is a surprising finding, as several prior studies have shown that transmitted NNRTI resistance does reduce the activity of these regimens. One possible explanation is the greater potency of TDF/FTC vs AZT/3TC.
- Case report of DTG resistance in a treatment-naive patient [500LB]. Baseline HIV RNA 1,970,000 and CD4 78. The fact that CROI accepted a single case of this event shows how incredibly rare this is.
- Darunavir but not atazanavir associated with an increased risk of cardiovascular events [128LB]. It’s a DAD analysis, and the effect (a 53% increase) was comparable to lopinavir and indinavir. Is this a class effect, ameliorated by atazanavir’s bilirubin-raising properties?
- More discontinuations due to neuropsychiatric side effects on DTG than RAL or EVG/c [651]. Concomitant ABC/3TC with DTG appears to be a strong contributor. Note that rates of d/c due to adverse events overall did not differ between the drugs.
- High DTG plasma concentrations associated with more neuropsychiatric adverse events [426]. Study done in Japan — could tolerability be linked to BMI or pharmacogenomic issues?
- More adverse events in EFV rapid metabolizers [384]. Study done in Botswana, and runs counter to analysis of suicidality done in (mostly) US-based studies, where those with genotypes associated with slow metabolism appeared to be at higher risk.
- EFV use as a first-line agent in the USA has dropped dramatically [454]. Now less than 10% start it as first line, a stark contrast from the pre-integrase era.
- TAF superior to TDF after 144 weeks [453]. The most important safety finding is that 0/866 on TAF vs 12 (11 if you remove “bladder spasm”)/867 on TDF developed clinically significant renal issues, a difference that is highly statistically significant. ੯ੁૂ‧̀͡u
- Resistance to integrase inhibitors remains extremely rare [478]. In a 9 site survey, baseline (transmitted) integrase resistance was 0.04%; post-treatment was 0.4% — both very good news.
- Should we be sending baseline integrase genotypes before starting therapy [493]? Based on this modeling study, the answer is a resounding NO, for three reasons: 1) the prevalence of transmitted integrase resistance is fortunately still very low (see above); 2) DTG-based regimens will likely succeed even when resistance to first-generation INSTIs is present; and 3) even if virologic failure occurs, it will delay use of a salvage regimen only briefly. ੯ੁૂ‧̀͡u
- Many novel drugs in various stages of development. These include (deep breath) ibalizumab [449LB] (anti-CD4 monoclonal antibody), PRO140 [437] (different humanized anti-CD4 monoclonal antibody), UB-421 [450LB] (yet another monoclonal antibody that blocks viral entry), elsulfavirine [452LB] (NNRTI with 8-day half-life), MK-8591 [435] (potent and very long acting NRTI), GS-PI1 [433] (an unboosted once-daily protease inhibitor), GS-9131 [436] (NRTI with activity against essentially all NRTI-resistant isolates), and GS-CA1 [38] (capsid inhibitor that in vitro is more potent than any other antiretroviral agents). Wow that’s a lot!
- Even very early HIV treatment does not prevent virologic rebound after stopping ART [124]. Eight started treatment during “Fiebig I acute infection” (VL+, p24-, Ab-), which is known to induce a lower HIV reservoir, yet all rebounded by 9 weeks.
- A prolonged virologic remission in a patient undergoing a stem cell transplant [319]. The patient continued suppressive ART for 784 days after transplant, and had no detectable virus (HIV RNA or DNA) using many techniques. Rebound occurred after 288 days off ART, longer than in the “Boston patients”. Note that donor was CCR5 wild-type, not CCR5 negative.
- Latency-reversing agent plus HIV immunization may induce “viremic control” [119LB]. Strategy tested was “MVA.HIVconsv” vaccination, then three doses of romidepsin, then another vaccination; 5 of 13 maintained low-level viremia after treatment interruption. Importantly, study subjects started ART soon after HIV acquisition, hence were likely to have low viral reservoirs.
- TLR7 agonist induced “viral remission” in two of four Indian Rhesus macaques [338LB]. One of the agents (GS-9620) is currently in human trials.
- Does ART with integrase inhibitors increase the risk of immune reconstitution inflammatory syndrome (IRIS)? The answer is yes, based on two studies conducted in non-TB endemic regions ([731] and [732]). As DTG-based regimens are increasingly adopted world-wide, we should expect IRIS incidence to increase. And count me in the group that thinks this is a good thing — IRIS is a marker for faster virologic response and immunologic recovery. (Not everyone agrees.)
- Pre-emptive prednisone reduced the risk of TB IRIS in patients with advanced HIV disease [81LB]. All patients (CD4 < 100, diagnosed with TB) received ART and TB therapy. The study compared prednisone 40 mg/day for 2 weeks then 20 mg/day for 2 weeks versus placebo. Incidence of IRIS was 47% in placebo arm, 33% in prednisone arm (p=0.02). Incidence of infectious complications or malignancies did not differ between study groups.
- In cryptococcal meningitis, a single high dose (10 mg/kg) of liposomal amphotericin reduced CSF fungal burden as fast as standard dosing (3 mg/kg/day for 14 days) [82]. Based on these encouraging early results, this strategy will be evaluated in a randomized clinical endpoint study.
- Researchers intensively studied 5 patients with paradoxical CD4 decline on suppressive ART [226]. 4 of 5 had CD4 < 50 (other was 74). Unlike immuologic non-response, these patients did not have elevated inflammatory markers or immune activation, but did have higher levels of homeostatic cytokine IL-7. The title says it all: “a novel, rare and perplexing immunologic outcome.” (I’ve seen this once in my career, for the record.)
- For neurosyphilis, intravenous penicillin and procaine penicillin plus probenecid achieved similar clinical outcomes [750]. Although limited by the observational design, there is so little modern data on treatment of neurosyphilis this poster is still of great interest.
- Widespread use of HCV therapy in Holland has reduced the incidence of acute HCV [137LB]. An excellent example of treatment as prevention.
- No dose adjustment should be required when glecaprevir and pibrentasvir are administered with either ECF-TAF or ABC/3TC/DTG [413]. Approval of this pan-genotypic HCV treatment is expected soon.
- American ginseng did not reduce HIV-related fatigue [669]. We can add this to the (long) list of studies that fail to show benefits from
homeopathicnon-FDA approved herbal remedies. Plus, I just like typing “American ginseng.”
If you’re interested in watching webcasts of interesting plenary or symposium talks, I can strongly recommend Demetre Daskalakis on ending the HIV epidemic in NYC (he has more energy than the rest of the 4199 CROI attendees combined), Charlie Flexner on long-acting ART (he dispelled several “myths”), and Carl June on how cellular treatments of cancer might apply to the HIV cure effort.
One caveat to this last talk is that Dr. June neglected to mention that there’s huge difference in acceptable risk between someone with refractory metastatic cancer versus stable HIV infection. So I’m mentioning it for him.
You’re welcome.
See you at next year’s CROI in Boston!
[youtube https://www.youtube.com/watch?v=FSvNhxKJJyU]
February 13th, 2017
How to Make Preventing Heart Disease in HIV Fun and Exciting: The REPRIEVE Trial
The people researching cardiovascular disease in HIV have quite the challenge.
Because when you think about it for a second, we HIV treaters are a pretty spoiled bunch when it comes to therapeutic success.
We saw the transformation of a terrifying, incurable, and rapidly progressive disease (AIDS) into something that can be managed for decades — usually with just a pill or two each day.
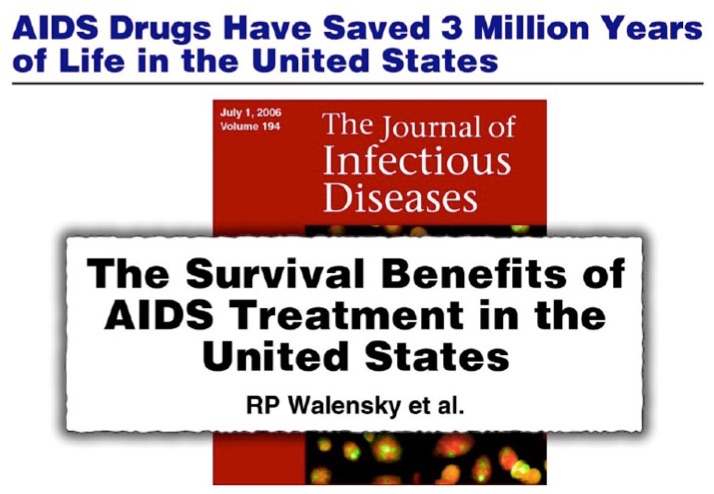
Or, if you prefer a quantitative description, here’s the slide Tony Fauci uses when he cites my friend Rochelle Walensky’s 2006 landmark paper in his talks:
Remember, these impressive numbers were estimated before we had the great advances in antiretroviral therapy in the late 2000s. The benefits are undoubtedly even greater over the last decade, since virtually everyone who takes HIV medications regularly now is virologically suppressed.
Pretty much any medical intervention for a non-HIV problem might seem a bit ho-hum compared to the miracle of antiretroviral therapy, meaning the people researching non-HIV related problems have their work cut out for them to get our attention. This is despite the fact that these non-HIV problems (especially the problems of aging) are more important than ever.
So when Steve Grinspoon contacted me recently about mentioning the REPRIEVE study on this site in honor of “Heart Month”, I readily agreed. Steve is leading this large NIH-funded trial, which asks this important question:
If people with HIV are intrinsically greater risk of heart disease, would they benefit from taking a statin drug even if we would not ordinarily prescribe it based on standard risk assessments?
REPRIEVE is actively enrolling at clinics and hospitals around the world, including at our site here in Boston.
As demonstrated in multiple studies (and reviewed here), people with HIV do appear to be at higher risk for heart disease even when their virus is well controlled with ART. “Lifestyle” issues (especially smoking), current and past immunosuppression, duration of uncontrolled viral replication, cardiotoxic drugs, and immune activation and inflammation all likely play a role. Related to the issue of inflammation, Steve’s research group just published a paper demonstrating that abnormal arterial inflammation — a risk factor for coronary disease — continues despite effective ART, at least in the short term.
So why not just recommend a statin for all people with HIV above a certain age? While it’s theoretically possible that statins will improve this abnormal inflammatory state, we don’t know that statins will provide a clinical benefit. And perhaps not all people with HIV are at higher CV risk — the most recent look at MI incidence in the Kaiser HIV cohort did not find an excess risk in a group of very healthy (high CD4, modern ART regimens, low rates of smoking) HIV patients compared to HIV negative controls.
Which brings us back to REPRIEVE — statins might be beneficial, they might not, and there’s enough equipoise that it’s appropriate to conduct a real randomized trial.
Eligible patients must have stable HIV, be older than 40, and not have a high risk for heart attacks or stroke (otherwise they should be on a statin). If you want to check, you can enter patient information into the American College of Cardiology/American Heart Association heart risk calculator. Those with a 10-year risk of heart disease or stroke < 15% may be eligible, depending on LDL cholesterol levels.
Participants are then randomized to pitavastatin (chosen because it doesn’t interact with any HIV drugs) or placebo. The primary endpoint is time to atherosclerosis-related clinical event.
I think it’s an excellent study, not just because I’ve known Steve for ages and he’s been a leading figure researching metabolic complications of HIV disease longer than just about anyone. A clinical trial that evaluates a critical non-HIV related complication makes abundant sense in a population where infectious complications are increasingly rare. The results will have great importance to patients, in particular the increasing proportion over the age of 50 (which now exceeds 50% in many urban areas).
Plus, if I mention REPRIEVE here, maybe I’ll get him to read this blog — which he obviously had never done before he called me. “I’ve been really busy,” he said.
Too busy to read Fun With Old Medical Images? To weigh in on whether ID doctors are the worst dressed specialists? To talk about doctors named Morgan? Or if we should wear white coats?
“Really busy”? — not sure I’m buying that excuse!
February 5th, 2017
Case Report of PrEP Failure: What Can We Learn From It?
The New England Journal of Medicine has published the first well-documented case of HIV pre-exposure prophylaxis (PrEP) failure despite good medication adherence.
We heard lots of this information at CROI last year, and again I’m impressed at the extraordinary degree of virologic investigation done on a case from clinical practice.
To refresh your memory, here are the critical details from the published case report and the supplementary appendix:
- A 43-year-old man began PrEP with TDF/FTC in April 2013, and had multiple negative 4th generation HIV screening tests over the next 21 months.
- Pharmacy refill records indicated excellent adherence. (Side note to young clinicians: Refill frequency is an amazingly powerful tool to monitor adherence.)
- Prior to diagnosis, he had multiple sexual exposures, including receptive anal intercourse without the use of condoms.
- A couple of weeks before his first positive HIV screening test (antigen positive, antibody negative — Day 0), he developed abdominal pain which waxed and waned over the next 3 weeks. A CT scan demonstrated thickening of the sigmoid colon, ascending colon and rectum. Endoscopy revealed erythematous patches of the sigmoid colon.
- Adherence was confirmed by analysis of a plasma sample obtained on Day 0 revealing tenofovir concentrations consistent with recently taking the drug.
- HIV RNA peaked at 28,000, and became undetectable with the addition of boosted-darunavir and raltegravir.
- His viral isolate had extensive multi-class resistance, including to FTC (M184V), TDF (multiple thymidine-associated mutations), NNRTIs (Y181C), and first-generation integrase inhibitors (92Q).
- He’s now virologically suppressed on DRV/c, RPV, and DTG.
The supplementary appendix has an excellent figure of the timeline, which I’ve pasted below:
So what can we learn from this single case?
- PrEP is very effective, but it’s not 100% protective. I don’t think clinicians are claiming 100% effectiveness, but PrEP-takers may be hearing this from various “experts”, or may be misunderstanding the data.
- Transmitted drug resistance will weaken PrEP. Although all of the mutations in the case are to drugs not in the TDF/FTC combination — except M184V — the multiple TAMs could have weakened TDF through cross resistance. Furthermore, FTC could have been transmitted, or alternatively selected by period of viral replication after viremia developed. The source patient’s virus was not available for sequencing, unfortunately.
- The symptoms of acute HIV infection are highly variable. The supplement to the case reports states, “The patient did not have classic symptoms of acute HIV seroconversion”, which is true — but he did have GI symptoms, which are quite common in acute HIV. We need to remember this variability when following patients on PrEP.
- The monitoring strategy recommended by the CDC in the guidelines should be followed. Although it might seem like overkill to monitor for HIV and other STIs every 3 months while receiving PrEP, remember that only those at highest risk for getting HIV should be receiving PrEP to begin with. Clinicians may choose to recommend more frequent monitoring if clinically warranted.
- Integrase resistance is rare in clinical practice, and transmitted integrase resistance is even less common. While some might interpret this case report to indicate a need for baseline integrase testing for newly diagnosed individuals, the detection of transmitted integrase resistance in most studies of newly diagnosed patients is less than 1%, and often 0%. Notably, the transmitted virus was still sensitive to dolutegravir (I’d interpret the genotype as fully susceptible).
Ok, that’s what I learned. Provides a cautionary note to those both prescribing and receiving PrEP, one further reinforced by this additional case report of PrEP failure presented at a recent conference.
As for tonight’s game, below is what I’m going to watch, and here’s why!
[youtube https://www.youtube.com/watch?v=15SdPnof0FY&w=560&h=315]
January 29th, 2017
In A Weekend of Paranoia and Anger and Fear, Some Release From the Other Side of the Globe
 This was not a happy or comfortable weekend for ID doctors, given our predilection for inclusiveness, non-judgmental care, global health, and that “safety net” idea that seems to us such an intrinsic part of being a good doctor.
This was not a happy or comfortable weekend for ID doctors, given our predilection for inclusiveness, non-judgmental care, global health, and that “safety net” idea that seems to us such an intrinsic part of being a good doctor.
Exclusion of foreigners? Why, we ask, would you do that? People from other countries are our friends, our colleagues, and our patients. Many of our favorite patients, I might add, since they might bring with them exotic, challenging, and treatable problems that are right up our alley.
Furthermore, to overstate the obvious, most of us living here in the USA are not that far removed from immigration ourselves.
Fidencio Saldana — he’s a cardiologist, the Dean of Students at Harvard Medical School, and the child of Mexican immigrants — gave medical Grand Rounds at our hospital recently.
He recounted what it was like being a medical student here, and how out of place he sometimes felt. He then movingly described how was made to feel welcome by hearing from one of our senior doctors, Marshall Wolf:
Hey relax. My parents were immigrants too. You belong here.
That was two weeks ago, a brief aside made at a lecture, yet I have thought of it frequently since, especially this weekend.
And this morning, glum and discouraged by recent events, I needed some distraction.
So I turned on the television at 6AM and watched two of the most extraordinary athletes in the world, Roger Federer of Switzerland and Rafael Nadal of Spain, play the fifth and deciding set of tennis at the Australian Open in Melbourne, Australia.
The crowd was cheering, and hanging on every point, and no doubt millions of others all over the world were doing what I was doing — watching and marveling and feeling a sense of global togetherness for this extraordinary event.
And here’s the best part. After Federer won the match, a grueling 5-set affair that lasted over 3 hours, he graciously said:
Tennis is a tough sport, there are no draws. But if there was I’d be happy to share it with Rafa tonight.
Share. No gloating. No petty rivalries. No cheating. No distortion of facts. These are the best players in the world, competing at the highest level for hours, and they can still get along like friends even in the most intense setting imaginable.
You got that?
https://youtu.be/upLv0xBTai8?t=125