An ongoing dialogue on HIV/AIDS, infectious diseases,
August 22nd, 2025
On the Internet, Nobody Read My First Blog
Not the site’s banner, but you get the point. (AI generated.)
In 2007, during the boom in online blogging, and right before the economy crashed, a medical education company contacted me and three other ID doctors to write a blog about HIV. The pitch was irresistible — write something about HIV on a regular basis (they didn’t say what), and we’ll promote it widely. Oh, and you’ll get paid!
The lead from the company certainly conveyed enthusiasm. He made the inevitable “viral” pun (ha ha, we all chuckled politely), and unveiled a clever name. It had “expansion potential,” he said: We’ll start with this one on HIV, but later we could launch one on Oncology, Dermatology, Hirudotherapy*.
(*Leech therapy — so not really that.)
He also mentioned how much interest he’d already received from the various companies that developed HIV treatments. Indeed, they planned to sell ads once the internet traffic came pouring in. It was all very promising.
I enthusiastically signed up. Then I wrote a few pieces, none of them in hindsight very good, and sent them to the person responsible for posting them online.
It launched in the spring of 2007, including an inaugural piece of mine called “Some Non-Scientific Thoughts on CROI” where I complained about CROI holding its opening night during the Academy Awards — in Los Angeles, no less. (Yes, they did that.)
Then I waited for the flood of insightful comments. You know, Web 2.0.
The response?
It got worse from there. Reader engagement went from sparse to nonexistent. The site was glitchy, forcing people to reset their passwords for no apparent reason. You can only clear your browser cache so many times before bolting. Even in 2007, patience for that kind of frustration was in short supply.
And the design of the site? It typified the overall look of the early-ish internet — low resolution, bad colors, possibly done with an open-access graphics program by someone’s 8th grader. You want pop-up windows? We’ve got pop-up windows!
The combination of sporadic content and technical obstacles hardly created the kind of user experience to encourage participation. The site closed up shop in less than a year, a much less famous failure than Lehman Brothers, which shared a similar fate and termination date.
But despite the false start, I’m grateful to the organizers for their optimism and for getting me going — you have to start somewhere. That was the lesson I learned in hindsight. It won’t always be a success, but it’s worth putting the words on the page, even if you later cringe at the whole effort.
That’s true for any creative pursuit — painting, music, pottery, bonsai tree cultivation. False starts are still starts, cringeworthy though they may be.
Most importantly, when the NEJM Journal Watch editor Matt O’Rourke considered expanding the Journal Watch content to include blogs, I had some experience with the medium, and could send him some of my posts — now revised, reworked, and improved, of course!
(Revision is an amazing thing. Another lesson learned.)
Would I have been able to launch this effort without that initial experience? Unlikely.
And as a reminder that even the most enduring internet creations start somewhere, here’s Peter Steiner talking about his own legendary contribution to world humor — the brilliant, timeless cartoon “On the Internet, nobody knows you’re a dog.”
It started just another sketch in a pile of many, and was hardly his first try.
August 16th, 2025
Anal Cancer Screening in HIV: When Guidelines Get Ahead of the Evidence
 Should every person with HIV over age 35 (if MSM or transgender woman) or 45 (everyone else) have an anal Pap smear, a digital anal rectal exam (DARE), and possibly a high-resolution anoscopy every 1–2 years? According to recent guidelines, yes. But here’s the problem: we don’t know if this screening effort actually prevents cancer.
Should every person with HIV over age 35 (if MSM or transgender woman) or 45 (everyone else) have an anal Pap smear, a digital anal rectal exam (DARE), and possibly a high-resolution anoscopy every 1–2 years? According to recent guidelines, yes. But here’s the problem: we don’t know if this screening effort actually prevents cancer.
First, some facts:
- Human papillomavirus (HPV) infection is necessary, but not sufficient, for the development of anal cancer.
- Both HPV prevalence and anal cancer incidence are higher in PWH than in those without HIV.
- The natural history of HPV leading to anal cancer is similar to cervical cancer.
- Cervical cancer screening programs have reduced incidence of that disease.
- In the ANCHOR trial, treatment of biopsy-confirmed, high-grade squamous intraepithelial lesions (HSIL) in PWH reduced the risk of anal cancer.
So far, so good.
The temptation, therefore, is to apply our cervical-cancer-prevention model directly to anal cancer, and that’s an approach many have advocated for years. But here’s the problem — there’s no proof this works. As Dr. Hayden Andrews wrote in a recent State-of-the-Art review in Clinical Infectious Diseases (Note: I am currently editor-in-chief of this journal):
To date, no trial has been conducted to determine if anal cancer screening among PWH decreases anal cancer incidence.
And if you think about it for a nanosecond, that’s not surprising! Demonstrating that cancer screening improves outcomes is notoriously hard. Just ask anyone who studies breast, prostate, lung, or colorectal screening — and those cancers are far more common than anal cancer, and have been far more widely studied.
This gets to the core of why I believe the International Anal Neoplasia Society guidelines — later reinforced by the Department of Health and Human Services HIV guidelines — are premature and overly aggressive. They’re posted in our clinic workroom, so I’m constantly reminded of just how broad they are. The recommendations show up in this Bluesky post of mine, along with my incredulous query:
Calling all HIV/ID providers: How many are able to do this screening for anal cancer according to IANS? Including the HRA and repeat screening every 1-2 years (!!) for normal results? Wow, that's a lot of screening tests in a lot of people! #IDSky #HIVsky onlinelibrary.wiley.com/doi/10.1002/…
— Paul Sax (@paulsaxmd.bsky.social) 2025-08-15T17:39:22.614Z
Wow (again) — all MSM and transgender women older than 35? All men and women older than 45? Referral of all abnormal results to high-resolution anoscopy? Then repeat the process if normal results every 1-2 years? My goodness.
Some issues that make broad screening problematic:
- Poor test performance: Anal cytology via Pap smears has low sensitivity for HSIL even in high-prevalence populations; it also has high interobserver variability and lots of unsatisfactory or ASCUS results. Read Dr. Amit Achhra’s paper describing their experience at Yale — disappointing, both in terms of accuracy of anal cytology and patient participation! Digital anal rectal exams (DARE) can pick up anal cancer, but lack sensitivity for HSIL, the key precancerous lesions.
- Limited access to the best test: High-resolution anoscopy (HRA) is superior to anal cytology, but many clinical sites have few or even no trained providers to do the exams. I know of one site that cares for thousands of patients and has zero access to HRA.
- Patient burden: Local anaesthesia, discomfort, repeat visits, cost, and anxiety aren’t trivial.
- Unclear screening frequency: The evidence for how often to screen is even weaker than whether we should screen at all.
Add to this the medicolegal bind these guidelines create — if you follow them, you may overwhelm your local system or excessively burden your patients; if you don’t, you risk looking negligent in hindsight. It’s the perfect recipe for a frustrated group of HIV providers, as we’re doomed to fail (and we obsessive ID types hate failing). I really do wonder what fraction of us are in “compliance” with these guidelines. I’d bet good money it’s very low!
As the late David Sackett, one of the founders of evidenced-based medicine, once wrote, “the fundamental promise we make when we actively solicit individuals and exhort them to accept preventive interventions must be that, on average, they will be the better for it… Without evidence from positive randomized trials … we cannot justify soliciting the well to accept any personal health intervention.”
That’s exactly the unease many of us feel with these guidelines (and thanks to Amit for pointing me to this great quote).
I shared my concerns with Dr. Grant Ellsworth, a member of the DHHS guidelines committee who heads the HPV section, and obviously knows a lot more about this field than I do. In addition to looking forward to a time when HPV testing is routinely incorporated to reduce over-screening, he made some additional valuable comments:
Amit Achhra’s paper really highlights how poor a screening tool cytology can be. They had high unsatisfactory rates and frankly outlying poor performance — even at a place like Yale. If Yale can’t pull it off, who can? My other hesitation with the current recommendations is that I’m not sure ANCHOR’s results can be reproduced in the real world. The study sites had an onerous and expensive training process, with ongoing audits to maintain quality. Sure, we can screen for anal HSIL, but will your clinic be able to find and treat it at the same level as ANCHOR?
That last question is key — if the idealized trial environment can’t be replicated in everyday practice, then the guidelines risk being aspirational rather than accomplishing their goal.
Here’s what I’d do until we have better evidence.
- State up front that although we know that anal cancer is more common in people with HIV, we don’t know if screening helps reduce the risk over a strategy of not screening.
- Start discussions at age 50 (or younger if other strong risk factors: low nadir CD4, smoking).
- Offer shared decision-making, not automatic screening. What does the patient want? We do this with the PSA, why not this test?
- Skip the anal Pap entirely, and go directly to HRA for those who choose screening. If HRA isn’t available, focus on HPV testing.
- Repeat no more often than every 3-5 years, or some other interval to be determined by baseline risk.
This approach acknowledges that the ANCHOR trial answered only one question — whether treating HSIL reduces cancer incidence. It emphatically did not address the important questions of how to screen, whom to screen, and how often to do it.
I’m afraid answers will only come from further clinical studies.
August 6th, 2025
Does the Fact That AI Is Brilliant at Writing “Learning Objectives” Prove They’re Not Really Needed?
Paramount Pictures, 1932.
Recently, I was invited to speak at a primary care conference on a terrific topic: “Can’t Miss Diagnoses in ID for the PCP.”
Love it. So many great examples come to mind — endocarditis, Lemierre syndrome, vertebral osteomyelitis, acute HIV. A wonderful opportunity to teach about the “rare but there” diagnoses hidden among everyday outpatient complaints: fatigue, sore throat, back pain, and “mono,” respectively.
I was all in.
You know what I wasn’t all in on? The inevitable mountain of paperwork that followed. Veterans of academic medicine know what’s coming: the dreaded email with five attachments, multiple forms, and of course — the request for Learning Objectives.
First, let me remind everyone of the Universal Rule of Email Avoidance:
The likelihood of an email being answered promptly is inversely proportional to the square of the number of attachments.
Now, back to the Learning Objectives, which will occupy the remainder of this post. They’re short statements (usually three, range 2–5) that describe what the audience is supposed to learn from a lecture. Education experts say they help focus the talk and make evaluation easier. Accrediting bodies like ACCME require them for Continuing Medical Education (CME) credit. (Mea culpa: This is true even for our course, ID in Primary Care, despite this rant to follow. Sorry.) Hence their ubiquity, and the fact that every talk now asks for them.
Some excellent educators defend them as a helpful way to structure a talk. Fair enough; if they work for you, terrific. And there are numerous authorities in both written and video form on how to write effective Learning Objectives, so you can study up to your heart’s content.
(Go ahead, watch one of those videos in its entirety. I dare you. To me, they are mind-numbingly boring — but to each their own, I guess.)
But let’s not pretend Learning Objectives are an essential part of effective teaching. So much of what will be conveyed in a talk can be communicated in the talk’s title, plus (if requested) a 2–3 sentence summary. And that process of using learning objectives to organize a talk? We used to call that “making an outline.” No pre-talk submission required, no adhering to SMART criteria — which stands for “specific, measurable, achievable, relevant, and timebound,” in case you were wondering.
Fortunately, there’s now a solution: Artificial Intelligence — which has gotten so good at writing Learning Objectives that the task is now completely frictionless. I guess this is no surprise, as even in the stone age of AI (like, last year), it was great at streamlining workplace drudgery.
Here’s the prompt:
“Write 3 learning objectives for a talk called ‘Can’t Miss Diagnoses in ID for the Primary Care Provider.’”
Now watch the magic, example #1 from ChatGPT:
At the end of this presentation, learners will be able to:
Identify key clinical features of uncommon but serious infectious diseases that may initially present with nonspecific symptoms in primary care settings.
Apply diagnostic reasoning to distinguish these conditions from more common, benign illnesses through targeted history, physical examination, and appropriate use of laboratory and imaging studies.
Initiate timely management and specialist referral when these high-stakes infections are suspected, to reduce morbidity and improve patient outcomes.
Bravo. These are far better than anything I could have done, mostly because my Learning Objectives are always written with a combination of mild annoyance and the driving motivation not to let “perfect” be the enemy of “just get it done already.”
Didn’t like these ChatGPT products? Go ahead and try Gemini. Or CoPilot.
Voilà! Problem solved. These are so good, it’s downright scary. No thinking required. Copy, paste, submit. Or just send the organizers a link or generate a QR code for handy scanning.
But here’s the problem: if AI can generate them instantly — without context or understanding or board certification in Infectious Diseases — what are Learning Objectives really worth? How many people actually read them? At the end of a talk, no one says, “Wow, those Learning Objectives were beautifully met.”
Instead, we say:
Was that a good talk? Did I learn something useful? Was I engaged? Or was I bored out of my mind, checking my phone?
So I’m sticking with the view that it’s hardly ever about the Learning Objectives. Let’s stop pretending otherwise.
And a plea to the leaders of medical education: could you please — please — lighten the paperwork load for clinical teachers? That would be hugely appreciated.
Let’s close with a scene that proves exasperation with institutional nonsense in education is timeless. These guys had it pegged nearly a century ago.
August 2nd, 2025
The Short Political Half-life of a Medical Contrarian
 In early May, I wrote about the surprising FDA appointment of Dr. Vinay Prasad to lead the FDA’s Center for Biologics Evaluation and Research. Prasad is a UCSF hematologist-oncologist known for his views on COVID-19, oncology clinical trials, and his sometimes sharp-elbowed communication style, in particular directed at people with whom he disagrees. My goal was to write something balanced, and even hopeful, acknowledging both Prasad’s impressive skills in interpreting medical evidence and his well-documented provocations, at least as viewed from the perspective of an ID doctor.
In early May, I wrote about the surprising FDA appointment of Dr. Vinay Prasad to lead the FDA’s Center for Biologics Evaluation and Research. Prasad is a UCSF hematologist-oncologist known for his views on COVID-19, oncology clinical trials, and his sometimes sharp-elbowed communication style, in particular directed at people with whom he disagrees. My goal was to write something balanced, and even hopeful, acknowledging both Prasad’s impressive skills in interpreting medical evidence and his well-documented provocations, at least as viewed from the perspective of an ID doctor.
Let’s just say: not everyone loved that piece.
I wrapped up that post with this:
Ultimately, my deepest hope — and I suspect everyone’s — is that this appointment of Dr. Vinay Prasad leads to a continued focus on improving the safety, efficacy, and public trust in biologics, especially vaccines. We need rigorous science, honest communication, and thoughtful leadership more than ever.
That doesn’t sound too bad, does it? The comments I received here on this site were quite thoughtful, led by Dr. Jonathan Blum’s clever “I am cautiously pessimistic” — ha! I also got a nice note from Dr. Adam Cifu, who is a friend of Prasad’s and co-founded the interesting Sensible Medicine newsletter with him.
But, judging by some of the responses I received by email or on social media, you’d have thought I’d volunteered to ghostwrite for RFK Jr. For those who think Bluesky is the kinder, gentler social media platform, allowing only polite and balanced responses — I have some strong evidence to the contrary. Yeesh. Turns out anonymous burner accounts are nasty no matter where they post.
Now, not even 3 months later, Prasad is out. Officially, he resigned — the classic “time with family” explanation. Unofficially? He’s gone because he did what we say we want FDA leaders to do: he questioned the approval of an expensive, potentially toxic therapy with scant evidence of benefit.
And no, this wasn’t about COVID-19. Or vaccines. Or even infectious diseases.
It was about a treatment for Duchenne muscular dystrophy — a tragic and incurable disease that understandably generates passionate advocacy and whose therapies have a long track record of FDA controversy.
But after a Wall Street Journal op-ed from a non-physician critic and some well-placed accusations of political disloyalty (apparently, he’s too much of a Bernie guy now?), he’s gone. Just like that.
This raises a disheartening possibility: that both his appointment and his dismissal had less to do with his ability to interpret clinical studies and more to do with politics, all while mixing in an unhealthy tincture of conflict of interest.
That’s deeply unfortunate — because whether you loved or loathed Prasad’s presence at the FDA, one thing is clear: science-based public health leadership shouldn’t be a partisan tug-of-war. Not when trust in our institutions is already on shaky ground.
I’d like to give the last word to one of my long-term mentors, a now-retired ID doctor who held some important government positions during his distinguished career. He’s been watching this turn of events with detached amusement from his summer home, and wrote me this sage comment in a terse email:
It’s a lot easier throwing bombs at others from the outside than taking criticism coming in.
Isn’t that the truth?
And speaking of sharp thinkers who challenged conventional wisdom, and because last week I finished with a tribute to some recent celebrities who died, this past week we lost satirist-mathematician Tom Lehrer at age 97. His songs were a master class in wit, skepticism, and brainy mischief — all qualities that (whether you like him or not) Prasad might admire.
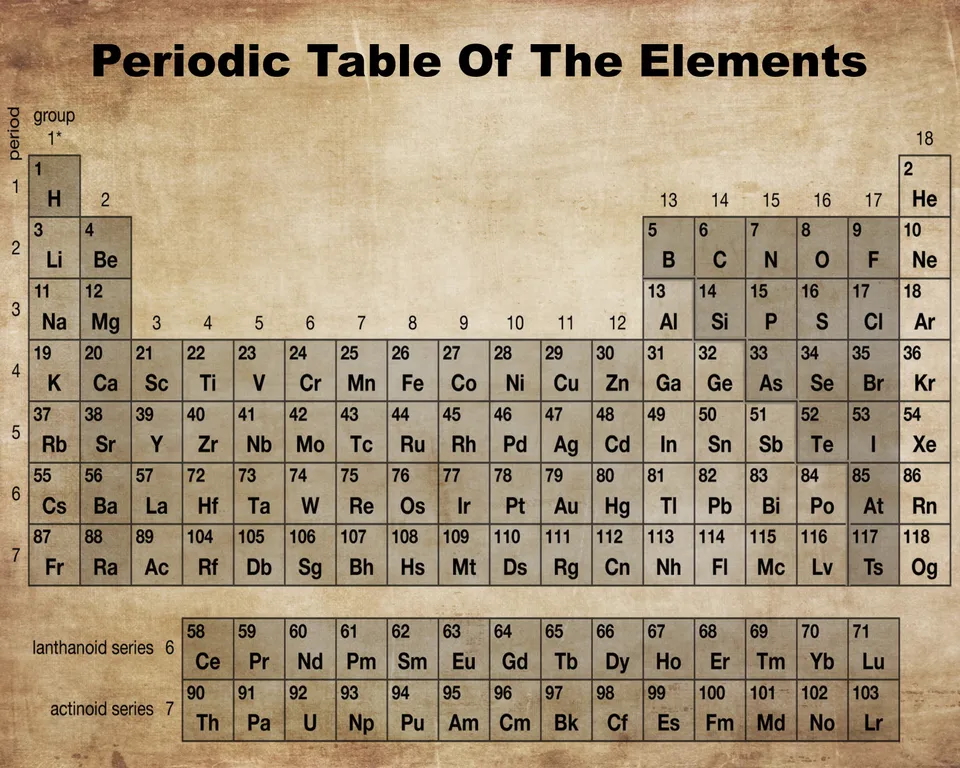
Lehrer’s work also brings back fond memories of the smartest kid in my school, my friend Jimmy P, who introduced me to these nerdy musical gems. (I was an 8.5/10 on the nerd scale; Jimmy easily 10/10.) If you’ve never seen it — or just want to be reminded how funny chemistry can be in the right context — here’s one of the all-time classics:
What a talent — even rivals Ozzy Osbourne.
July 25th, 2025
Who Gets Sent to ID Clinic? A Field Guide to Outpatient Referrals
 Sometimes people ask me what kind of cases get referred to ID doctors in the outpatient setting. Despite what the latest television series might suggest, it’s rarely suspected Ebola (fortunately) or Tsutsugamushi fever — a disease that is much more fun to say by its Japanese name than its common one, scrub typhus.
Sometimes people ask me what kind of cases get referred to ID doctors in the outpatient setting. Despite what the latest television series might suggest, it’s rarely suspected Ebola (fortunately) or Tsutsugamushi fever — a disease that is much more fun to say by its Japanese name than its common one, scrub typhus.
(In Japanese, “tsutsuga” means “hindrance” or “illness,” and “mushi” means “insect” or “vermin”. Now you know!)
Instead, the cases generally fall into one of these four broad categories:
1. Diagnostic dilemmas. The clinical gestalt suggests infection, there’s no diagnosis, and the patient isn’t getting better. You know, Box #4 of the Four States of Clinical Medicine — “No diagnosis, not improving,” the most unstable box to be in. Let’s see if our diagnostic skills can get the patient out of that box as fast as possible.
Fever of unknown origin is the classic example, but it could be a red limb unresponsive to empiric antibiotics, refractory diarrhea, disabling night sweats, or the cough that just won’t go away.
A somewhat different version of these dilemma cases (but still in this category) is the patient reporting extensive infectious exposure, and now new symptoms that could be related. If a construction worker has just returned from an excavation project in Tucson, where he oversaw trenching and grading operations (or whatever excavators do), you’d think of a certain fungal infection if he now showed up with a cough and low grade fever. Or it could just be a viral upper respiratory infection.
Closer to home, infection would be top of the list if a restaurant worker from a New England seafood restaurant had slowly growing nodular red bumps up her arm. Fun fact: the person most likely to have M. marinum isn’t your friend with the aquarium — it’s the sous chef cleaning lobsters with a Band-Aid on a scraped knuckle.
Sometimes it’s just profound fatigue after an infection — in ID, we were seeing post-infectious fatigue long before COVID-19 (after sepsis, Epstein-Barr virus, cytomegalovirus, influenza, lyme), and COVID has certainly increased that pool of unfortunate patients. Yes, many of these referrals turn out not to be active infections, or infection-related, at all — but that’s for us to figure out. We’re the “it might be an infection” people.
2. Unusual diagnoses to nonspecialists. These are infections that primary care clinicians might see only occasionally, but that land in our inboxes daily. HIV, osteomyelitis, endocarditis, tuberculosis, nontuberculous mycobacteria, prosthetic joint and other hardware infections, multi-drug resistant bacterial infections, and the full spectrum of syphilis. (Examples of this last one: secondary syphilis with uveitis, or tinnitus, or some other bizarre manifestation of this quintessentially protean disease.) Hepatitis C used to fall into this category, especially in the interferon and early direct-acting antiviral era, but now treatment has become so simple that most patients get treated (and cured!) in primary care. Still amazed at that transformation.
Vertebral osteomyelitis is a striking example of this category — rare to primary care, common to us. A busy first-year ID fellow may see more than a dozen of cases over the year on the inpatient consult service, whereas a primary care clinician will evaluate hundreds of patients with back pain over several years. But chances are good that none of them has vertebral osteomyelitis.
Not surprisingly, many of these patients are diagnosed during a hospital stay. Since most generalists today focus on either inpatient or outpatient care (not both), we often inherit these cases post-discharge after an inpatient consult.
3. Unusual diagnoses — even to us! These are the real fascinomas, the ones that earn a coveted slot in ID case conferences and elicit audible gasps, especially if there are good images.
Here in temperate Boston, parasitic infections and tropical diseases make the list, as do systemic fungi, nocardia (which straddles the line between fungus and bacterium — I hope that’s not insulting to nocardia), and various other medical oddities. Infections that were once common but are now mostly vanquished also show up, and here’s when having gray hair as a “seasoned” clinician (I wonder who that could be) is a plus. One recent example is a referral we received for a fever and an unusual pustular rash that turned out to be … varicella … better known as chickenpox.
But for many of these true rarities (not chickenpox, but rather melioidosis or leishmaniasis or cysticercosis, et al.), there are usually only a handful of true experts, and we ID doctors often act as the conduits to them. Luckily, they’re often generous with their time when we call or email. Thank you, remote consult heroes!
4. Very common diagnoses — but with a twist. Finally, the largest category. These are the bread-and-butter infections that just won’t go away, or keep coming back, or are sometimes particularly severe. Recurrent cellulitis, sometimes complicated by bacteremia and requiring hospitalization. Chronic sinusitis. Nonhealing wound infections. And leading the pack by a wide margin: urinary tract infections (UTIs).
UTIs may never make the headlines in medical mystery columns, but what they lack in novelty they more than make up for in frequency — and in misery, for the frustrated patients who suffer through them. Challenging UTIs are so common in ID clinic that we really ought to start a loyalty program. Fortunately, two of my colleagues — Drs. Sigal Yawetz and Jacob Lazarus — specialize in these cases and generously share their expertise with the rest of us.
If you’re looking for guidance on managing UTIs, you’re in luck: two outstanding new publications have just come out to help clinicians navigate both recurrent and complicated cases:
- A State-of-the-Art review on Recurrent Uncomplicated UTIs in Women, published in Clinical Infectious Diseases.
- A comprehensive IDSA Guideline on Complicated UTIs, which includes my colleague Sigal on the panel.
Each comes with practical tools, evidence-based recommendations, and at least one flowchart you’ll find yourself referring to again and again — whether you’re in clinic or on the wards.
Wow, quite the week for deaths of some notable celebrities from my youth and young adulthood — Ozzy Osbourne, Hulk Hogan, Chuck Mangione, Malcolm Jamal Warner (particularly sad, given his age). I can’t say any of them was a particular favorite, though of course I knew of them all, with Chuck Mangione’s “Feels So Good” playing on perpetual repeat during my senior year of high school.
Who to feature here at the end of this ID blog? I’m going to go with Ozzy, in honor of the self-awareness he developed later in life (especially on the reality TV show he did with his very appealing wife Sharon), and as a gift to my mother, who turns 91 today. She loved his music.
That, my dear readers, is sarcasm. Happy birthday, Mom!
July 17th, 2025
Ceftriaxone Is a Narrow Antibiotic Now — and Other Musings
Mather and Company, 1929.
In no particular order, 20 things I’ve found interesting lately — a mix of ID (mostly), language quirks, clinical stuff, even tennis, and an apology (#21) at the very end. Bonus videos embedded because we all need a break.
1. Isn’t it amazing how, over time, an antibiotic once considered “broad spectrum” later becomes the drug we use after the term “narrowed?” Example: “He was on meropenem, but his cultures came back with just Strep mitis, so we narrowed him to ceftriaxone.” Fair enough — it’s narrower than meropenem — but it’s crazy that ceftriaxone is now a “narrow” antibiotic!
2. Someone who has scant knowledge about healthcare — but has nonetheless risen to a position of power and influence — said that “50 percent of revenues to most pediatricians come from vaccines.” What the …? You might as well say that they get the other 50% by charging for the stickers they hand out at the end of the visit. In fact, pediatric practices take on financial risk and incur high up-front expenses to have vaccines available; for some, providing and administering vaccines can lose money.
3. On the topic of pediatrics, childhood hospitalizations last year from mycoplasma did indeed sharply increase, accounting for half of hospitalized children with pneumonia. We also saw way many more cases in adults, including many with those strange non-respiratory presentations (rashes, neurologic disorders, hemolysis). While cyclic variations in mycoplasma incidence are expected due to waning immunity, this past year saw a bigger increase than usual.
4. I’m not gonna lie — it has always amused me that many people (including me!) highlight certain comments with, “To be perfectly honest…” What does this imply about when we don’t say this? That we’re not being honest? And yes, “I’m not gonna lie,” “truth be told,” “truthfully,” and the rest of the bunch all fall into the same category.
5. A patient I’ve been following for years had a CD4 nadir of 3 at the time of their HIV diagnosis in 2010; it’s now over 2000, an astounding increase. Meanwhile, a similar patient I saw recently has had virologic suppression for almost as long, and the absolute CD4 count still can’t quite crack 100. This variation in immune response to antiretroviral therapy is one of the unsolved mysteries in HIV medicine.
6. Learned recently that pair of words that is used in a fixed order in an idiomatic expression is called an “irreversible binomial.” You know — wet and wild, mac and cheese, wear and tear, rock and roll. The first ID one that came to mind? Glucan and galactomannan — fungal diagnostics aficionados will agree, no one says it the other way
7. The continued universal susceptibility of Treponema pallidum and group A strep to penicillin remains a great gift to humankind, one we should be grateful for every day.
8. We complain about electronic medical records a bunch, but let’s face it — they have made a whole lot of things better than back in the pre-digital age. Near the top of the list? The ability to review radiographic studies without having to trek to a reading room, where the films may or may not be available. It’s especially great since we can now use Teams or Zoom to review the images with our radiologists, with them highlighting the areas of greatest interest.
9. How does anyone ever learn English?
10. We’ve had BCID (Blood Culture Identification) testing in place for around a year now; it rapidly identifies the bacteria in positive blood cultures, and tests for genetic determinants of common resistance mechanisms, too. Trust me — once you have this in place, you can’t imagine ever going back.
11. Even a year after my rant, and over a decade since generic tablets hit the market, some clinicians still think linezolid is too expensive. That’s because patients go to pharmacies, get told their insurance won’t cover it, and aren’t told they can just pay out-of-pocket at a reasonable price. Even worse, one large chain still charges a crazy high price, presumably for the branded version. Because they can? It’s madness.
12. I used to pride myself on knowing all of the FDA-approved cephalosporins, including obscure oral formulations. Confessing right here that the blizzard of recently approved and late-stage compounds (most of them cephalosporin-beta lactamase inhibitor combinations) has challenged this party trick. Let’s see — there’s already ceftazidime-avibactam, ceftolozane-tazobactam, cefepime-enmetazobactam, and cefiderocol; coming soon will be cefepime-zidebactam and cefepime-taniborbactam. Wow.
13. By the way, in addition the cephalosporins, I can also name the fluoroquinolones that were withdrawn due to safety issues — temafloxacin, sparfloxacin, gatifloxacin, grepafloxacin, and trovafloxacin. Branded Zagam, Trovan, Raxar, Tequin, they sounded like action figures fighting it out in an animated science fiction movie. Fun times!
14. Which reminds me: A resident recently told me they couldn’t go into ID because it required “too much memorization” — antibiotics and microbiology, specifically. My reply: it’s not like you become an endocrinologist by spontaneously deriving the hormonal feedback loops. Every specialty has its learning curve. Memorization follows interest.
15. Since the topic of party tricks came up (Name that cephalosporin! That discontinued quinolone!), I often find myself watching videos of card tricks with amazement, admiring the talent of people with a large repertoire. This guy, who says he has a million such tricks, is my favorite of many such magicians — something about his very regular-sounding voice makes him tremendously appealing:
16. Since those were Keith Haring playing cards — you noticed, right? — I must cite that IAS 2025, the 13th IAS Conference on HIV Science, happened this week in Kigali, Rwanda. Not surprisingly, there were several presentations on disruptions in patient care resulting from recent policy changes and budget cuts by the USA — disruptions that will lead to more HIV infections and more HIV-related deaths. Sad to see this proud chapter in U.S. foreign policy come to an end.
17. The letters to the editor at NEJM protesting the Sounding Board written by Drs. Vinay Prasad and Martin Makary on vaccines for COVID-19 make fascinating reading, as does Prasad’s and Makary’s response to the correspondence. It’s remarkable how a group of intelligent, experienced, and well-meaning people can look at the same body of evidence in medicine and come up with starkly different interpretations. I think both sides having valid points.
18. Related, what I’d really like to see is Prasad — who is a strong advocate of evidence-based medicine — take aim at some of the quite outlandish statements we’ve heard about the epidemiology and causes of autism, or the perils of seed oils. Hey, why not? He’s never been shy about voicing his opinion in the past.
19. My favorite new phrase mobilized by our ID fellows when coming up with a treatment plan for an ID consult? Course it out. “He’s improved on cefepime day 3 empirically for pneumonia; I think we can course it out with 4 more days and sign off.” Love that phrase — “course it out” — now a part of our service lingo. Plus, 3+4 = 7. Because of course it does.
20. Congratulations to Jannik Sinner, who blitzed his way past Carlos Alcaraz in this year’s Wimbledon final, as well as Iga Świątek, who “bageled” Amanda Anisimova, 6-0, 6-0. But the best single point of the competition? I’d give the nod to old-timer (38!) Novak Djokovic who, on his way to a semifinal finish, pulled this one off in an earlier round:
21. I was hard on Djokovic in the past when the guy refused to get the COVID-19 vaccine, comparing him to a bully athlete from my school days, but he has really grown on me. In my defense, the world was crazy those first 2 years of the pandemic; I wasn’t always so tolerant. Which is why I was delighted to read a piece entitled Novak Djokovic, I Was Wrong About You, as it summarizes my current views on him perfectly.
So my apologies, Novak!
July 12th, 2025
The Patient Did Well — So the Insurance Company Won’t Pay
 Sometimes, you can predict a bad outcome. Examples:
Sometimes, you can predict a bad outcome. Examples:
- Proposing marriage after an awkward first date — and doing so over gas station nachos.
- Moving to a Cambridge apartment with no off-street parking, then buying a Tesla Cybertruck.
- Trying to recruit for ID fellowships from a group of cosmetic dermatologists.
But predicting what happens in clinical medicine? Not so easy. Which is why the clairvoyance expected by certain health insurance companies baffles the mind — they seem to believe we can diagnose, prognosticate, and determine outcomes with the omniscience of the Oracle of Delphi.
Take this recent gem. I’m sharing it here not because it’s unusual, but because the absurdity deserves a moment in the spotlight.
(Part of a series.)
Here’s the scenario (some details changed to protect privacy):
The patient, a 64-year-old man, went to our emergency room with fatigue, acute kidney injury, and a hemoglobin drop. He’d recently undergone gastric sleeve surgery, making the clinical status more uncertain than usual — plus a background of diabetes and high blood pressure as medical comorbidities. Given the symptoms and risk factors, he was admitted to medicine for hydration, monitoring, and endoscopy. He got better. We all celebrated. Cue the credits.
But then… the sequel. (Spoiler alert: It’s a horror film.)
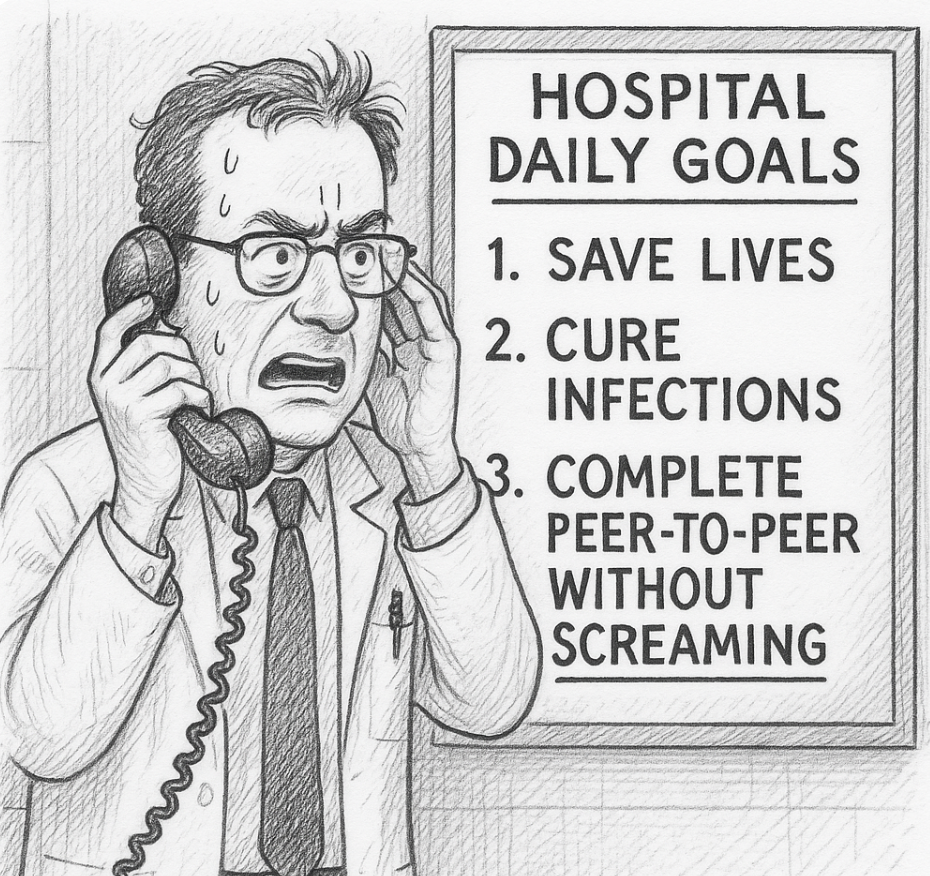
A few days later, I received an email saying that the insurance company had denied inpatient level of care — in plain English, they didn’t want to pay. Would I have time to do a “peer-to-peer” discussion to try and reverse the decision?
They might as well have asked me to call an airline to rebook a cancelled flight during a massive Nor’easter, that’s how much I was looking forward to this task. But given how justified the admission was, and my trying to be a team player to defend good clinical practice in the face of our Private Insurance Overlords, I set up some time to talk with my “peer.”
I use quotation marks because while I’m sure she was, technically, a healthcare professional, her role in this drama felt more like prosecutor than peer.
She had some of the hospital data. Not all. Enough to cherry-pick to support their refusal to pay, but not enough to understand the full context of the case since, of course, she had never seen, spoken with, or evaluated the patient.
She asked me a series of questions, some of which were about information she already possessed, as if hoping I’d contradict myself like a suspect in a police procedural. (“So you’re saying the patient had a drop in his hemoglobin during the hospitalization? Interesting, doctor… very interesting. I see here it remained 7.5–8.3 during his stay. Do you consider that a drop?”)
I explained, again, the patient’s presentation. The drop in hemoglobin from his baseline of 10.5. The post-bariatric surgery. The concerning acute kidney injury in someone with diabetes, hypertension, and obesity. You know — the reasons why he was admitted.
But then came the decision, delivered with the cool finality of a game show host eliminating a contestant. Because the patient had no hemodynamic instability during his stay, and no ongoing bleeding, the hospitalization was deemed… unnecessary.
Denied.
“I cannot overturn the decision,” she said, as if quoting some higher order of evidence from randomized clinical trials rather than a faceless algorithmic edict she no doubt had up on her screen as she was talking with me.
I took a deep breath.
Then I asked her to imagine herself as the patient — sitting in the ER, post-recent surgery, with those symptoms and those lab results. Or better yet, as the clinician doing the initial assessment, deciding whether to admit or to send him home.
Would she have discharged this man? Would her judgment have changed if she weren’t now on the payroll of Giant Healthcare Insurance Company? Had she, like so many burned-out clinicians, left clinical medicine because of pointless, time-wasting demands like this conversation — only to end up perpetuating the same dysfunction from the other side?
No answer. Silence on the other end. Then, she repeated, “Thank you, Dr. Sax for your perspective. I cannot overturn the decision.”
Because of course, the outcome — the good outcome — was only apparent after the fact. One reason to admit people is when we don’t know if they’ll do well.
So yes, the patient got better. No, he was not critically ill. But that’s not evidence the admission was unnecessary; that’s evidence the admission went about as well as could be hoped. Isn’t that what we all want?
Unfortunately, our healthcare system now seems to reward retrospective omniscience more than clinical judgment. “If only you had known he wouldn’t bleed again!” they say. Right. And if only I had known to buy Nvidia stock when it first went public in 1999.
I’ll stop now — time to call my airline because my flight has been canceled due to an unexpected mid-summer blizzard. Should be more fun than this call.
July 7th, 2025
Two Pandemics, Compared: Reflections on HIV and COVID-19
 “Dr. Sax, what’s it like to have lived through two pandemics as an ID doctor?”
“Dr. Sax, what’s it like to have lived through two pandemics as an ID doctor?”
The question came from a brand-new intern during afternoon sign-out. I took a breath — because wow, were they different.
HIV: It Felt Like A Calling, One Miraculously Rewarded
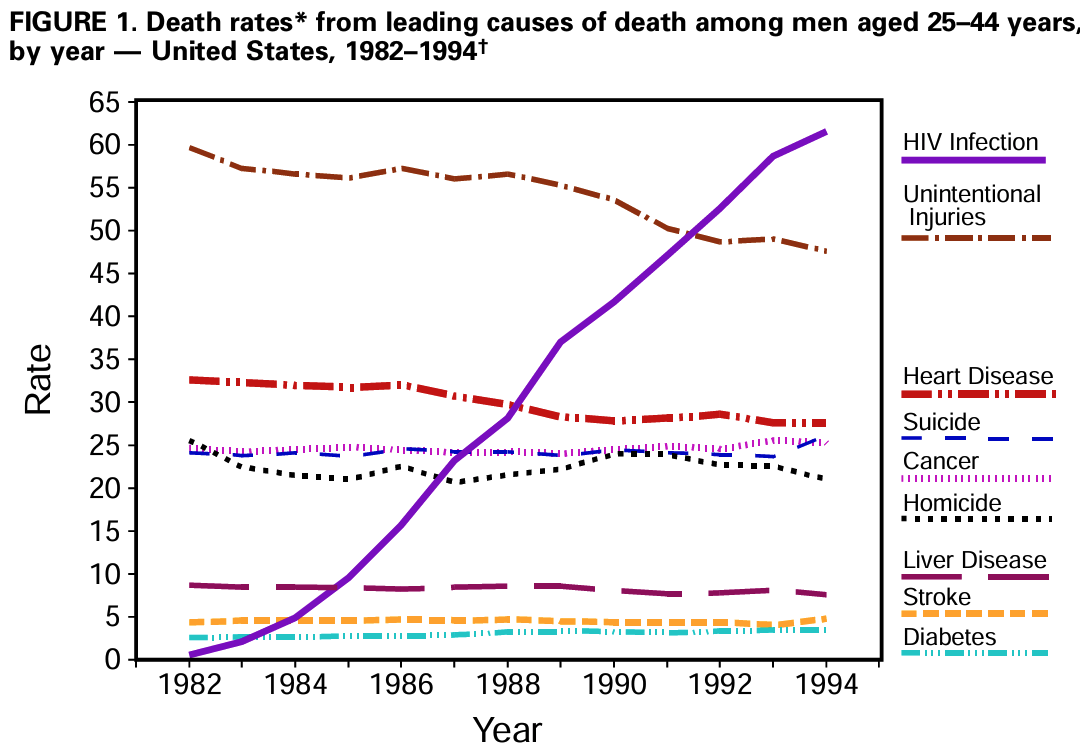
I started my internship in 1987, six years after the first cases of AIDS were reported. The median survival of someone newly diagnosed with AIDS was 12−18 months. When, at the end of my three-year residency, I chose Infectious Diseases as a specialty, part of the rationale was to follow what felt like an urgent mandate: HIV was about to become the leading cause of death among young men in the United States.
(I also liked antibiotics, microbiology, and taking patient histories about travel and pets. You know, the nerdy ID stuff.)
This catastrophic new disease taking the lives of young people in our country didn’t just present a medical challenge. The stigma was brutal. Many clinicians reinforced it by asking how someone acquired the virus, even when the information was in the chart or had no impact on treatment. “How many partners?” “IV drugs?” “Why didn’t you use condoms? I sure hope you do now.” Patients loathed the inquisition and the implied accusations; most of them already felt deeply stigmatized by their diagnosis.
One gastroenterologist, after doing an endoscopy, memorably told a 28-year-old patient of mine with candida esophagitis, “You don’t look like someone who has AIDS. How did you get it?” She remembers that 30 years later, and so do I.
It’s hard to convey just how ubiquitous, and punishing, this stigma was back then. “We can’t have those people taking up an ICU bed,” a cardiologist grumbled to me in 1990. Those people. Some surgeons looked for any excuse to avoid operating on a patient with HIV. Hospitals deliberately downplayed HIV as an area of expertise, not wanting to be branded an “AIDS hospital.”
I’m embarrassed to write that even some ID doctors followed this unfortunate plot line, expressing concern that HIV might ruin our specialty. Why take care of someone with advanced HIV disease when there was nothing that you could do to treat the underlying problem, the virus itself? Send them back to their primary providers for palliative care once you’ve treated the toxoplasmosis or pneumocystis, they argued. Small in number (fortunately), this group of ID doctors did not distinguish themselves during this period.
Because they were wrong. There was plenty we could do, and it wasn’t just diagnosing, treating, and preventing the opportunistic infections. We could also help alleviate chronic symptoms, manage polypharmacy, provide a longitudinal, compassionate care team, and — this part was critical — we could follow closely the research on antiretroviral therapy gathering steam in the laboratories and clinical trials.
When successful HIV treatment arrived in 1996, we could then celebrate with our patients the transformation of their previously fatal disease into something quite treatable. Rejoice!
Today, remarkably, HIV is easier to manage than many chronic conditions. In a quiet signal of triumph over the inevitable downward course of untreated HIV, residents who admit someone with stable HIV to the hospital — usually for a completely unrelated reason — list HIV way down on the patient’s problem list, something in the background that deserves mention but is rock-solid stable.
COVID-19: A 2-Year Siege That Drained and Divided Us
March 2020 reversed that script. Critically, this time, we ID folks weren’t alone; the whole medical center mobilized.
Energy to respond clinically was both collaborative and, at least initially, sustaining. In those first months, we worked together with critical care specialists, emergency room personnel, the microbiology lab, nursing, respiratory therapists — everyone on the front lines of patient care chipped in to get it right.
Another big difference was that, due to the mode of transmission, the fear was everywhere: every PPE donning felt like bomb-squad duty. Is it weak of me to admit that each time I entered the room of a suffering, coughing patient with COVID-19 in the spring of 2020 that my heart rate quickened? That I repeatedly checked my N-95 mask for the proper seal? Cursed with a giant nose, I had always considered this feature of my anatomy a cosmetic challenge, not a life-or-death issue — but it sure made fitting an N-95 mask difficult.
(Too much information? Sorry.)
I remember a woman from the Dominican Republic, struggling with COVID, telling me — through an iPad interpreter — that she drew strength from memories of going to church as a child. Her faith, she said, was helping her fight the virus. I listened, nodding, but from the far side of the room. The connection felt intimate; my posture and location, not so much.
Hallways were eerie and quiet — administrators were remote, many non-essential clinicians sidelined and doing only video visits, all elective surgery canceled, and family and friends of patients barred from visiting their sick loved ones. That last one was particularly heartbreaking. What a terrible time.
Then, the summer of 2020 teased us with a very welcome pause, as COVID practically disappeared from northern cities like Boston. Phew, time for a deep breath, everyone. I remember postulating hopefully, wishfully, to a close friend that perhaps the virus had already targeted the vulnerable, either from immunologic or genetic factors still to be determined; maybe it was done wreaking havoc on society at large.
I was so very wrong. The next 18 months brought us an autumn/winter surge almost as bad as the first one. Delta the following summer filled ICUs with the unvaccinated; Omicron then infected everyone else within weeks, making the Christmas holidays in 2021 a blur.
We in ID watched each of these waves unfold, following the scientific advances closely, and doing our best to communicate this knowledge to our patients and an increasingly weary public who just wanted this virus gone. Monoclonal antibody treatments came and went as the variants mutated — each antibody challenging to obtain with limited supply, and as difficult to deploy as they were to pronounce.
(It will be quite the trivia question one day to ask ID doctors to say, or spell, bamlanivimab, casirivimab, and imdevimab.)
Alas, our hard work put us in growing conflict with a world ready to move on. Anytime we modified our guidance due to evolving evidence as the disease changed, our words were seized as a signal we weren’t to be trusted. Ivermectin enthusiasm and anti-vaccine rhetoric spiraled into mass delusion. Two extremist camps battled it out in the press and social media — the group that insisted the whole thing was a fraud from the start versus those who refused to acknowledge that the disease had lessened in severity over time.
We knew that the truth lay somewhere between these two groups — yes, COVID was still with us, causing some unfortunate people to become severely ill or leading to Long COVID, but no, it was nowhere near the threat it was in the first 2 years. Somehow, conveying this message led to increasingly cantankerous pushback from both camps.
What began with a collaborative spirit to fight a global pandemic evolved into a political fracture that still hasn’t healed. It was the toughest 2 years of my career, and I’m still not over it.
Some Lessons Learned
Back to that intern’s excellent question, because in our workroom, I probably didn’t give it sufficient thought when I answered, motivating this post.
Yes, they were different. There’s no better example of how different than to look at what happened to Dr. Anthony (Tony) Fauci. Celebrated for leading the response to HIV, pilloried for the same leading role with COVID, he eventually needed a security service to protect himself and his family — one of the saddest commentaries on our divided world one could imagine.
But both viruses exposed societal ignorance and healthcare inequities. The best responses involved teamwork, compassion, rigorous evaluation of the latest research, and nuanced communication.
And both reinforced the fact that our work is never boring, that’s for sure. ID is still the best job in medicine, even when it breaks your heart.
June 27th, 2025
The Mystery of the Isolated Hepatitis B Core Antibody, Solved

(A post inspired by years of doing eConsults, an extremely common query about hepatitis B testing, and the latest BritBox series, “Core Antibody Confidential,” starring a grizzled detective with a faded suit and a haunted past.)
Your electronic medical record lists “deficiencies” in health care maintenance for one of your patients, so you order hepatitis B serologies. The next day, the results pop up on your screen (cue ominous base line):
HBsAg: negative
anti-HBs: negative
anti-HBc: positive
The start of the report was simple, but it’s the ending that pushes you to hit the “Next Episode” button.
Why? Because there’s no surface antigen to confirm an active villain. No reassuring surface antibody to declare the battle won. Just the mysterious core antibody, skulking around your labs like one of those brilliant character actors who also appeared in Broadchurch — or was it Shetland, or (changing British TV genres) Bleak House?
Let’s play the eccentric British detective, his career fading and forced to resign from a post in London due to a separate mystery on its own (and a very engaging subplot itself), and now arriving in a remote seaside town to solve this mystery.
- Resolved infection. Your patient cleared HBV long ago; anti-HBs has simply faded with time, like my memory of the names of the minor characters from Episode 1.
- Occult HBV infection. They have chronic hepatitis B, but the surface antigen is too low for detection — hiding in a witness protection program, likely somewhere in the right upper quadrant. Further inquiry with a hepatitis B DNA test (hepatitis B viral load) may snag this guy, but you’ll have to bring the patient back for more questioning … um, blood tests.
- The “window period” of acute infection. The crime just occurred, and the protective surface antibodies haven’t shown up yet, even though the surface antigen cleared. Even detectives on the downslope of their careers can chase down recent risk factors for HBV — and so should you.
- False-positive test. Tests aren’t perfect, and antibodies to hepatitis B core might cross react with other antigens — such as those triggered by eating marmite, haggis, or trifle. (Not a fan of any of these British food items, for the record. And yes, I made those up as the cause. In reality, we rarely know what triggers false positives, but low pre-test probability and imperfect assays are usually to blame.)
Practically, what to do next? And isn’t it time to stop this detective series metaphor?
(Yes. Apologies if I periodically lapse.)
Back to real life. Since by far the most likely explanation for anti-hepatitis B core antibody is resolved infection — item #1 above — the simplest thing to do is check for hepatitis B DNA. In the vast majority of cases, it will come back negative, and you can reassure your patient.
But are you done? Not quite — like any good mystery, a couple of loose threads remain, maybe even enough for Season 2. Importantly, people with isolated anti-HBc positivity may have occult hepatitis B infection (OBI), defined as HBV DNA in the liver with or without detectable HBV DNA in the blood. This becomes clinically relevant in immunosuppressed individuals, organ transplant recipients, and those with HIV or hepatitis C virus coinfection, as they are at increased risk for HBV reactivation and associated complications.
The population at greatest risk for this reactivation? People who receive B-cell depleting therapies such as rituximab, with the risk high enough to warrant antiviral therapy with either entecavir or tenofovir.
Note that this isolated core antibody pattern is particularly common in those with HIV and hepatitis C. Since most of those with HIV are already receiving anti-hepatitis B therapy with tenofovir and/or lamivudine/emtricitabine, reactivation is not a concern unless switching to a NRTI-free regimen — something increasingly done in the era of long-acting cabotegravir-rilpivirine. For those not on NRTIs who have isolated core antibodies to hepatitis B, periodic HBV DNA monitoring may be warranted, and I would certainly do this if the ALT and AST become abnormal.
Before wrapping up this mystery, let’s consider this important unresolved plot line:
Should people with isolated anti-HBc receive the hepatitis B vaccine?
The guidelines say yes, so clinicians who choose to do this certainly are taking a defensible position. There may be institutional or documentation-based reasons to vaccinate — fair enough. And you’d make the guidelines happy.
But in terms of virologic logic? Count me unconvinced. I’d argue that since the primary purpose of the hepatitis B vaccine is to prevent viral acquisition, what’s the point of vaccinating people who have already had hepatitis B?If there were convincing clinical studies demonstrating that those with isolated anti-HBc are at high risk for infection with de novo hepatitis B virus, then I’d be more enthusiastic. But I can’t find any.
Also, as far as I know, there aren’t even studies showing that giving the vaccine reduces the risk for reactivation of occult HBV — only studies that look at antibody responses after vaccination. Some respond, some don’t.
To quote one expert on viral hepatitis, University of Washington’s Dr. Nina Kim:
Bottom line: We don’t have but need longitudinal data showing that vaccination actually helps this subset of patients.
Agree 100%!
Take the poll, folks.
Now watch Nina’s great educational lecture on this mysterious serologic pattern, and come back for this classic.
June 20th, 2025
Federal HIV Guidelines Face a Shutdown — A Critical Loss for Clinicians and Patients
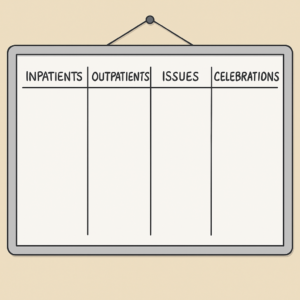 Each week, our HIV clinical group gathers to review active patients, share updates, and celebrate good news. On our whiteboard, we list four columns: Inpatients, Outpatients, Issues, and Celebrations.
Each week, our HIV clinical group gathers to review active patients, share updates, and celebrate good news. On our whiteboard, we list four columns: Inpatients, Outpatients, Issues, and Celebrations.
This week, under “Issues,” one of my colleagues wrote:
HIV Guidelines: ☹️
Yes, you read that right. This week, we learned that the federal HIV guidelines — long the most cited national standard for clinical care — may soon lose NIH support. Here’s what the official letter said, shared with me by a current panel member:
After careful consideration, leadership at the National Institutes of Health (NIH) has determined that NIH support provided by the Office of AIDS Research (OAR) for the HIV clinical practice guidelines will phase out by June 2026. In the climate of budget decreases and revised priorities, OAR is beginning to explore options to transfer management of the guidelines to another agency within the U.S. Department of Health and Human Services (HHS).
The key phrase here is “in the climate of budget decreases and revised priorities,” which basically means someone has decided that the national standards for HIV treatment aren’t worth spending money on. Let’s think about this for a nanosecond — how much money is this really saving anyone?
And the “options to transfer management of the guidelines to another agency” face big-time challenges. I have it on good authority from people at HHS that it is highly unlikely any existing agency has the available time or expertise to take it on.
Meanwhile, it’s worth reviewing just how valuable these guidelines have been in establishing an informed, evidence-based standard for HIV care in our country. A historical perspective with some notable milestones:
- First OI prophylaxis recommendation (TMP-SMX for PCP)
- First perinatal guidelines, post-ACTG 076
- First ART guidance responding to the era of combination therapy
And they’ve kept going. Responding quickly to practice-changing studies, these guidelines have truly been a “living document,” publishing updates on a regular basis in a way that would be impossible for most journals.
A disclosure: I contributed to the Opportunistic Infections Guidelines (Bacterial and Respiratory working group) and served on the HIV treatment panel from 2008 to 2016. What impressed me most was the care, rigor, and collegiality of the process. Every recommendation was debated, refined, and re-reviewed, always with the goal of helping clinicians deliver the best possible care.
(For the cynics: Panel members volunteered their time. Translation — we were unpaid.)
The NIH staff overseeing the process had deep expertise in the field and kept the process moving along with an uncanny ability to attend to multiple voices. Plus, they were meticulous about details in a way that card-carrying ID types like me find very reassuring. Remember, many of us exhibit a clinical form of OCD that translates into our history taking and notes. Just the other day, I read a colleague’s note that started with the word “briefly” — and then went on for a thousand words, give or take.
Another disclosure: I now participate in another guidelines group, headed by the IAS-USA. In doing so, one might ask why have two existing sets of guidelines? I’d argue that having alternative voices in this process — one that includes international contributions — enhances the usefulness of both guidelines.
It’s not clear what will happen to the federal HIV guidelines going forward. A discussion about the “transfer” options is planned during an upcoming Office of AIDS Research meeting on June 26. The guidelines discussion will start around 2:15 p.m. ET, with the public comment period scheduled for 3:25 p.m. ET. If you think the guidelines have been important, and worth saving, I encourage you to provide public comment, or email OARACinfo@nih.gov directly.
Now back to the frowny face emoji at the top of this post. I can’t help but connect this decision to another recent action: the abrupt firing of ACIP members. Both seem to reflect the same troubling sentiment we heard not long ago from the current HHS leadership — a desire to “give infectious diseases a break for eight years.”
Why should that break include eliminating something that works this well, and that clinicians actually use? Frustrating.
For the record, if you’re wondering what landed in the “Celebrations” column on our whiteboard this week — it was the graduation of our ID fellows.
Here are two of our stellar grads, making me optimistic about the future of infectious diseases, “break” or no “break.” Congratulations, Cesar and Gaby! And thank you for sharing the photo.

Me with two future ID clinical leaders; photo posted with permission. (I’m the old guy in the middle.)

