An ongoing dialogue on HIV/AIDS, infectious diseases,
December 2nd, 2018
As A Strategy for HIV Prevention, Disabling the CCR5 Gene in Embryos Implanted in HIV-Negative Mothers Makes Zero Sense
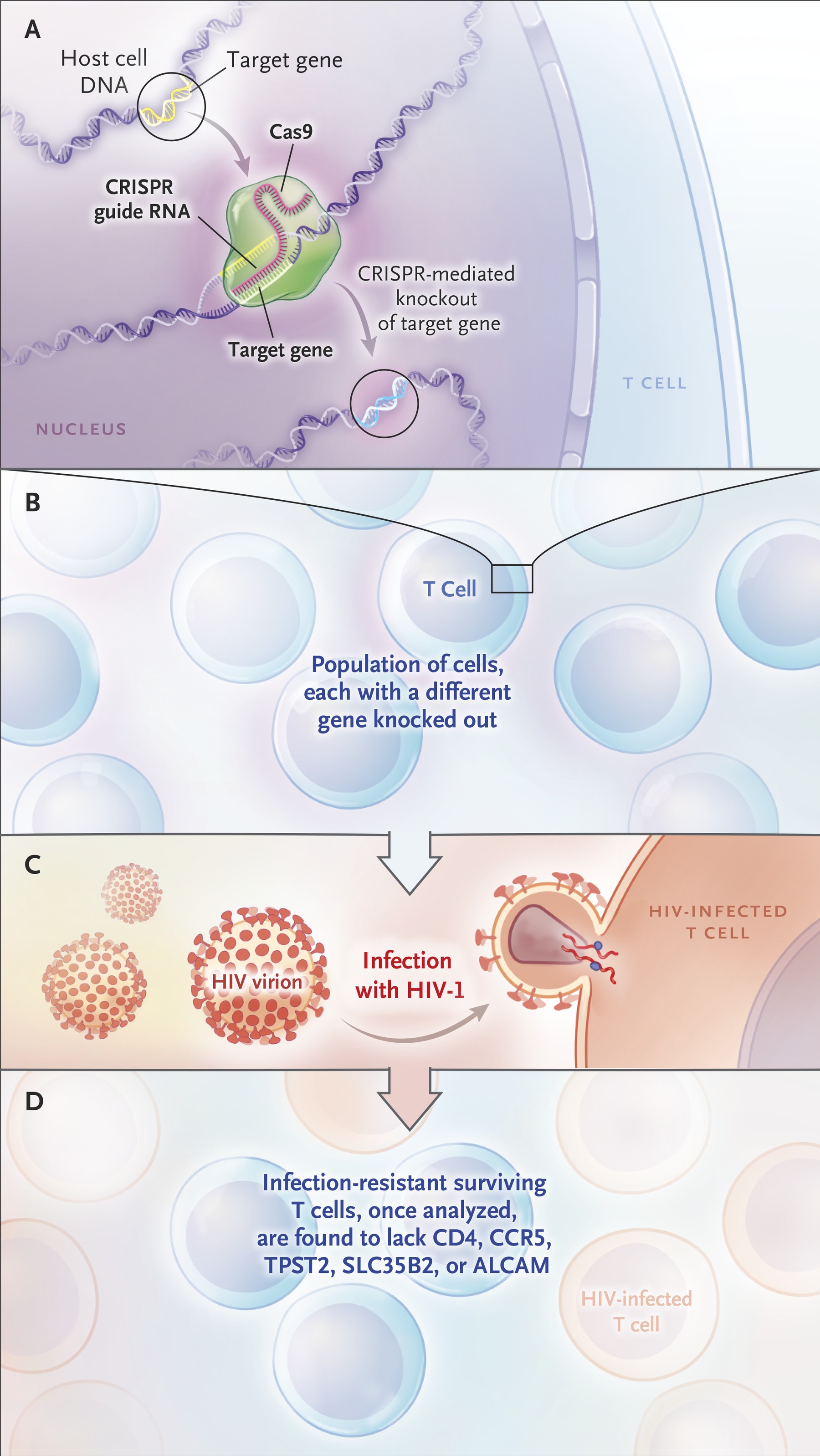
The CRISPR Way to Identify Proteins Essential to HIV-1 Infection. From N Engl J Med 2017; 376:1290-1291.
One of the great joys of being an ID/HIV specialist is looking back at how far we’ve come in HIV prevention and treatment since the beginning of the epidemic.
Here are a bunch of things we know about HIV prevention, listed roughly in order of when we learned them — and forgive me if this is an oversimplification for this sophisticated readership:
- Condoms work very well in preventing HIV transmission.
- Taking a brief course of HIV therapy soon after exposure reduces the risk of HIV acquisition.
- Babies born to HIV-positive mothers do not contract HIV if the moms take suppressive HIV therapy.
- Male circumcision reduces the risk of these men acquiring HIV.
- People do not contract HIV from their HIV-positive partners if the person with HIV takes suppressive HIV therapy.
- People taking pre-exposure prophylaxis markedly reduce their risk for HIV acquisition.
You’ll note that nowhere on this list is anything about preventing HIV in babies born to women who don’t have the virus to begin with — because the babies are not at risk, even if the mother’s male sexual partner has HIV.
Just typing that sentence felt a little strange, it’s so obvious. However, it seems that He Jiankui may not understand this basic fact.
He’s the scientist who startled the world by releasing news that he and his research team had used CRISPR–Cas9 genome-editing to alter the embryos of two babies. The editing disabled the CCR5 gene, which means the babies lack a key co-receptor that HIV uses to infect cells.
However, as noted at 1:53 in the above-linked video, it’s the father who has HIV. Indeed, reports indicate that eight serodiscordant couples have participated in his studies — all with the fathers having HIV.
I’ll let others with far greater knowledge of genetics, embryology, and medical ethics comment on just how reckless this experiment was — here’s a good take (there have been many).
But from an HIV prevention perspective, it’s easy to judge — it makes zero sense to do this since the babies aren’t at risk of getting HIV to begin with. For them and their families, the genome-editing was all risk and no reward.
Let’s hope the mothers understood this before they agreed to participate in this disturbing experiment.
November 25th, 2018
Does Experiencing Childhood Illness Make Someone Stronger? How One Person Turned Adversity into Remarkable Success
Many people growing up with chronic illness become resilient.
Whether it’s Crohn’s Disease, or cystic fibrosis, or diabetes, or the sequelae of an accident, or whatever condition they have, they impressively live their life just like the rest of us — occasionally regressing or slowing down only during a flare of the illness.
But then there’s an extreme version of this resilience — people born with or acquiring severe illness as a child, and somehow not just surviving, but thriving.
Their medical problems are just a small bump in the road as they go from one success to another, each achievement more remarkable given what they’ve had to go through to make this success happen.
The easy interpretation is that all the hardships they’ve endured make them stronger — but it must go beyond that, since most of us mere mortals would respond in no such way.
Dr. Eric Winer, who runs the breast cancer program at Dana-Farber Cancer Institute, is an example of this remarkable group. He kindly agreed to tell his story for a podcast on Open Forum Infectious Disease.
(It’s also available on iTunes, and Overcast; we’re working on Stitcher.)
He talks about growing up with hemophilia, and HIV, and hepatitis C, and how this influenced his career and family life. (Quick answer — both hardly at all, and more than most could possibly understand. That’s a theme here.)
The medical and personal details are fascinating, and not just to ID and hematology-oncology doctors.
Has he been extraordinarily lucky, or terribly unlucky?
The answer, again, is both — listen and find out.
November 18th, 2018
HIV and HCV Treatment, Shorter Antibiotic Courses, Malaria-Sniffing Dogs, and Other ID and HIV Reasons to Be Grateful, 2018 Edition
As noted here before, I’m a big fan of Thanksgiving, a great excuse to get together with family and friends, and to eat a gargantuan amount of food.*
(*On this last point, non-U.S. citizens will wonder how this differs from any other time we “Americans” get together. Indeed, we are the Land of Giant Portions. Ever eat at a Cheesecake Factory? Yeesh.)
But the primary purpose of Thanksgiving is expressing gratitude, a very healthy impulse that makes everyone happier. And since this is an ID blog, here are bunch of things ID and HIV specialists can be thankful for over the past year:
- HIV treatment continues to improve. In the past year, we’ve seen approvals of bictegravir/FTC/TAF, darunavir/c/FTC/TAF, doravirine and doravirine/3TC/TDF, and ibalizumab. If that’s not enough, generic 3TC/TDF and EFV/3TC/TDF also gained FDA approval. Treatment now is so good with bictegravir and dolutegravir-based regimens that essentially 100% of patients taking these simple, well-tolerated regimens achieve viral suppression, and the IAS-USA Guidelines responded by making them the preferred treatments. Starting HIV treatment on the same day of diagnosis has moved from an interesting idea to a practical reality (especially with bictegravir/FTC/TAF and darunavir/c/FTC/TAF). Finally, the remarkably good results of the two-drug dolutegravir plus 3TC regimen in the GEMINI studies suggest that therapy can be even safer — and cheaper — than it is now.
- When it comes to the duration of antibiotic therapy, less is almost always better than more. A barrage of studies have shown that almost regardless of the condition, a shorter course of antibiotic treatment is the right choice. Shorter is better than longer both in the hospital and in the outpatient office. The take-home message from these data should be that clinicians can use their clinical judgment to decide how long to treat someone, not relying on some arbitrarily chosen treatment course — and yes, I mean even a treatment course defined by an ID doctor.
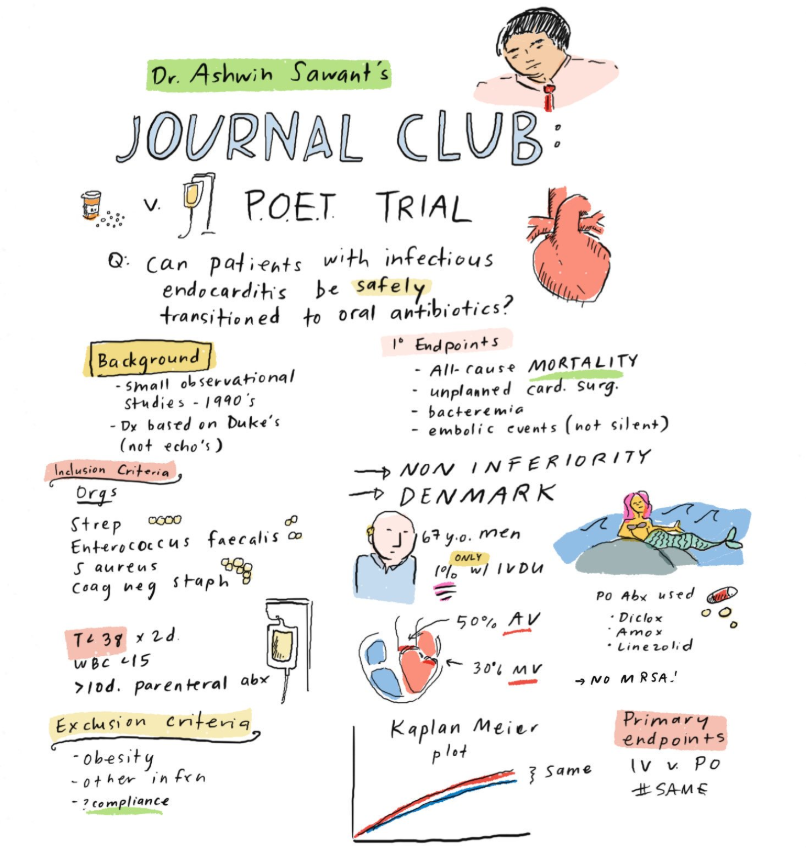
- It is becoming increasingly clear that oral antibiotics can substitute for intravenous in almost every situation. In the much-discussed POET study, stable patients with endocarditis who completed treatment with oral therapy did just as well as those who completed treatment with IVs. (And here’s a big thank you to Dr. Grace Farris for allowing us to use her wonderful journal club cartoon.) In another study, linezolid — price dropping rapidly — was a fine option for completing treatment in uncomplicated Staph aureus bacteremia. OVIVA study, where are you?
- Hepatitis C treatment has become staggeringly simple. I’m going to estimate that 99.156% (approximately) of treatment-naive patients could be successfully treated with either 1) sofosbuvir/velpatasvir, one pill daily for 12 weeks or, 2) glecaprevir/pibrentasvir, three pills daily for 8 weeks (sometimes 12). Go ahead and abbreviate SOF/VEL and GLE/PIB, if you find saying them a mouthful. Both are pan-genotypic, safe, well tolerated, and incredibly effective, and the price has dropped dramatically since the crazy days of 2014. In other words, these are the “must know” HCV treatments; the rest are optional. Here are a couple of slides I’ve made to describe a few of the medical issues in the choice between them — it’s a very short lecture — since most of the time, either one will do.
- Undetectable = Untransmittable, even in the highest-risk patients. The first publication of the PARTNER study of “condomless sex” among HIV serodiscordant couples didn’t have enough MSM couples to make a confident statement about the risk in this population. No longer — in a follow-up presentation this summer in Amsterdam, 783 MSM couples contributed data including 1596 couple-years of follow-up, and 76,991 (impressive precision!) condomless sexual encounters — and there were still zero transmissions. Giving this U=U message to our patients never gets old.
- Treatment of African trypanosomiasis will very soon be safer, easier, and more effective. Current treatment for this life-threatening parasitic infection — better known as “African sleeping sickness” — involves a complicated infusions with the drug eflornithine (administered in a hospital) along with nifurtimox. By contrast, fexinidazole (just approved) is given as one pill daily for 10 days and is both more effective and less toxic. Thanks to several European countries, the Bill and Melinda Gates Foundation, Doctors Without Borders, and other donors for funding the study that led to its approval, which was coordinated by the Drugs for Neglected Diseases Initiative.
- Preventive therapy for latent TB is getting shorter. In a large randomized study, a 4-month rifampin regimen was just as effective as 9 months of INH, and was both less toxic and more likely to be completed. In people with HIV, 1 month of daily rifapentine/INH prevented TB as well as 9 months of daily INH. The latter study hasn’t yet been published — and included some “high risk” patients who lacked positive skin testing or IGRA studies — but one is hopeful that the favorable results would translate to people without HIV as well.
- There continue to be ID-related studies that test the diagnostic skills of dogs. I guess they can’t reliably sniff out C. diff after all, but they did pretty well identifying malaria from the socks of children. (Yes, that’s what they were asked to do. Dogs will sniff anything.) I don’t actually think any of these dog diagnostic strategies will ever become standard-of-care (alas), but the videos and pictures released with each study sure are cute.
What are you grateful for this Thanksgiving?
November 12th, 2018
Sharing Radiology Images Across EMRs Is Frustratingly Terrible — and It Doesn’t Have to Be This Way
In the United States, any person who has tried getting their own (or their patient’s) radiology images from another hospital or practice will find this brief anecdote painful:
https://twitter.com/sarahkliff/status/1059518100821983233
Here are several obvious reasons why the CD-ROM — briefly the darling of large-data transfer — is a truly terrible way to share radiology images in 2018:
- They require physical transfer. Remember the term “snail mail”? Do people still say that?
- They are slow. When you bring a CD-ROM down to your friendly radiologist to review the scans, also bring a good book — you will be waiting awhile for the images to load. Zzzzz …
- There’s no universal software to read them. Watching even the most tech-savvy radiologist trying to extract images from these disks is proof enough that this is a horribly outdated technology.
- The blank disks are disappearing. When was the last time you purchased a “spool” of these things? Back when Napster was a thing?
- The drives are disappearing from computers. They’ve been gone from most laptops for years. Desktop computers, especially the mass-market, small-form ones used in hospitals, often lack them as well.
- Hospitals spend significant time and money transferring images from CD-ROMs into their EMRs. It works like this: you walk the disk down to wherever the uploading machine is located. You fill out some forms. You hand the disk over. It goes into queue with other disks. Later — hard to predict exactly when, could be later that day, or tomorrow, or next week, but never during your patient’s office visit — you can view the images in your patient’s medical record. However, sometimes (and this has happened more times than I can count), the disk is unreadable, or doesn’t even have images at all — only the radiology report, and not the actual images. Gak.
- No one knows whether CD-ROM disks should be spelled “disk” or “disc.” Discuss among yourselves — I’m going with “disk.”
Non-clinicians might wonder, what’s the big deal if you can get the radiology report? Isn’t that what “Care Everywhere©™” does?
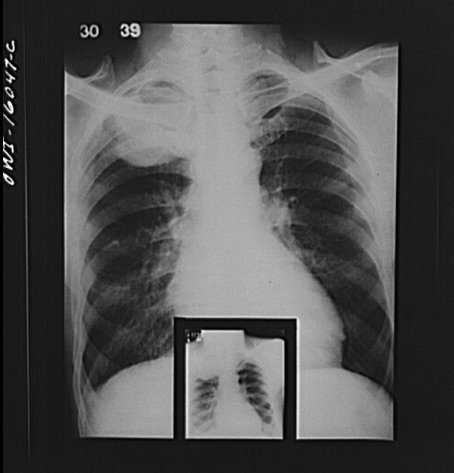
Sure, having the report is better than nothing. But in complex cases, and when making difficult diagnostic or therapeutic decisions, it is always better to review the actual images — preferably with a radiologist specially trained in the involved anatomic region.*
(*ID doctors do a lot of this kind of thing. This probably explains why getting ID consults on complicated cases is associated with better outcomes. And it definitely contributes to why we’re typically bottom-feeders in an RVU, procedure-based world. How do you bill for time spent chasing down images and reviewing them with radiology?)
Of course it doesn’t have to be this CD-ROM way. If there ever were an irrefutable argument for the benefits of digitizing medical information, the switch from hard copy “films” to digital images would have to be right near the top. Think of how far we’ve come from the days of searching for x-ray films that, not surprisingly, would disappear in direct proportion to how interesting the case, or how sick the patient.
That’s why the current CD-ROM strategy is so frustrating. Never mind that a faster and more reliable technology (the USB flash drive) has been available for years. Though cheap and ubiquitous, and better than CD-ROMs, USB flash drives would also require physical transfer.
The solution, of course, is to put the images on the web — which is apparently what many non-U.S. hospitals have been doing for years:
We were consulted on a patient transferred from a hospital in Thailand. We needed to review his MRIs. The doctors there kindly emailed us a link and, bingo, we could see them all (along with his whole medical record).
This was at least 5 years ago. https://t.co/I3ARLxEtO9
— Paul Sax (@PaulSaxMD) November 9, 2018
So here’s what I recommend we do, starting now:
- Patients scheduled for imaging fill out a form while they are waiting asking if they want their images available for review by the clinicians caring for them.
- If the answer is Yes — and I imagine it would be for all but the most paranoid individuals — then after the scan is done, they are provided a secure link. It can be communicated by email, text, a post-procedure print out, or all of the above.
- In order to make the link work, they need to click on it and verify that it can be accessed by others.
- They then get to choose the variety of ways others can access it — secure password? Two-step verification?
- The patients can then share the link with whomever they like.
There, wasn’t that easy?
November 4th, 2018
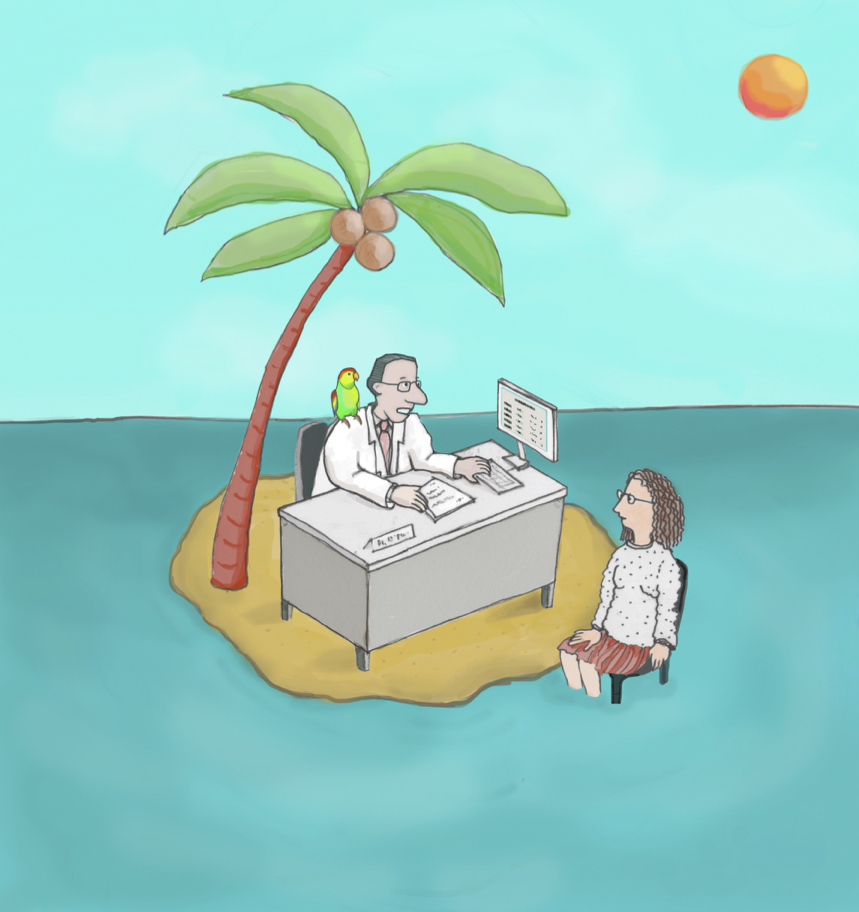
Your Next ID Cartoon Caption Contest — Yearning for Your Submission
The nice people who write our hospital’s newsletter interviewed me recently about this blog, and we covered a whole lot of territory.
How it got started … inspirations … popular posts … fax machines … why an ID doctor from Mexico asked me about my dog Louie.
There was, however, a grave omission — nowhere in this otherwise comprehensive review of highlights did I mention our ID Cartoon Caption Contests.
Appalling, I know — especially since these are easily the most commented-upon posts in the 10-plus year history of this thing. If you add up posted comments here and on Twitter, we must have something like a gazillion so far.
A collaboration with my sister Anne, these contests are the product of a now- patented creative process, which goes something like this (all by email/texting):
Me: Hey, Anne. How about we do another cartoon?
Anne: Sure! Any ideas?
Me: Let’s do one that shows a doctor examining a patient with a highly obvious abnormality — something so absurd you can’t miss it.
Anne: How’s this?
Me: Yikes. Too scary.
Anne: How about this? Or this?
Me: I’m partial to dogs [OBVIOUSLY] — but dolphin man might be better.
Anne: Really? How bout getting rid of the animals altogether? Take a look at this.
Me: Perfect! Umbrella head!
Anne: Wonder how your brilliant readers will come up with an ID-themed caption.
Me: They’ll think of something.
Here, then, without further ado, is the latest cartoon, desperate for your clever caption. You’ll see it’s a common cartoon theme, but with a medical twist. And just in time for the cold weather.
As always, write your proposed caption in the comments section, or post it on my Twitter feed. Have fun, and be safe out there!
And given the obvious inspiration for this whole exercise, here’s a highly relevant video.
October 28th, 2018
New Flu Drug Offers Convenience, Fast Activity, and a Novel Mechanism — at a Price
Last week, the FDA approved a new drug for treatment of influenza, baloxavir marboxil (Xofluza).
The drug is indicated for treatment of symptomatic influenza in patients 12 years of age or older. As with existing treatments, it should be started within 48 hours of symptom onset.
In a comparative clinical trial in otherwise healthy outpatients, baloxavir and oseltamivir (commonly known as Tamiflu) comparably reduced the duration of flu symptoms — both on average by about 36 hours. Each treatment was more effective if started within 24 hours of symptom onset.
Baloxavir differs from oseltamivir in several ways, some of them potentially important:
- Treatment is a single dose. Patients receive 40 mg if their weight is between 40 and 80 kg, and 80 mg (two pills) if 80 kg or more. As every primary care clinician knows, oseltamivir is 75 mg twice daily for 5 days.
- Side effects ascribed to the treatment occurred less frequently in those randomized to baloxavir vs oseltamivir — specifically, 3.9% and 8.4% for baloxavir and oseltamivir, respectively (p=0.009). The side effects table from the study indicate that GI-related side effects (especially nausea) were numerically more common with oseltamivir. In clinical practice, this is the most commonly encountered problem with the drug, which can be diminished (but not eliminated) when oseltamivir is taken with food. The incidence of severe adverse events did not differ between arms.
- Baloxavir lowered influenza viral loads in respiratory secretions faster than oseltamivir. The clinical significance of this faster antiviral action is unclear. Might this make patients less contagious more quickly? Or could this translate to a clinical benefit in very immunocompromised hosts, or in the most severe cases? A study in “high risk” adults demonstrated a faster recovery time compared to oseltamivir if the infecting virus was influenza B; outcomes in influenza A were similar. A different clinical trial of the drug in hospitalized patients is about to start.
- The mechanism of action is different. Unlike the neuraminidase inhibitors (oseltamivir, et al), baloxavir blocks influenza replication through inhibition of viral endonuclease (see the fine video below). It’s the first flu drug with this mechanism of action. The good news is that baloxavir should retain activity against neuraminidase-resistant strains, which periodically emerge and could be a substantial global threat.
- Baloxavir treatment selects for resistance. This excellent accompanying editorial to the above-cited phase 3 trial describes the resistance concerns in more detail. Will this resistance limit the usefulness of the drug? Or will the impaired replication capacity of resistance variants make them less transmissible?
- Oseltamivir is generic, and cheap. A 5-day course costs around $50. Payers have undoubtedly negotiated a much lower price. (That stuff is kept secret from us patients and clinicians, remember.) Baloxavir will cost $150, regardless of the dose, with coupons available to lower the price.
My colleague Ken Freedberg, whose research focus is cost-effectiveness, often jokes that he’s frequently the last to speak at a conference since the topic of cost is so often considered secondary to the “scientific” parts of the program.
Please note, Ken, that I meant no offense by putting cost last in the bulleted list above.
Especially since with baloxavir, it’s probably this very point — cost — that will limit use of the drug, at least initially. Insurance plans are not eager (an understatement) to add new treatments to their formularies that cost more than existing options unless they are clearly more effective, or safer, or preferably both.
With baloxavir, while it seems to have some advantages over osteltamivir in these metrics, we’re not quite there yet.
In the meantime, we can make fun of the brand name —Xofluza! — which, if you say it loudly and quickly, kind of sounds like someone sneezing.
October 21st, 2018
A Day in the Life of the Academic Assistant Professor of Medicine Who Wakes Up at 5:30 a.m. to Get Her Kids to School, Takes the Bus to Work, Answers Emails, Completes Online Required Modules, and Fills Out Disability Forms for Her Patients
 (Inspired by a recent peculiar article about a Bay Area tech superstar.)
(Inspired by a recent peculiar article about a Bay Area tech superstar.)
Dr. Camilla Gormley is always on the move.
From the moment her alarm wakes her at 5:30 a.m. to prepare breakfast and school lunches for her three kids, to the time 16-plus hours later when she can finally rest her head on her pillow, Dr. Gormley is constantly in motion.
On a typical day, after bundling up her kids to be dropped off at school by her husband Jack — if he’s not traveling for work, in which case she (somehow) has to do it — she can be seen running after the bus which, on a good day, will have an available seat and not smell like last night’s frat party.
She recently shared with us the rhythms and rewards of being a Junior Faculty member at a prestigious academic medical center.
5:30 a.m.: She wakes up and immediately panics that she has forgotten an important deadline.
“I find that this early time of day is perfect for free-ranging anxiety and panic,” says Gormley. “It’s a tremendous relief when I realize that I don’t in fact have a school paper due, or an exam today — though one of my three kids might.”
The first task for the day is feeding her family, which consists of a streamlined operation that efficiently generates five breakfasts, two coffees, and four bagged lunches. Husband Jack takes orders and has learned the hard way not to talk back.
“He once expressed doubts about my selection of bread for the kids’ sandwiches,” she recalls. “He found himself alone on food duty for the next month, which was a disaster for all. But that will teach him.”
6:30 a.m.: She wakes her kids and helps them get dressed and ready for the day.
“My son Zack will wear anything, he’s easy,” she says proudly. “Same with Jenna, the youngest.”
But, she notes, middle child Phoebe can be a challenge. “Not a week passes by without her wanting some crazy new style to wear, nothing’s ever right,” she says. “We’re at the point where if she told me she wanted to wear her bathing suit to school in the middle of winter, I’d just give in. Sick of it, really.”
7:00 a.m.: Dr. Gormley gets in some intense cardio by running for the bus.
“If I miss the 7:05 — which stops right at our corner — I’ll never make it to work in time for my 8 a.m. patient.”
She spends the time on the bus catching up on emails that were sent overnight.
She shares one request: “Can we outlaw the ‘high importance’ exclamation mark in emails, please?” she asks. “And people who use that for emails sent overnight should be imprisoned.”
8:25: Her 8 o’clock patient shows up — as does her 8:30.
“Of course, I saw her anyway,” she said, of her late-arriving patient. “And she had a disability form for me to fill out — putting my MD degree to work!”
It’s fall, so it’s flu shots for everyone — except the patient who refused, saying it always gave him the flu.
“Oh, give me a break,” she editorializes.
12:45 p.m.: After seeing her outpatients, she paused for a quick lunch at her desk — but didn’t stop working.
“You know those corporate lunches in Mad Men, with martinis and glamorous companions in Manhattan restaurants?” she asks.
“My companion is my office computer with a required online video about fire safety.”
1 p.m.: Time to check the electronic “inbox” on her electronic medical record!
“Usually the in box has another couple of hours of work in there, at least,” she says.
“I feel like the EMR inbox should have a sign that says, Open at Your Own Risk, or Ye Who Enter Here, Abandon All Hope.”
3 p.m.: Dr. Gormley attends a meeting about the medical school course she’s teaching in the fall. The meeting is in a conference room half a mile away, so she debates whether to walk or to Uber — she’s so undecided that she arrives 15 minutes late, as does almost everyone else.
“Teaching in this course is awesome,” she says. “But why are all the meetings held so far from the hospital?”
Also not so great — deadlines for submission of PowerPoint slides and the dreaded requirement for “learning objectives.”
“Has there ever been a study showing that submitting ‘learning objectives’ actually led to more learning?” she wonders. “What if I just ignore the request?” she says, a sly smile creeping over her face.
 4 p.m.: She’s back in her office, poring over emails that have accumulated since she last had a moment to check.
4 p.m.: She’s back in her office, poring over emails that have accumulated since she last had a moment to check.
“Let’s see, there are 58 messages here,” she notes. “I think I’ll do the ones marked as ‘high importance’ last, just for revenge.”
Included in the email barrage are several invitations to bogus medical conferences (“Greetings of the day!” they begin), as well as sales pitches for laboratory reagents, monoclonal antibodies, and small rodents.
“Why do I get emails asking if I want reagents for doing my own CRISPR experiments or for a supply of knockout mice?” she asks. “That reminds me, I need to call the exterminator for the ant problem we have at home.”
She also receives a dire warning — yes, ‘high importance’ exclamation point — that the annual Conflict of Interest form (required of all faculty) is overdue.
5:45 p.m.: As a big believer in never wasting a single moment, Dr. Gormley starts the online Conflict of Interest form on her phone while waiting outside for the bus.
“Last week I started it three times and it kept crashing,” she says.
“Apparently, if you do it at your computer, you need to be running Internet Explorer. Internet Explorer! I mean, could they please start using a browser that is updated for this century? Is that so much to ask?”
Completing the form takes her approximately 30 minutes, which completely ends all hope of listening to that great podcast everyone has been talking about, whatever it’s called.
6:30 p.m.: She arrives home to find that her three kids are fighting, their cat Quentin has vomited on the rug, and that her husband has forgotten it’s his night to plan dinner.
“I give him one thing to do,” she sighs. “Am I the only one who thinks that families need to eat to survive? You didn’t need to go to medical school to learn that.”
She picks up her phone and dials the local Mexican restaurant, which delivers.
 While waiting, she and her husband reflect upon their key wins and challenges and prepare for the adventures of the next day.
While waiting, she and her husband reflect upon their key wins and challenges and prepare for the adventures of the next day.
“Just kidding. We’re just trying to survive here.”
7:00 p.m.: Take-out burritos for everyone.
“It’s only the third time this week,” she says, defensively.
(It’s Thursday.)
7:30–9:30 p.m.: Gormley and husband Jack help all three of their children with homework, then Gormley starts laying out their kids’ clothes for the next day.
“If Phoebe says one thing about the clothes I put out for her, there might be Armageddon,” she says.
9:30 p.m.: As she’s washing up for bed, she remembers that she forgot to call the exterminator, and adds it to tomorrow’s to-do list.
“Ants aren’t so bad,” she rationalizes.
With thanks to Carolyn Frank Sax, MD, who really did have a cat named Quentin.
October 15th, 2018
Outpatient Antibiotic Prescribing Boosts Patient Satisfaction Scores, Rewarding Bad Medical Practice
A recent study confirms what every busy clinician already knows.
Many patients seeking care for respiratory infections expect to receive an antibiotic. When they get one, they’re happier than if they don’t.
Among 8437 patients seeking care for a respiratory tract infection in a direct-to-consumer telemedicine service, 66% received an antibiotic. The rate of prescriptions prescribed by physicians ranged from 19% to 90%, showing that these were not exactly evidence-based decisions. Satisfaction ratings strongly correlated with adjusted antibiotic prescribing rates (Pearson correlation, 0.41; P < .001).
It’s even worse if you look at the figure — none of the MDs in the lowest half of prescribers exceeded the 75th percentile for patient satisfaction.
More details:
Few physicians achieved even the 50th percentile of satisfaction while maintaining low rates of antibiotic prescribing. To reach the top quartile, a physician had to prescribe antibiotics at least half the time; almost all physicians above the 90th percentile had a rate of antibiotic prescribing greater than 75%.
This isn’t the first time we’ve seen data like these. In this earlier study comparing immediate versus deferred versus no antibiotic (along with a patient education intervention), patients with the immediate antibiotic prescription were significantly more likely to be very satisfied with their care — even though clinical outcomes were, not surprisingly, the same.
Jeffrey Linder — who studies appropriate outpatient antibiotic prescribing — would no doubt remind me that not every study demonstrates this effect of antibiotic prescribing and increased patient satisfaction. While this is true, his group just presented data that many antibiotic prescriptions aren’t written in the context of a patient visit, and often for diagnoses not even related to infection.
I asked a physician who works with one of the companies charged with assessing patient satisfaction what he thought about these recent survey data. He made the excellent point that it was physician communication — time spent talking with patients — that most powerfully drove patient satisfaction.
While no doubt this is true, let’s imagine you control for this talk-time. And that clinicians in urgent care centers and telemedicine systems are graded on volume (productivity) and patient satisfaction scores. Some would undoubtedly consider the counseling and education piece too time consuming. Remember, it was urgent care centers that had the highest rate of inappropriate antibiotic prescribing in a study published earlier this year.
What’s the fastest way for urgent care and telemedicine clinicians to achieve higher scores in patient satisfaction and “see” more patients/hour? In our action-driven society, it’s doing “something” (antibiotics, pain relievers, sleep aids, MRIs, you name it) rather than “nothing” (observation). It takes energy and time to explain why the latter is often the right choice.
If you doubt my ID-doctor biased perspective, here’s another interesting view on this study from F. Perry Wilson on Medscape:
All of this leads to an all-too-familiar patient encounter, typified by this note from a local walk-in center:
Finally, could anything comment more appropriately on this relationship between antibiotics and patient satisfaction than this New Yorker cartoon?
So what are we going to do about it?
October 8th, 2018
“Mini”-Really Rapid Review — IDWeek 2018, San Francisco
Once upon a time, the annual meeting of the Infectious Diseases Society of America (IDSA) wasn’t much of a research conference.
It consisted mostly of review sessions on topics deemed worthy of an update or a refresher, led by noted experts in the field. They would cite the latest literature on endocarditis, or mycoplasma, or prosthetic joint infections, or malaria, or transplant infections, or HIV complications, or sternotomy infections following cardiac surgery.
(I kid you not about that last one … to each their own, I guess!)
Some of this was good stuff — cutting edge and exciting — but some was frankly kind of tedious. You went because it was “good for you”, kind of like eating kale if you don’t like kale.
And pretty much all of it was led by white men of a certain age — which is my age now, give or take a decade, good grief.
My, how times have changed, and emphatically for the better.
The IDSA meeting, re-branded “IDWeek” a few years ago, now mixes in original research with not only these terrific review sessions (you can still skip the one on sternotomy infections), but also challenging case presentations, entertaining debates, policy updates, and awards.
Importantly, presenters, participants, and awardees all increasingly reflect the diversity of our field, making the meeting feel much more inviting and collegial — a very welcome change.
There’s so much going on no one can cover it all, certainly not me. So here’s a sampling of some (emphasis on some) of the interesting research presentations from last week, a “Mini” Really Rapid Review™ of the conference. Use the comments section to chime in with your favorites.
- 20% of outpatient antibiotic courses are prescribed without a visit, and 46% without even an infection-related diagnosis. These data (from former colleague Jeffrey Linder) are discouraging, but not surprising — it’s much easier for clinicians to respond to patient complaints with action (here a prescription for antibiotics) than a recommendation for watchful waiting. Antibiotic prescribing is also associated with higher patient satisfaction. We need to keep getting the word out that these are not benign drugs!
- Daptomycin plus IV fosfomycin is better than daptomycin alone for MRSA bacteremia. There is in vitro synergy between daptomycin and fosfomycin against MRSA (who knew?), which motivated this randomized controlled trial. The results are tantalizing, with most endpoints significantly favoring the combination. Credit to the investigators for studying something so common and so serious, but for which we have so little good comparative data. (IV fosfomycin is not available yet in the USA.)
- Preemptive therapy for CMV in high-risk donor seropositive/recipient seronegative liver transplant recipients reduced the incidence of CMV disease more than prophylactic therapy. Participants were followed with weekly CMV viral loads, so this strategy requires quite a bit of monitoring and care coordination. Still, the study is very likely to change clinical practice in some transplant centers. (FYI, every time I write “preemptive” I need to confirm the spelling.)
- Fetal exposure to efavirenz during pregnancy increased the risk of “neurologic conditions” among HIV-negative children. This observational study of 3,747 children also showed a trend toward more such conditions (microcephaly, febrile seizures, seizure disorders, ophthalmologic disorders, others) with dolutegravir. Since boosted PIs may increase the risk of premature birth (and have the worst GI tolerability), the unfortunate fact remains that we still don’t know the safest HIV treatment for pregnant women.
- Therapy dogs benefit pediatric oncology patients, but may transmit MRSA. Fortunately, a decontamination procedure involving chlorhexidine-based shampoo before the visit, and chlorhexidine wipes on the fur during the visit, reduced this risk. I say benefit-risk ratio favors keeping the dogs involved, but acknowledge I’m highly biased! (Go ahead — click on the picture.)
- Dogs (actually puppies) were also responsible for a large outbreak of highly drug-resistant campylobacter. Extensive use of “prophylactic” antibiotics by breeders and a pet store chain provided the selective pressure. So don’t blame the pups.
- Women are underrepresented in publications and achieving the rank of full professor in academic ID. Imbalance is greater in ID than in other specialties, including cardiology, endocrinology, and hematology — can we speculate why that would be? (Study led by one of our ID fellows, he wrote, beaming with pride.)
- For healthcare workers caring for patients with viral respiratory infections, there was no difference in their incidence of lab-confirmed influenza or viral respiratory infections whether they used N-95 or standard medical masks. Hugely important negative study — N95 masks are expensive, uncomfortable, require fit testing, and are just generally a huge pain.
- A longer duration of surgical antibiotic prophylaxis did not reduce surgical site infections but increased adverse events. Tell your surgical colleagues this the next time they want to continue antibiotics postoperatively for a few days “just in case.”
- Clinical outcomes of ID consultations done by telemedicine were comparable to in-person consults. The field of telemedicine is exploding, driven by ever-improving technology, shared electronic medical records, what’s best for the patient and — importantly — mutually agreeable financial benefits for both consultant and consulting clinicians. It really can’t get off the ground in a fee-for-service, RVU-based system, where in-person visits still are an ID doctor’s only billable service. Outstanding session here given by representatives from successful programs.
- All-cause mortality is significantly increased in adults with pulmonary non-tuberculous mycobacterial infections. This large (43,394!) Medicare database study confirmed what we ID doctors and pulmonary specialists already know — that these NTMs are serious infections that deserve way more attention. Better treatments can’t come soon enough!
- A small randomized study found similar outcomes — and shorter lengths of stay — when patients with substance use disorder received OPAT. This contentious topic was debated further here; shout out to my colleagues for this excellent recent comprehensive review.
There was plenty more, of course — read the many responses to this query!
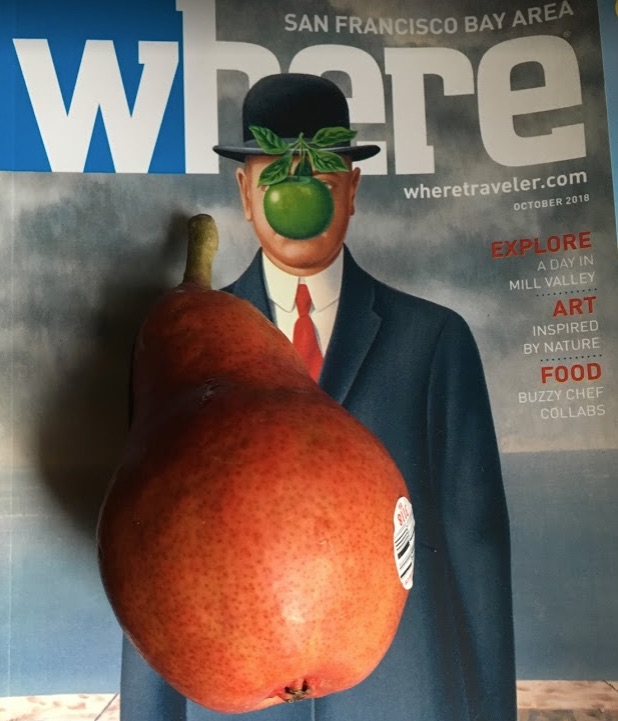
Hi Twitter Friends, I'm going to do a "Mini Really Rapid Review" of #IDWeek2018, looking for suggestions of what to cover. Fire away! Links appreciated. p.s. will explain the significance of the pear later. pic.twitter.com/oMk0PU9B5Z
— Paul Sax (@PaulSaxMD) October 6, 2018
As for the pear, it cost a staggering $4.64 in my hotel lobby. Remember when San Francisco was affordable? I don’t either.
At least I saved money on the flight out there.
October 2nd, 2018
Winner of Latest Cartoon Contest Proves Again That We ID Specialists Are a Different Breed
It is with a mixture of professional pride and embarrassment that I hereby present the winner of our last ID Cartoon Caption Contest:
Yikes. Talk about inside jokes.
Though the second-place finisher “Ah, no, I prescribed the AEROSOLIZED, not PARASOL-ized form” mounted a late charge, the geeky reference to Listeria monocytogenes and its “umbrella motility” held out for the win.
Let’s pause for a moment to consider the sheer obscurity of this winning caption:
- It involves Listeria monocytogenes — a relatively rare infection (despite its prominence in medical school curricula).
- It requires knowing that listeria causes meningitis. Astute observers of the cartoon will note that the umbrella may be in the lining of the guy’s brain.
- Finally — and easily most obscurely — you have to know that when listeria is inoculated vertically into soft motility agar, growth of the organism produces umbrella-like lateral extensions from the stab line.
Ha ha!
Special thanks to Sébastien Poulin for being the first to submit it, and doing so all the way from Canada. That couldn’t have been easy, what with the latest controversies in US-Canada relations.
As is customary, Sebastien will receive a lifetime free subscription to this blog. Perhaps he’ll even come this week to the annual gathering of ID nerds like him in San Francisco to pick up his prize.
Not surprisingly, the caption completely baffled my sister Anne, creator of the above cartoon (and not an ID doctor). She had no idea she was going to elicit listeria associations with her skillful and silly drawing. Our astute editors at NEJM Journal Watch were similarly perplexed, but too embarrassed to ask me to explain the joke.
(Now do you get it?)
While we’re all enjoying that bit of ID-related humor — and we are, aren’t we? — allow me to share this spot-on parody of how we ID doctors can obsess over obscure details (like umbrella motility) when sometimes those consulting us just want to know what to do:
For the record, that’s Brown medical resident Zoe Weiss, poking affectionate fun at her revered ID attending Dimitrios Farmakiotis.
(All “actors” gave permission to post this video, by the way. Send the lawyers away.)
And since Zoe made the best possible choice when it comes to her upcoming subspecialty training (ID, of course), she will one day play the same important role as Dimitrios — lecturing, um I mean teaching, impressionable residents.
Hope to see you at IDWeek!