An ongoing dialogue on HIV/AIDS, infectious diseases,
March 3rd, 2019
A Few Thoughts on the Day Before CROI — Our Best (and Quirkiest) Scientific Meeting
As I’ve written here numerous times, the Conference on Retroviruses and Opportunistic Infections — or “CROI” (rhymes with “toy”) — is the best of the scientific meetings on HIV. It starts March 4 in Seattle.
Bringing together the perfect blend of clinical, translational, and epidemiologic research, CROI consistently boasts the highest density of worthwhile content in any of our meetings. Even in years with no major breakthroughs, scientists present numerous studies that move the field forward in important ways.
So yay for CROI. I’m a huge fan, never miss it.
But … it has always had its unusual qualities, some of them lovable, others just … quirky.
For example:
1. You have to apply. All meetings require registration — name, address, affiliation, other demographic data — but only CROI asks for a list of publications. While no one is rejected based on their lack of productivity (I hope), this process always makes me feel weird. Is there a panel going through this list, looking at citations, impact factors, h-index, Altmetric scores?
At least they no longer ask for my MCATs and kids’ APGAR scores.
(Kidding.)
2. Distinctive swag. Upon registering, you are handed a stylish backpack, emblazoned with the letters CROI, the name of the city, and a graphic of a virion. Refreshingly free of pharmaceutical advertising, the bags are nice enough that my (APGAR-approved) children periodically carried them to school, garnering either mystification or, very rarely, an insider acknowledgment from other HIV specialists (or their kids).
But there’s more — inside the bags there’s a square notebook that would please even the most discerning graphic designer, and a nifty pen. The notebook sometimes has faint gridlines, in case you want to sketch out a Kaplan-Meier plot.
Did I mention the backpacks?
Check out the #CROI2019 backpack available at CROI check-in. pic.twitter.com/RP6IijCaQ4
— IAS–USA (@IAS_USA) March 1, 2019
3. It’s cold. Held in February or March, most commonly in Seattle or Boston (or in years past, Chicago), CROI will never attract participants eager to work on their suntans. This meeting is for serious scientific exchange, people! As if to prove this point, the Climate Gods even made Atlanta absolutely freezing in 2013 — the only year the meeting took place in the South.
Since February and March are still very much winter, a few notable snowstorms have hit the Boston CROIs — including two at both ends of the meeting last year. But let the records show that, owing to some marvellous cosmic luck, Seattle hosted the meeting during Boston’s 2015 “Snowmageddon.”
Remember that?
4. Now there’s a test. New this year, registrants received this via email:
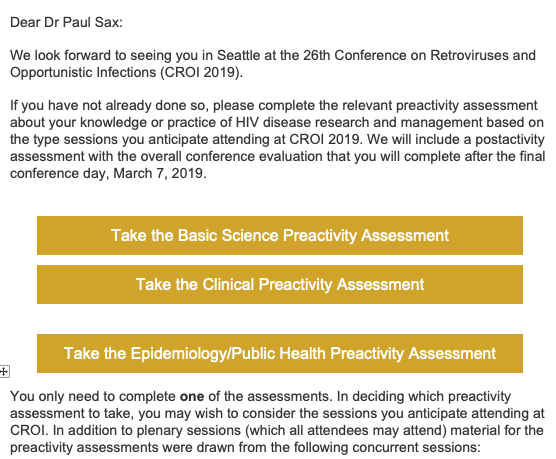
I’ve been assured by one of the CROI organizers that this test is for CME purposes, and that scores won’t be made public.
And that’s a good thing, too, since the questions are unbelievably difficult — if we had questions this tough on the ID board exams, hardly anyone would pass.
(Maybe I should concentrate more on my work, and stop worrying about my suntan.)
To be fair, CROI is a lot less quirky than it used to be. The conference used to release its upcoming dates less than a year before the event, wreaking havoc on academic and clinical schedules — and triggering some serious sleuthing,with leaks on the date coming from some very high profile sources.
(If you’re reading this now, Principal Source of Embargoed CROI Dates, your secret is still good with me.)
Hooray, those days are over, and we now get plenty of notice! CROI 2020 will be in Boston, March 8-11, so save the date, and bring your overcoat.
Which reminds me — got a funny email after last year’s Boston meeting; mystery still unsolved!
Just got this from a person I met at #CROI2018:
Possibilities:
1) He doesn't know I'm from Boston.
2) He meant the note for someone else.
3) He THINKS I'm someone else.
4) He's been cutting/pasting the same note to everyone. pic.twitter.com/6ol2i2gxrQ— Paul Sax (@PaulSaxMD) March 9, 2018
February 24th, 2019
Why Choose Infectious Diseases as a Medical Specialty? Here’s the Beginning of My Story, with Bonus Podcast

I got this from gefilte fish? oy …
Forgive the autobiographical nature of this post, but here’s a recap on how I started down the the path to becoming an ID doctor.
To begin, understand that my first year of medical school was rough going.
In hindsight, this wasn’t surprising. After majoring in English during college (with a minor in the Harvard Lampoon to develop good study habits, ha ha ha), then spending a year abroad teaching, I found medical school’s unrelenting science courses and lecture hours an unpleasant blend of overwhelming and tedious.
Meanwhile, most of my classmates were cruising — including my future spouse, who attended all the lectures, took meticulous notes in colored pencil, and aced every test.
Ouch.
Any jealousy I felt about her breezing through the first year of med school was more than compensated for by gratitude — hard to imagine I’d have made it to second year without her.
And so glad I stuck around, because our second-year microbiology course gave me a strong signal that I might actually like this medical business. Led by the articulate and worldly Dr. Arnold Weinberg, and ably taught by other superb teachers and section leaders, the course was endlessly stimulating, the very opposite of the metabolic pathways I had (barely) memorized during first-year biochemistry. I looked forward to every microbiology lecture and every lab.
I loved this course for multiple reasons:
- Each disease had a story. The legionnaires’ convention in Philadelphia, the contaminated cooling tower of the hotel’s air conditioning system, and the (appropriately named) new disease due to Legionella pneumophila! The makers of gefilte fish at home who later developed Diphyllobothrium latum! The river rafters from Ethiopia who developed fever, myalgias, and eosinophilia and were ultimately diagnosed with Schistosoma mansoni! The visitor to the deserts of southern California with fever, pneumonia, skin lesions, and Coccidioides immitis!
- The names of the bugs were so poetic. Just look at that previous paragraph — each microbe a musical mouthful of letters and syllables. Even the more common bugs sounded exotic and fascinating to my ears: Streptococcus pyogenes, Enterobacter (now Klebsiella) aerogenes, Staphylococcus saprophyticus, Pseudomonas aeruginosa, Plasmodium falciparum. Just read those names out loud — heaven! And does anything sound scarier than Toxoplasma gondii?
- Even the lab was fun. My experience in science labs had at that point been limited to dry exercises in organic chemistry as an undergraduate, and some snooze-worthy histology and pathology labs during first year of medical school. Microbiology lab, however, was a whole new ballgame — culture plates, strange smells, actually seeing the bacteria and parasites under the microscope, and helminths in clear vials. It didn’t hurt that one of my section leaders was the extraordinary pathologist Dr. Franz von Lichtenberg. Franz’s enthusiasm for the material was 100% communicable — and yes, I chose that word intentionally.
- This new, mysterious disease — AIDS — had just been identified. It was during microbiology that we first had lectures on this new problem. We didn’t know yet what caused AIDS, but a sexually- and blood-transmitted infection seemed likely — one of our lecturers posited that it would be cytomegalovirus. (He was wrong.) Plus, the vast majority of the complications were infectious, most of them rarely seen in patients with normal immune systems. Could there be anything more fascinating — and important — than an infectious disease that could be rapidly lethal in previously healthy people?
After microbiology, the rest of medicine became much more interesting. Cardiology had endocarditis and rheumatic fever; pulmonary had pneumonia, empyema, and lung abscess; renal had pyelonephritis; neurology had meningitis, encephalitis, and brain abscess. You get the idea.
Everyone I knew thought I’d end up an ID specialist. After all, I was the only one who had memorized all of the oral and intravenous cephalosporins, a party trick I still bring out for the right company if they ask nicely.
And after a brief flirtation with cardiology, I haven’t regretted my choice of ID one bit.
Medical school microbiology was my start down the road toward ID, but there are multiple other reasons I chose it. Another ID enthusiast is my longtime friend and colleague, Dr. Raphael (Raphy) Landovitz from UCLA. To elucidate these reasons further, I invited him to join me on an Open Forum Infectious Diseases podcast, where we drafted the Top Five Reasons to Choose ID as a Specialty.
You can listen now on the site, and even read along with the transcript.
Or grab it on iTunes, or Overcast, or various other podcast charging stations.
Have fun.
February 18th, 2019
Yes, Many People Are “Pleasant” or “Delightful,” Even “Lovely” — But Should That Be in the Medical Note?

Isn’t she “lovely”? Could be, but keep it out of the note!
When writing medical notes, some clinicians include an appreciation of their patient’s personality and disposition in their opening line (the “Chief Complaint”), or when they’re wrapping up (in the “Assessment and Plan”), or in both locations.
You know — it goes like this:
“CC: Ms. Smith is a very pleasant 62-year-old woman admitted with …”
or:
“A/P: To summarize, Mr. Jones is a delightful 89-year-old man presenting with …”
or:
“CC: This lovely 74-year-old retired school teacher was in her usual state of health until …”
Yikes, not a fan of this practice.
Am I just being curmudgeonly and negative? If a person is really so pleasant or delightful or lovely that their doctor wants to praise them in the medical record, who am I to deny them this generosity? Or deprive their patients of this honor?
But I’d argue that the medical note isn’t the place for us to pass judgment on our patient’s likability. What does this imply about those we don’t call pleasant?
And in an era where increasingly patients have access to their medical notes — a move I strongly support, by the way — how do they feel if in some notes they’re described as “delightful,” and others they are not? What if they’re having a bad day, reducing their loveliness? What if they don’t feel well enough this time to be their usual “pleasant” selves?
Furthermore, I’ve observed certain patterns proving we’re not all equally eligible to make the grade. First, women earn way more “praise” (ahem) than men:
- “Pleasant”: 60% women
- “Delightful”: 75% women
- “Lovely”: 90% women
(Data from a highly scientific review of several thousand medical charts. Really.)
Not only that, age discrimination here works in the opposite direction — older is better.
In fact, every decade beyond age 60 yields a greater likelihood of earning one of these adjectives. Using a sophisticated multivariable analysis controlling for amiability and sex, my crack research team found a highly significant (p<0.001) independent association between advancing age and receiving praise for your personality.
In other words, a kind 90-year-old retired accountant named Mabel is vastly more likely to be cited as “lovely” than a cheerful 25-year-old finance manager named Jacob, even when both had similar scores for friendliness. Is that fair?
But — if you think about it for a moment, doesn’t this “lovely” imply something demeaning and patronizing about the label? Of course it does.
Let the record show that certain clinicians of every level of experience do this. Ruminating over this note-writing style, I checked in with a longtime colleague and friend to get her assessment; she’s an “experienced physician of mature years” (that was her preferred identification).
In a twist, she wrote back the following:
Hi. Generally I agree with you.
… beat
… beat
…
er, except for this. Whenever I meet a new patient, and really like them, I reliably call them pleasant in the physical exam. (Note: I never ever called anyone delightful or lovely. That seems patronizing.) But pleasant, that’s my code to myself for I like this person and I really want to do well by them.
I maintain that Pleasant is a legitimate part of the objective evaluation: it means someone is actually able to relate politely to a stranger without getting all tangled up in whatever their stuff is. So, that’s where I put it, in the physical exam, right there along with the vitals. Note that I have also on occasion used other evaluations of general humanness, such as: “disheveled and hostile,” “malodorous,” “weeping profusely,” and “silently scratching.” All germane, if you ask me.
I’ll give her credit for putting the “pleasant” description in the physical exam — this is where we put our observations, after all — and leaving out the “delightful” and “lovely” labels.
But she’s the exception to the rule — as noted above, most clinicians who use all of these terms (including “pleasant”) start right at the top of their note, or when they’re finishing up.
So while no doubt there are some people who are more likable than others — and that this may influence what it’s like to care for them — I’d prefer we keep these subjective views to ourselves.
February 10th, 2019
Six Musings Triggered by the Latest Measles Outbreak
Source: CDC
In 2018, there were 372 cases of measles in the United States, the largest number since 2014. This year, we’ve already had 79 cases, many from a large outbreak in the Pacific Northwest — where anti-vaccine proponents recently protested efforts to restrict nonmedical vaccine exemptions.
A few ruminations triggered by this outbreak.
1. The vaccine is extraordinarily effective at preventing measles, lulling us into a false sense of security. After many years of clinical practice, the total number of measles cases seen by my wife (a pediatrician) and me (an infectious diseases specialist) is … two. We’ve both seen one.
The measles vaccine is wonderfully effective — think how contagious it is! — but the net result is that most clinicians in the United States have never seen a case. Here, take a look at this poll:
Simple poll for you ID and non-ID clinicians out there. If you answer Yes to the question, please help by providing the context (when it was, where it was, why it happened, etc).
Have you seen a case of measles in the post-measles vaccine era?— Paul Sax (@PaulSaxMD) February 10, 2019
Around three-quarters of the clinicians have never seen a single case. If the poll had been limited to US doctors and nurses, even more would have no personal contact with the disease. Non-clinicians, of course, have even less direct experience.
The effectiveness of the vaccine indirectly fuels some of the vaccine refusers — it’s the victim of its own success. Some may not believe it’s a serious disease since they’ve never seen it. Others might think it’s too rare to cause their child a problem, so why vaccinate? (More on this latter ungenerous line of thinking below.)
Both views are terribly short-sighted. Regular readers of this blog will undoubtedly agree, but how can we overcome this?
2. The anti-vaccine effort spans the entire political, economic, religious, and racial spectrum. Rich and poor; left, right, center; observant, agnostic, atheist — does not seem to matter.
We’ve got celebrity “experts” such as Jenny McCarthy and Jim Carrey; “environmentalist” and lawyer Robert F. Kennedy Jr who, since he’s related to a former president, gets tons of attention; a Hasidic Jewish community in Brooklyn; immigrants from Somalia in Minnesota. There are people up and down the socioeconomic spectrum who just don’t trust either the science, or the government, or both.
Homeopaths and crystal lovers might be leery of — some would say paranoid about — hidden toxins, chemicals, and preservatives in vaccines. They prefer “natural” immunity to the vaccine-induced kind, nevermind that measles itself can be fatal.
Libertarians want the government out of their health care choices, period. Recent immigrants might be susceptible to persuasive anti-science hucksters — this is what happened in Minnesota.
How does one target educational efforts about the importance of immunizations to such a diverse group?
3. The cost of childhood immunizations is no impediment to receiving them. Our fragmented US healthcare system definitely gets this one right — childhood immunizations are covered essentially everywhere, regardless of a family’s ability to pay.
Why might this be? Child immunizations do it all — they are highly effective in preventing illness and death, very safe, reasonably priced, and actually save our society money. Does anything else we do in medicine have such strong personal, public health, and economic data supporting their use?
4. Eliminating nonmedical vaccine exemptions is absolutely critical for maintaining herd immunity. Several years ago, I interviewed Dr. Samuel Katz, a physician-scientist who played a critical role in developing the measles vaccine. (Transcript here, podcast here at the bottom of the page.)
After he provided an overview of the discovery of the attenuated measles virus strain and the early clinical trials, I asked him to comment on on the anti-vaccine movement. To my surprise, he was relatively sympathetic, calling the group “vaccine hesitant” rather than “vaccine refusers.”
(I confess to being much less charitable, viewing parents who refuse vaccines for their children for nonmedical reasons as exhibiting an extreme form of selfishness and antisocial behavior that borders on criminal.)
However, on one fact he was quite clear — the critical role of vaccine school-entry requirements in keeping measles at bay. These regulations are much stronger here than in most of Europe, and as a result, Europe’s measles outbreaks are far worse. In 2018 alone, Europe had over 82,000 cases and 72 deaths — three times the number of cases they had in 2017, and over 200 times the number of cases here.
As for religious exemptions, there’s a good chance many (most? all?) reflect personal beliefs, not something specifically forbidden by a religion. Where does it state in the Bible, the Torah, the Koran, or in any religious text that vaccines are prohibited? And why should religious exemptions be permitted for vaccines, and not other safety codes and laws? As noted in this excellent editorial in The Boston Globe, “There’s no religious exemption from the fire code or the seat-belt law.”
5. Many people refuse the vaccine for their kids because they just want a free ride. I imagine the thinking goes like this:
Hey, if everyone else gets vaccinated, then measles will be so uncommon that my kid won’t need it. And I heard from my yoga instructor that this is what she did, and her kid has been fine — so that’s what we’re doing too.
You want proof? Vaccine demand is up 500% in the county experiencing the outbreak.
Guess it doesn’t take much to overcome those “philosophical” or “religious” objections to the measles vaccine! For more on this line of selfish and privileged thinking, read this superb post by Dr. Amy Tuteur, who writes:
Nothing says “privilege” quite like refusing the same vaccines that an impoverished mother in a developing country would trudge five miles to get for her child. No sooner did the privilege disappear — destroyed by anti-vaxxers themselves whose choices have ushered back a deadly public scourge — then the anti-vaxxers folded.
6. Many stock photos of vaccine administration are absolutely terrible. How many times have you read a piece online or in a magazine that shows a giant needle and a crying kid? Sometimes there’s also a scary-looking doctor or nurse.
Seth Mnookin, Professor of Comparative Media Studies/Writing at MIT, wrote an excellent book on the vaccine controversy. He also provided this choice example of bad vaccine images in the media:
Worst possible art choice for this @slate piece about understanding root of vaccine fears. Pictures of needles going into babies make people anxious & uncomfortable. Regartdless of content of article, yr using anti-vaccine propoganda to illustrate it. https://t.co/KRuvEU5HBW
— Seth Mnookin (@sethmnookin) February 5, 2019
I agree entirely that far better would be to show pictures of happy, measles-free children, or parents with kids visiting a friendly-looking doctor’s office — or at least anything else besides a little kid and a big needle!
As for the outbreak in Washington, I am hopeful that the surge in immunizations will get the new infections quickly under control.
After all, it doesn’t matter why you immunize your kids — it just matters that you do it.
Herd immunity in one minute — remember, we need at least 90% immunized for it to work for measles!
February 3rd, 2019
An “Interview” with the OVIVA Study of Oral vs. IV Antibiotics for Osteomyelitis
An “interview” inspired by publication of a landmark clinical trial. All responses written by me — but be assured, they are based on reading the paper, the accompanying editorial, the supplemental appendix, hundreds of comments on Twitter (some of them from the study investigators), and even a few generous comments from the the senior author in response to email queries.
Me: Thank you for joining us today, and welcome to the official world of published medical literature. We’ve been waiting quite a while with eager anticipation. Can you start out by introducing yourself?
OVIVA: Sure, thanks for having me. My name is OVIVA, which stands for “Oral vs. Intravenous Antibiotics” for bone and joint infections. Clever, eh?
Me: Yes, pretty good — though these makers of this “maple water” might object. Tell me a little about yourself.
OVIVA: Well, as you know, it’s a longstanding view that adults with bone and joint infections need prolonged IV therapy for optimal treatment. But this is inconvenient, expensive, and doesn’t make a whole lot of sense since many antibiotics are well-absorbed when taken orally. Plus, the pediatricians have treated osteomyelitis with oral therapy successfully for years. So we set out to challenge this assumption that you need to use IV.
Me: Great idea! Where was it done, and who did it include?
OVIVA: We did it at 26 sites in Great Britain, from 2010 to 2015 — solidly pre-Brexit — and enrolled around 1000 people. Eligible participants had a bone or joint infection, and would normally be treated with at least 6 weeks of intravenous antibiotics. We included people who had surgery (such as removal of an infected joint or hardware, or debridement), and those who didn’t. The treating physicians chose the antibiotics based on cultures and their clinical practice. These are deliberately very broad inclusion criteria — we wanted to make it as representative of the “real world” as possible.
Me: Interesting choice — really drives home the “pragmatic strategy” in clinical trials design. Any notable exclusions?
OVIVA: We excluded people with Staph aureus bacteremia or endocarditis, since at that time, oral therapy would not have been standard of care — this was way before POET. And since we had to consider the possibility that half the participants would get IV therapy, we did not want to include anyone for whom this treatment might not be completed — hence few (if any) participants were enrolled with active injection drug use. [It’s not clear if anyone who uses injection drugs is in the study.]
Me: So what did you find?
OVIVA: Here’s the big news: Oral therapy was clearly non-inferior to IV. Definitive treatment failure at 1 year occurred in 13% of the oral group and 15% of the IV group. These results held up in several sensitivity analyses, including something we called a “worst case” outcome. In this approach, we take the participants with missing data, and assume all these participants who were randomly assigned to receive oral therapy and no participants who were randomly assigned to receive intravenous therapy had definitive treatment failure. This introduced the worst possible bias against the oral strategy — and it was still non-inferior. Here, take a look at this figure:
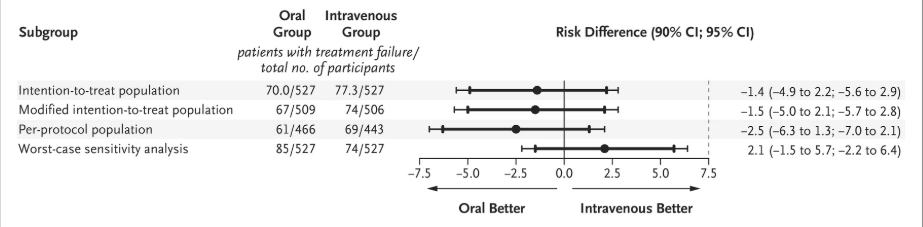
Me: Very reassuring that the point estimates for your baseline analyses all numerically favored oral therapy. And clever job with that “worst case” scenario — good one for the doubters.
OVIVA: Thanks. I should mention that we were worried that the oral group would receive much longer total treatment, but this wasn’t the case — the median duration of therapy was 78 days in the intravenous group and 71 days in the oral group. Plus, even though there was more adjunctive rifampin use in the oral group, outcomes didn’t vary significantly whether this strategy was chosen.
Me: Any other results you’d like to highlight?
OVIVA: Another plus — those getting oral therapy had shorter hospitalizations and fewer complications (in particular, line-related complications). This approach to treatment of osteomyelitis will save plenty of pounds/euros/dollars/etc. So oral therapy can save money, be safer, and be just as effective. Is that what you Yanks would call a home run? Or a touchdown?
Me: Vastly prefer the former, thank you. And no doubt these are great results — congratulations for being such a challenging, important, and rigorously conducted study. Highly likely to change clinical practice!
OVIVA (beaming): Aw shucks — that’s very kind of you.
Me: However, as as noted in this excellent editorial, it might take a while — this particular study might not be enough for certain clinicians, and earlier studies were smaller (or forgotten). And some of us might have trouble convincing our surgical colleagues that their patient with osteomyelitis can be treated with “only” oral antibiotics after debridement — for many surgeons, “more” equals “better.”
OVIVA: Yes, our surgeons are like your surgeons.
Me: May I raise a few additional questions and concerns?
OVIVA: Of course — this is your blog, and you’re writing this made-up interview!
Me: I noted that the oral regimens selected by the clinicians were mostly quinolones, doxycycline, and clindamycin — relatively few got oral penicillins, and oral cephalosporins didn’t get chosen at all. And no love for trimethoprim-sulfamethoxazole in Britain? No linezolid?
OVIVA: We did not mandate antibiotic selection — the antibiotics chosen represented clinical practice at the sites. Oral cephalosporins are hardly ever used in Britain, and not enough people chose “cotrimoxazole” (that’s what we call it) to warrant a separate line-item in the report. Some chose linezolid, but not for more than two weeks.
Me: Understood. But here’s another way of looking at the results — if clinicians generally select highly bioavailable oral antibiotics for treatment of bone and joint infections, then oral is non-inferior to IV. This might be overinterpreting the subgroup analysis, but the forest plot for planned oral treatment even hints at this conclusion:
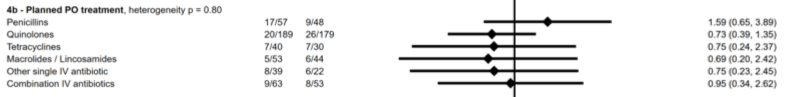
OVIVA: Hey, you read the Supplemental Appendix! Very impressed. In my defense, let me quote from the paper, which states: “We did not seek to compare specific antibiotic agents or to stipulate which agents should be used.” Someone else might choose to do that sort of study. We simply can’t say whether one oral strategy was better than another.
Me: Got it. But clinicians will read this paper and want guidance over what specific antibiotic regimen to use for a specific bug for a specific indication — this study can only give the broad view that oral is non-inferior to IV. Not much granularity here. And from a practical standard, we’d all appreciate more information about dosing.
OVIVA: Hey, I can’t be all things to all people. Rest assured, more analyses and reports are coming. And remember, we relied on the expertise of the ID docs at the sites, whom I assume were among the smartest — if not the smartest — clinicians responsible for choosing the treatment.
Me: No argument from me on that point.
January 27th, 2019
For Our Stable HIV Patients, Why Are We Still Sending All These Lab Tests So Often?
 Interesting query from a colleague recently:
Interesting query from a colleague recently:
I’m a community ID doc in the trenches (the measles trenches at present) with an HIV question. Why do we still check CBCs & chem panels every 3-6 months in our HIV patients? Particularly our well-controlled, virologically-suppressed patients? This strikes me as a tremendous waste. I haven’t been in practice that long, but I can count on one hand the number of times these routine labs have led to a change in ART (and even then, it was probably a patient on TDF, which I don’t use much any more). Is this an evidence-based practice? Or a vestige of an earlier era of more toxic drugs?
Thanks!
Andrew
Andrew raises an important question — do the guidelines for laboratory monitoring still make sense when our HIV treatments have become so safe and effective?
Below I’ve summarized the labs recommended by the DHHS Guidelines for our stable patients — the people who have been virally suppressed on ART for years. In italics, a bit of commentary.
- CD4 cell count — if CD4 < 300, every 3-6 months; if CD4 300-500, every 12 months; if > 500, optional. Wow, that’s complicated. How about never? One could easily argue that CD4 monitoring is only needed in those very rare patients who have persistently low CD4 (e.g., < 200) despite long-term viral suppression. Remember, HIV treatment should not be changed based on CD4 results alone.
- HIV RNA (viral load) — every 6 months. While the viral load is absolutely critical for monitoring adherence, does a strategy of twice-yearly measurement make sense for patients who have been on effective treatment for a gazillion years, are on a perfectly good regimen, and have never failed therapy?
- Basic chemistries, LFTs, and CBC (when measuring CD4) — every 6 months. This was the group of tests alluded to by Andrew in the above email, and I agree that they rarely pick up something of HIV- or ART-related concern with current treatments. Exceptions would be for patients with known comorbidities — but this is a different indication for testing. About the only good thing you can say about this testing is that it’s cheap, at least compared to CD4s and viral loads.
- Urinalysis — yearly if on TAF or TDF. Certainly this makes sense with TDF, and again also when there are concomitant risk factors for renal disease (diabetes, hypertension). But in an otherwise healthy young person not on a TDF-based regimen? The incidence of clinically important abnormalities with this yearly screen must be extraordinarily low.
Here, then, is a revised (and deliberately provocative) recommendation for monitoring the otherwise healthy people (who happen to have HIV), and who have long-term viral suppression — let’s say at least 5 years < 200, just to be safe. Let’s also assume they are also currently receiving a recommended regimen that does not include TDF:
- HIV RNA (viral load) — yearly.
- CD4 cell count — never.
- All other tests (chemistries, renal function, LFTs, CBC, urinalysis) — at comparable age-appropriate or comorbidity-appropriate frequency to HIV-negative people.
When I’ve floated this idea by certain colleagues, they frequently cite the asymptomatic sexually transmitted infections they’ve picked up in their twice-yearly (or more frequent) monitoring.
I’d argue that this reflects an individual’s STI risk, which is not the same in all people with HIV. By all means, continue to screen for STIs when clinically indicated, and the same goes for underlying medical problems that increasingly arise during aging.
So to test this revised strategy, let’s imagine a clinical study:
Eligible: Stable on guidelines-approved ART; no history of virologic failure or treatment interruption; HIV < 200 on all measurements during the past 5 years.
Intervention: Randomized to 1) guidelines-recommended monitoring, or 2) HIV RNA once-yearly, other testing as indicated by demographics, clinical status, comorbid conditions, STI risk.
Primary endpoint: Virologic suppression at the end of the study.
Secondary endpoints: Occurrence/diagnosis of HIV or non-HIV-related comorbidities; cost (to healthcare system); cost (to patient).
And, since we’re talking about a way to reduce office visits and healthcare utilization, how about this recent “appointment” in Alaska?
https://youtu.be/oqzso15FRlM
January 22nd, 2019
Unanswerable Questions in Infectious Diseases — Treatment Duration in Endocarditis: 4 Weeks, 6 Weeks, Other?
National Library of Medicine
Time to get back to some tough clinical decisions. It’s been a while.
We’ve done The Abdominal Collection and Duration of Antimicrobial Therapy, Persistent MRSA Bacteremia, and The Positive Cultures for Candida in an ICU Patient.
However, that series of posts appeared here in early 2014, which means it’s been 5 years with no “Unanswerable Questions.”
Lest you think that all Unanswerable Questions have been answered — ha — here’s another one, inspired by a flurry of papers recently on a favorite topic, duration of antimicrobial therapy.
To summarize virtually all of them — shorter is usually as good, if not better, than longer. Nice editorial here.
Before we get to the case, an up-front apology that the question might seem simple. But I assure you, the answer is anything but straightforward. Bold prediction: there will be a substantial divergence in responses.
Additionally, while the question may not seem like such a big deal, there are many interested parties eagerly awaiting our answer — including our hospitalist, cardiology, and primary care colleagues, diverse insurance plans, homecare companies, outpatient pharmacies, and skilled nursing facilities. Most importantly, our patients and their families care a lot, too.
And even though the correct answer to “How long should I treat?” is “Long enough” (thank you, Bob Rubin!), this doesn’t change the fact that consulting services really want to know a precise answer. Ironic, huh?
Here’s the case, an amalgam of many seen over the years:
A 52 year old man is admitted with fever. On exam, he has a temperature of 101.5F and a loud systolic murmur. Two sets of admission blood cultures grow methicillin-sensitive Staph aureus. A cardiac ECHO shows a bicuspid aortic valve with a 0.5-cm vegetation.
He is treated with oxacillin; follow-up blood cultures are negative by hospital day 3, and fevers slowly resolve. A peripherally inserted central catheter (PICC) is placed on hospital day 5, and cefazolin replaces oxacillin in anticipation of discharge home on IV antibiotics.
The patient, the medical team, the homecare company, and your OPAT colleagues all await a specific “stop date” for the IV cefazolin.
The question:
If he has a clinically stable course (no further positive cultures, no recurrent fevers, and no metastatic sites of infection), how long would you treat him with intravenous antibiotics?
Before you answer, you’re welcome to look at the guidelines — this is an open-book blog, after all:
- American Heart Association
- European Society of Cardiology
- British Society for Antimicrobial Chemotherapy
Or, you could just wing it based on your clinical experience and judgment, or cite the POET study if you’re feeling cutting edge. Clock starts the day of the first negative blood culture.
And please defend your choice in the comments section, especially if you choose option 4!
(Apologies to Drs. Wald-Dicker and Spellberg for the Days-of-the-Week Units.)
January 13th, 2019
Are We ID Doctors Really So Unhappy Outside of Work?
Must be a rheumatologist or otolaryngologist. (Source: National Library of Congress.)
Medscape released their 2019 Physician Lifestyle & Happiness Report, and the results aren’t pretty for a certain cognitive specialty, one commonly abbreviated “ID.”
Out of 29 medical and surgical specialties, infectious diseases physicians ranked second to last when responding to a 7-point scale rating on their happiness. Only neurologists were gloomier than we were during their off-hours.
Rheumatologists and otolaryngologists finished first and second, smiling all the way.
The news was even worse for ID docs in “self-esteem,” where we ranked last, right behind oncology and internal medicine. Meanwhile, the plastic surgeons, urologists, and ophthalmologists scored highest on this measure.
Some of my ID colleagues have commented about possible methodologic issues with the survey, as the results don’t correlate with our own happy non-work lives.
For example, Dr. Dan McQuillen weighed in with this critique:
Much like crappy data in major salary surveys, ID docs were only 1% of this sample, roughly 150 of 15,069 docs surveyed. @IDSAInfo salary surveys w/ larger sample size have shown small sample size data to be inaccurate. Hard to take 150 responses and generalize to > 11K ID docs.
— Dan McQuillen (@McQHoya81) January 11, 2019
I have a query into Medscape to get more information about these concerns, and they’ve kindly agreed to get back to me. For example, I don’t understand how the 7-point happiness scale translated into the percentages shown in the linked figure.
More importantly, what were the demographics of these 150 ID respondents, and how do they compare with ID practitioners as a whole?
Methodology notwithstanding, it’s worth postulating at least a few reasons why indeed we might be somewhat less happy outside work than other doctors right now. So here goes:
1. The current political climate. It’s no secret that ID doctors skew strongly to the left when it comes to politics. I can’t be the only ID doctor who, on a certain Wednesday in early November 2016, went to work and encountered several colleagues and trainees literally in tears.
(Or maybe you were in tears yourself. It’s OK to admit that to other ID docs.)
I’ve discussed this issue before, postulating that the “safety net” and inclusive ethos of ID doctors was more in line with one particular party than the other. Some even choose ID as a specialty because of these political leanings. Here again are the facts, which could very well contribute to a lower happiness score during the recent survey period:
I can count on one hand the number of ID/HIV docs I know who are openly Republicans, and still have fingers left. https://t.co/m2ewtxpcwd pic.twitter.com/90gEaIWISM
— Paul Sax (@PaulSaxMD) October 6, 2016
How about today, two-plus years later? Decent chance that the fraction who have registered red is even smaller.
2. Salaries, debts, and money concerns in general. During a time when certain government workers are sadly not being paid at all (see #1, above), it seems petty to complain about ID doctor salaries — which, in this latest comprehensive salary report, aren’t really that bad:
In general, full-time ID physicians in private practice (n = 366) reported higher incomes, with a median annual salary of $260 000, than respondents employed by hospitals, clinics, or academic medical centers (median salaries of $237 500 and $181 500, respectively).
But context is everything, and here are some important considerations. Students graduate from medical school with on average nearly $200,000 in medical school debt, a hefty sum to pay down with these ID salaries.
Furthermore, ID doctors are often paid less than hospitalists and primary care physicians — doctors who have spent less time training, and frequently work fewer hours, than ID doctors. And all of us cognitive clinicians can only dream of accumulating the RVUs (and hence revenues) of a plastic surgeon, urologist, or ophthalmologist.
Hey! Those are the docs who just happen to lead in the “self-esteem” metric! Hmmm.
3. We’re by nature big-time worriers. Obsessive to a fault, we ID doctors take the most detailed histories, frequently contact the outside labs, march down to the radiologists or ECHO room or microbiology lab to review primary data, write the longest (too long) notes, and still — we live in terror of missing something.
Could it be that this personality trait doesn’t translate into happiness? Maybe the sensation that our work is never done translates into non-work “worry hours” that cloud the responses to a happiness survey.
Imagine the thought bubble of some of us as we head home from work:
How can I be happy at home when that patient with Staph aureus on a urine culture may have bacteremia? Or that other patient with a positive IGRA could develop active tuberculosis when starting etanercept? Or that person being discharged on IV antibiotics won’t have close follow-up? Or that guy who missed his HIV follow-up appointment might have stopped ART? Or that patient getting blasted with immunosuppression for graft-versus-host disease might have an undiagnosed fungal infection? Or that person …
You get the idea.
4. Our work lives are so interesting, rewarding, and wonderful that everything else pales by comparison. This must be the explanation, right? For example, look what I accomplished at work just this last week — how could anything beat that?
Apologies for bragging, but I'm the proud owner of a new degree.
Cc'ing @NobelPrize , just in case this was the one missing piece. pic.twitter.com/q5Y83YKCu6— Paul Sax (@PaulSaxMD) January 9, 2019
So, what do you think? Is the Medscape survey valid?
January 6th, 2019
Rabies After Trip to India, Aortic Dissections with Quinolones, a Vaccine for Candida, Koala Bites, and More: A Welcome-to-2019 ID Link-o-Rama
From the Library of Congress, government shutdown notwithstanding.
As 2018 tips over into 2019, here are a bunch of ID- and HIV-related studies that, for one reason or another, haven’t made their way to this site yet — but still yearn for your attention:
- Cases of infective endocarditis have increased since release of the 2007 dental prophylaxis guidelines. Recall that those guidelines only recommended prophylaxis for patients at the highest risk of IE. The results of this population-based study suggest (but do not prove) that perhaps some moderate-risk patients should also receive antibiotic prophylaxis.
- A woman in Virginia died of rabies after being bitten by a puppy during a trip to India. Though rare, these horrific cases underscore the value of pre-travel counseling and immunizations for certain trips. And dogs (especially puppies) are cute and wonderful, but stay away from strays in countries that still have canine rabies!
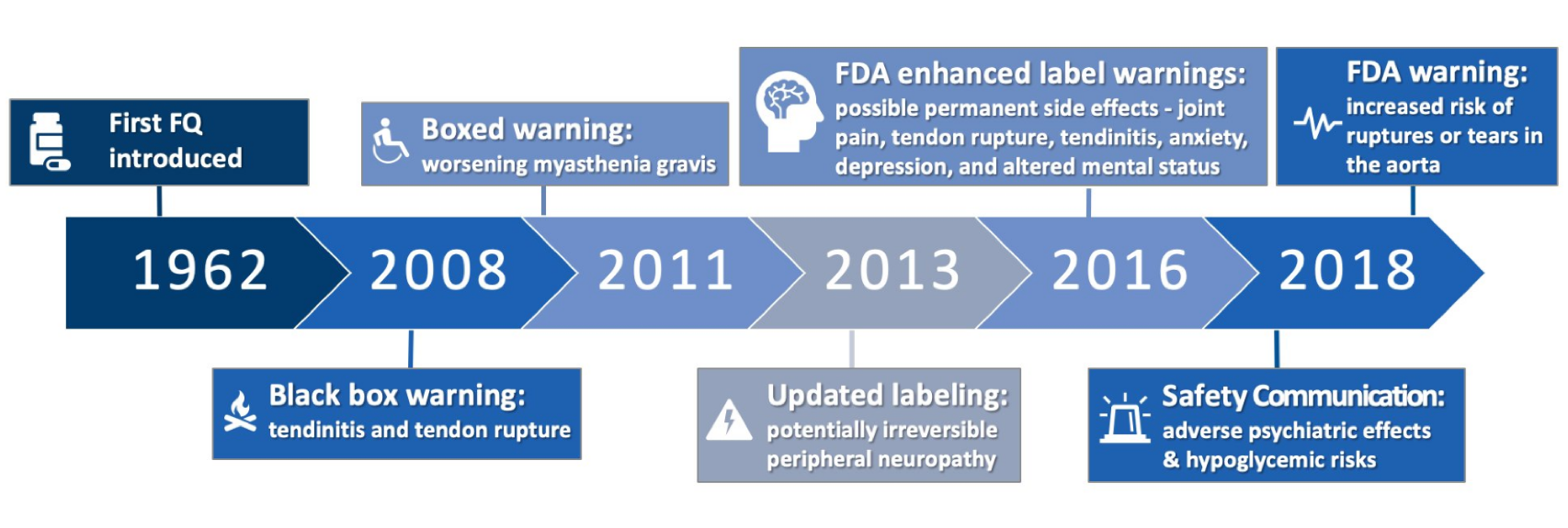
- Per FDA, fluoroquinolone use is linked to aortic dissections. As the parade of adverse events for this drug class marches on, it’s worth remembering that they remain extremely useful antimicrobials, especially in patients with complex infections. For those interested in the history of these alerts, here’s a great graphic, courtesy Travis Jones, PharmD:
- Dolutegravir monotherapy lands with a thud. In the linked study, nearly 10% failed by week 48 (some of whom developed resistance), prompting cessation of the study. A second study done in patients treated during early infection suggests the monotherapy strategy may work in patients with a low viral reservoir, but 1) we don’t measure reservoir in clinical practice, and 2) what’s the point?
- Starting antiretroviral therapy right away works great — even in the most difficult-to-treat populations. In a group of 216 patients with high rates of mental illness, substance use disorder, and homelessness, an astounding 95.8% achieved an HIV viral load <200 at least once after receiving immediate ART. I can’t imagine this occurring without integrase inhibitor-based therapy.
- A 39-year-old man nearly died of influenza last year, and now he’s publicizing the importance of the flu vaccine. I have tremendous admiration for people who endure such extreme hardship and then try to make something good out of the experience.
- A vaccine is under investigation for recurrent vulvovaginal candidiasis. This phase 2 study demonstrated safety and immunogenicity and hinted that it would be effective as well. For the record, there are currently zero vaccines for fungal infections.
- Here is a superb summary of the severe infrastructure problems fueling the national hepatitis A outbreaks. This disease is strongly linked to breakdowns in sanitation and hygiene, and not surprisingly have targeted the homeless and drug user populations.
- Complications are very high with outpatient parenteral antimicrobial therapy (OPAT) for severe Staph aureus infections. Roughly 33% experienced an adverse event, and 64% were readmitted at 90 days. Clearly a very tenuous patient population! And will Dr. Spellberg be right in his bold prediction?
- In North Carolina, infective endocarditis related to drug use has increased more than 12-fold over the past 10 years. As I’ve noted numerous times before, this dramatic rise in drug-use-related endovascular infections is one of the most profound changes in ID since starting practice in the early 1990s.
- Add wound botulism to the list of infectious complications of injection drug use. These cases in California involved black tar heroin, which is made mostly in Mexico. During transport inside car tires and other unsanitary locations, it may be exposed to soil containing Clostridium botulinum spores.
- Using both pneumocystis PCR and blood beta glucan improved the diagnosis of Pneumocystis pneumonia in cancer patients. These two tests complement each other — PCR is highly specific, but it may be too sensitive; a high value on beta glucan can help distinguish between colonization and true infection.
- Beta glucan is frequently elevated after abdominal surgery. Another study underscoring the basic problem with this test — if it’s ordered in the wrong context, there are innumerable false positives.
- Fusobacterium necrophorum is often implicated in recurrent peritonsillar abscess. This anaerobic gram-negative infection is more famously known for causing septic jugular vein thrombosis (Lemierre’s syndrome), but it clearly has a role in other suppurative complications. Question: Would a throat swab diagnostic test for F. necrophorum help identify the non-strep pharyngitis cases that would benefit from antibiotics?
- Cefiderocol versus imipenem for (what else?) complicated UTI — and cefiderocol comes out the winner. The winner, that is, based on microbiologic response. As a reminder, cefiderocol is a “siderophore” antibiotic (you can read here what this means), with activity against multi-drug resistant Pseudomonas, Stenotrophomonas, and Acinetobacter spp. Looking forward to seeing the studies in more difficult to treat patient populations, such as hospital-acquired pneumonia.
- Here’s a simple framework to guide antibiotic prescribing: 1) Is infection one that needs an antibiotic? 2) Have cultures or other studies been sent? 3) What empiric treatment should be started? 4) How should results alter therapy? 5) What duration is required? ID clinicians have internalized these thoughts, but no harm making them explicit.
- A woman acquired HIV that was highly resistant to all available integrase inhibitors. Transmission of integrase inhibitor resistant virus is very rare; these viruses have typically still retained susceptibility to dolutegravir and bictegravir. Not this one — the baseline isolate had three major integrase mutations, E138A, G140S, and Q148H. The critical information from the case report was the identification of the source patient, for whom the authors obtained detailed resistance information.
- For ID specialists, management of Staph aureus bacteremia is all over the map. Treatment of choice, management of persistent bacteremia, duration of therapy — plenty of variation! Example: For MSSA endocarditis, 32% chose cefazolin, 29% favored nafcillin, while 32% considered the two the same. Practice variation can represent differences in quality, but here I think they reflect lack of a clear, evidenced-based choice.
- For infected burn wounds, bacteriophages did worse than standard of care in reducing Pseudomonas aeruginosa bacterial burden. This approach to treating resistant infections is highly promising, but still in its infancy.
- Three patients suffered wound infections from Lonepinella koalarum after koala bear bites. No, I’ve never heard of that bug either — which, given the source, will never become a global threat — but the molecular investigation into these cases is quite the tour de force.
Have you written 2018 on a form or check yet?
Of course you have. Happy New Year!
And just 18 million views for this video (and counting):
January 2nd, 2019
How Did Our Medical Notes Become So Useless?
Among the many complaints about electronic medical records (EMRs), the death of the useful medical note ranks very high.
Notes are too long, too complex, and filled with unhelpful words. It’s often impossible to glean what the clinician thinks is going on, or what’s planned.
Ever get a note from an urgent care clinic on a patient who went there with a viral syndrome? Or a discharge summary? The note contains pages of indecipherable gobbledygook, ICD10 codes, irrelevant review of systems, stock phrases — the medical words are there, but where is the content? Give a click on this note for a particularly egregious example (all identifying information removed). Then come on back here. I’ll wait.*
(*Good chance these notes are faxed to your office, then scanned into your EMR’s “media manager,” or whatever your EMR calls it. My wife, a primary care pediatrician, calls this part of the EMR “the place where information goes to die.” Yep.)
It hasn’t always been this way. I’ve worked with EMRs of various sorts for decades. One of them, designed for outpatient care, had two ways to file notes — the clinician either dictated a narrative (for complex cases) or, more often, wrote a brief handwritten note in a 3-line section that was immediately typed in by clerical staff.
Both types of notes were infinitely more useful than today’s behemoths. The long dictated notes told a logical story, the short ones highlighted only the most relevant information. Example of the latter:
New painful rash on back. PE: vesicles in T10 dermatome on L, otherwise neg. Dx zoster, Rx Valacylovir 1 gm TID for 7d. Discussed possible complications, reasons to return or call for f/u.
That’s it! Today, this would be unimaginable. In a paper published in the Annals of Internal Medicine, three experts in EMR optimization compared the length of notes in the USA vs other countries:
In other countries, [a note] tends to be far briefer, containing only essential clinical information; it omits much of the compliance and reimbursement documentation that commonly bloats the American clinical note. In fact, across this same EHR, clinical notes in the United States are nearly 4 times longer on average than those in other countries
So how did we get here? What caused the note to shift from being the primary means of communicating medical information to this gargantuan beast? Three primary reasons:
1. Money. Some might call this “billing” or “regulatory” or “compliance,” but let’s call it by its root source — money. Based on quirks of our strange American healthcare system, certain words or phrases or diagnoses yield higher reimbursement than others. This hierarchy has nothing to do with delivering good patient care or communicating with other clinicians.
It’s not just individual words — entire sections of notes owe their very existence to maximizing revenue from clinical services. Dr. Mark Reid, author of the entertaining Medical Axioms, complained last week about being forced to include certain words in his notes.
He received this painful response from a Cardiology fellow, who recently had his notes reviewed by a “Cardiology Coder”:
I got this message in my epic inbox. As a FIT, it was hard to look at this in any positive way. What can I do to help? pic.twitter.com/7oJ34DOUdF
— Ali A. Azeem (@aliahsanazeem) December 29, 2018
Not only did poor Dr. Azeem include a Review of Systems to satisfy the Insatiable Billing Monster, but someone reviewed his Review of Symptoms to ensure he used the correct words! Could there be a better example of what’s wrong with medical documentation than this anecdote?*
(*And could you imagine having that reviewer’s job? Shudder.)
2. Copy/paste. Some EMRs have a feature where you can highlight only the original — not the copied or imported — content of a note. If you do this, you instantly understand why “ID consulted, awaiting input” appears several days after you’ve done your consult and have been communicating regularly with the primary team. They’re not ignoring your beautiful consult, they just haven’t gone back to update the text.
Other symptoms of copy/paste madness are the gobs of laboratory and radiology data appearing in every note, copied from the actual reports and then pasted into the “Results” section, or imported via macros (see #3 below).
How bad is the copy/paste phenomenon in medical documentation? Researchers at UCSF reviewed the source of text from medical notes over an 8-month period, and their findings were not pretty:
We analyzed 23, 630 notes written by 460 clinicians. In a typical note, 18% of the text was manually entered; 46%, copied; and 36%, imported.
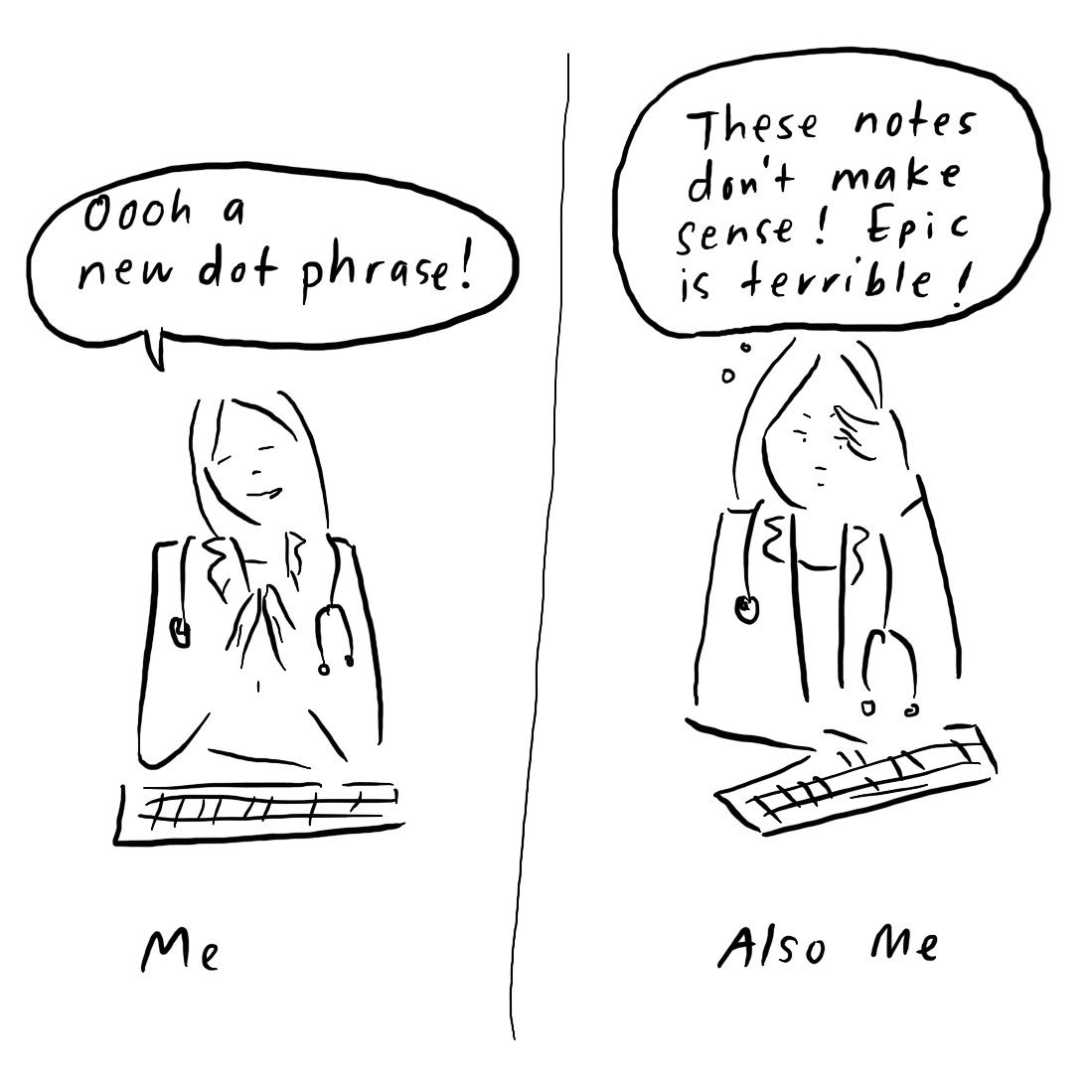
3. Text expanders. Call them what you like — “smart text” or “auto text” or “templates” or “dot phrases” — but these tricks of the trade, once mastered, are simply irresistible to most of us, for better or worse. Dr. Grace Farris captures our ambivalent relationship with this strategy perfectly in the cartoon that led off this post.
It works like this — we enter a magic little short string of characters, press return, and voila! Everything from a complex (but commonly used) sentence to a full medical note appears on the screen. Take a bow and admire your work!
From a Reddit thread on this strategy:
.NICU: As a peds resident, I made this dot phrase. Took me about 2 full days of work to get it together, but I basically created it to pull all the info I needed to preround on a patient. All the numbers from all systems, weight change, ecmo/ventilator settings, even the number of desaturations they had overnight. Approximately 6-8 pages worth of data, arranged in order of systems that we would present on rounds.
Impressive! But do we clinicians really learn, or interpret, material that “autopopulates” a note? And how can these one-size-fits-all notes apply to the infinite diversity of patient care?
Full disclosure: After once receiving feedback that my notes didn’t have sufficient documentation about the time spent on counseling and patient education, how did I respond? By creating “.saxcounsel”, of course — which when typed, expanded into a thorough description of time spent on counseling and patient education! That will show them!
So is there any hope for the medical note?
I do think there is a way to improve them, at least a bit, that won’t require a complete overhaul of billing regulations — but that will be a topic for a different post. In the meantime, I very much welcome your suggestions in the comments!