An ongoing dialogue on HIV/AIDS, infectious diseases,
October 4th, 2020
Does the White House Outbreak Invalidate the Strategy of Frequent Testing for COVID-19 Control?
As I’ve written here many times, I’m hopeful that frequent, inexpensive, rapid home testing for COVID-19 will help us climb out of this pandemic mess.
Let’s name it the Mina Frequent Testing Plan, after my indefatigable colleague Dr. Michael Mina who has championed it for months — most recently in a perspective published in the New England Journal of Medicine.
For the Rip Van Winkles out there, here are the basics of this approach:
- Much of the community transmission of SARS-CoV-2 comes from people who don’t know they are infectious since they have no or few symptoms.
- Testing them using standard PCR tests is impractical — too slow, expensive, and difficult to access.
- Scientists and companies have collaborated to develop simple paper-based rapid tests done on saliva samples.
- Results return in 15-30 minutes and require no special instruments for interpretation — analogous to home pregnancy or HIV tests.
- Produced at scale, the tests are cheap and readily available — $1-5 each.
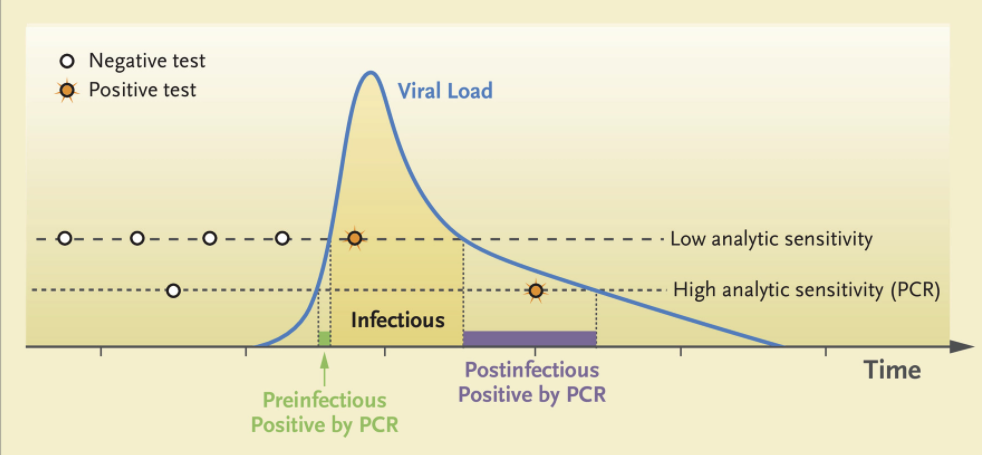
- These tests pick up some people who have high levels of infectious virus but are either asymptomatic or presymptomatic — hence potentially contagious to others but otherwise unaware themselves. Now, none of these people are being detected.
- Once they have a positive test, they isolate at home — they don’t go to work or school. Tests would be confirmed using standard PCR.
- Individuals can also buy them for use at home.
- Schools, hospitals, nursing homes, food service companies, places of worship, and others can purchase them in bulk, with requirements for a negative test (even better, a series of negative tests over the previous several days) for entry.
The strategy has a growing number of advocates across the medical, scientific, and public health fields — including the FDA — which is exciting. Here’s a short white paper on the topic many of us have helped draft, with a focus on testing in schools.
But as the Mina Frequent Testing Plan drew sufficient attention, various criticisms appeared, in the press and on social media. (Here’s a skillful rebuttal.)
These negative views certainly raise important concerns. I worry in particular about false positives — they will be inevitable when doing high-volume testing on a low-prevalence population.
Now, we have a president who acquired COVID-19 despite the fact that he and those who surround him are tested often.
How did this happen? Is this the death knell of the Mina Frequent Testing Plan?
The obvious first explanation is that no test is perfect. The rapid antigen tests used by the White House will miss some people who are infectious. Of particular concern are those who get tested only once, right before meeting the president.
The math is simple — if you increase the number of visitors, you increase the chance that at least one person with infection will escape detection with a single rapid test.
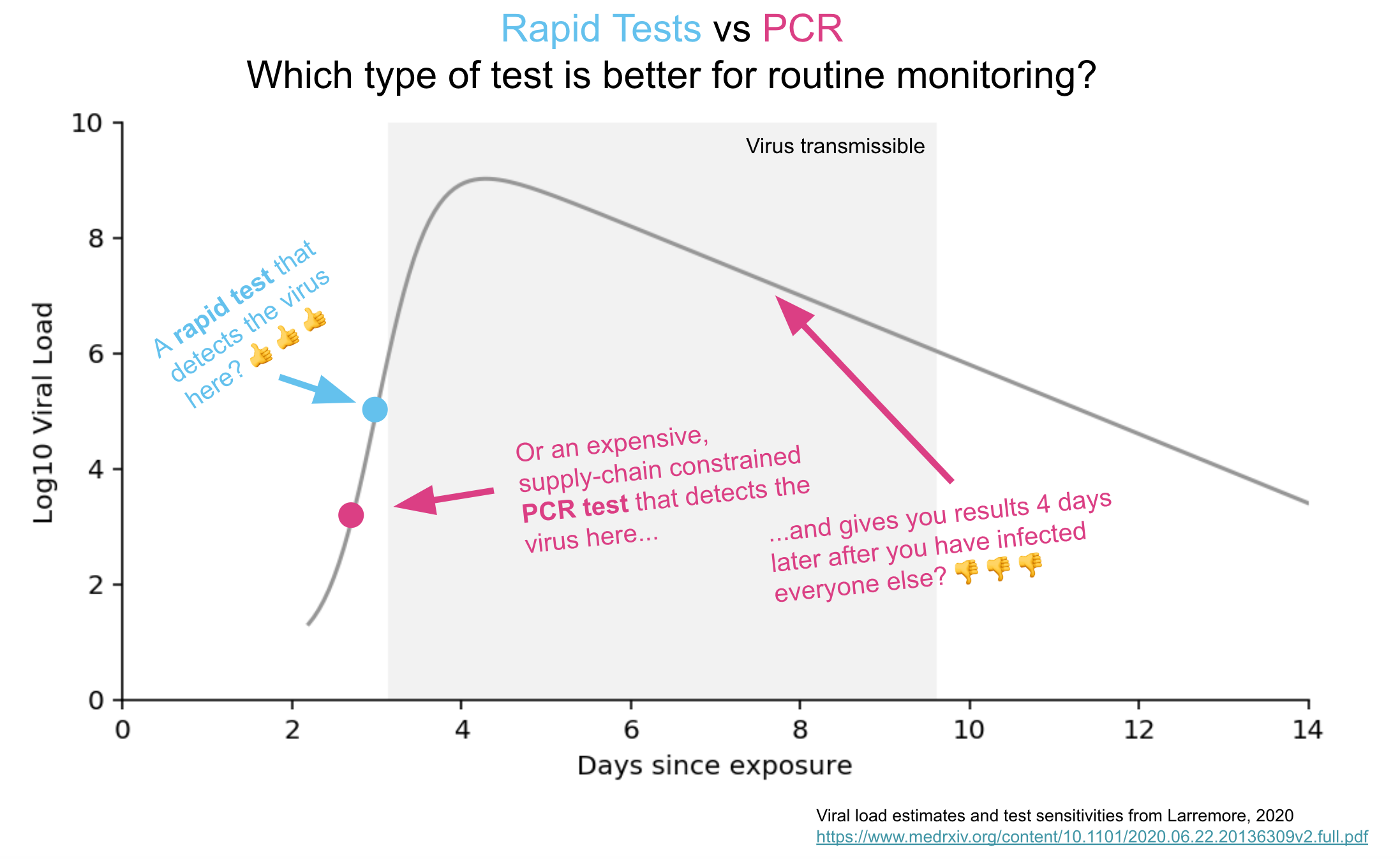
Remember, one strength of the Mina Frequent Testing Plan is just that — it’s frequent! People who test negative in the early phase of infection will test positive with tomorrow’s or the next day’s test based on the kinetics of viral replication in someone who has just come down with the disease.
From Mina’s NEJM piece, here are those viral trajectories — a person with a negative test in the morning could potentially be infectious shortly thereafter:
With the many visitors to the White House on Saturday, September 26 — the day the president announced the nomination of Judge Amy Coney Barrett to the Supreme Court — only a single rapid test granted them access to the event, mask-free.
Also, let’s remember that testing won’t give us a free pass to behave as if we were living in the Before Times, again because testing isn’t perfect. Certain activities facilitate spread of the virus — crowds, close conversations, poor ventilation.
How about this for an example?
At least 7 people who attended ACB's nomination ceremony in the Rose Garden on Sep. 26 have since tested positive for coronavirus. But experts say the more risky time spent that day was at a reception inside the White House. Here are some scenes. https://t.co/mTsZsxmSfy
— Christiaan Triebert (@trbrtc) October 3, 2020
Ouch.
Or this?
Double ouch! Watching that video makes most of us ID clinicians feel like we’re living on another planet. Suspect many of you readers feel the same!
In summary, let me quote my Boston ID colleague Dr. Roby Bhattacharyya, who wisely wrote:
People tap-dancing prematurely on the grave of rapid testing should reflect on how remarkable it is that for people behaving this way all year, indoors and out, in a place with countless thousands of visitors, it took until October for a superspreading event to happen. Test more.
So yes, the Mina Frequent Testing plan lives on — even if the track record of keeping the president free of the virus does not.
Which teaches us more about the limits and vagaries of human behavior than it does the limits of testing, doesn’t it?
September 27th, 2020
Humbled — But Still Hopeful
When Dr. Anthony Fauci joined us earlier this month for a virtual medical grand rounds, several of my colleagues participated. At the end, each was asked to comment about what they had learned so far from the COVID-19 pandemic.
Dr. Michael Klompas, our brilliant hospital epidemiologist, wisely answered:
Humility.
His answer resonated strongly again, because this week our hospital is facing a cluster of cases on our inpatient service.
I want to underscore that Mike and our infection control team have worked tirelessly on our COVID-19 response right from the first moment we heard about it in January — longer than anyone. They have done an exemplary job, providing transparent and evidenced-based guidance. They have done everything they can to keep our patients safe, and bring us to work safely as well.
The clinical staff — doctors, nurses, respiratory therapists, pharmacists, physical therapists, social workers, dieticians — adhere to infection control policies. Same for other essential workers delivering food, cleaning the rooms, working in the cafeteria, transporting patients.
But we humans are, well, human. Meaning not perfect. Nor are systems created by humans perfect. We are constantly learning. To pretend otherwise would be hubris.
And our cluster is a reminder that this is a tricky virus. As some have said, the Goldilocks’ porridge of viruses when it comes to how it spreads.
Not so universally severe that it can be diagnosed and contained once identified — like Ebola, SARS, MERS.
Not so well-understood from a transmission perspective that cases can be prevented through avoiding exposures and targeted immunization — rabies.
Not so mild in most people that we can tolerate nearly universal infection — Epstein-Barr virus.
To cause a pandemic, the likes of which we haven’t seen in over a century, SARS-CoV-2 has to be just right.
It causes a mild infection in most (not all) young people; becomes progressively more serious as we age; takes advantage of those with common comorbidities (diabetes, high blood pressure, obesity); and — here is the crucial factor — spreads to others before we have symptoms.
Or even have no symptoms at all.
Now, as the hospital tests literally thousands of employees, sequences the virus, does engineering analyses, and conducts behavioral interviews, we’ll optimally learn what happened with this cluster so we can prevent it from happening again — both here and elsewhere.
Yes, humbled. But optimistic that with continued transparency about what we find, there will be progress.
September 20th, 2020
Sports During COVID-19 — When What Doesn’t Matter Actually Matters a Lot
A few weeks ago, I got a text from a long-time ID colleague here in Boston:
Hey Paul want ur opinion … this is for an interview with MLB radio, and no one knows less about baseball than I do, but as an avid fan and wise ID doc, do you think the season should continue?
Confession — it took me around 3 milliseconds to respond, if that.
And my answer was yes.
But, some no doubt are thinking, we’re in the middle of a pandemic. It’s hardly under control. A bunch of players had already tested positive, proving it’s not safe.
And — let’s remember — it’s just sports. Sports don’t matter.
But here, in all its tarnished, selfish, complicated, and ultimately messy way, is why I still think it’s worth trying to play professional sports in 2020.
These professional leagues have extraordinary resources — and the motivation — to control outbreaks. The NFL alone boasts annual revenues of $25 billion. You think this might motivate the owners to play the games safely?
The players’ careers don’t last forever. The average professional football player’s career length is only 3-4 years, Major League Baseball 5-6 years. That’s the brief time most of these supremely talented individuals make the bulk of their life’s earnings.
The slowed reflexes, loss of muscle strength, decreased vision, accumulating injuries, and other changes brought on by aging loom as opponents that no athlete has ever beaten. A fast, hungry young rookie is always coming up to take their place — especially if they’re not superstars.
The clock ticks down on these brief careers even during a pandemic.
Sports have already taught us something about disease control — and can teach us more. With coordination well beyond what our government appears willing, motivated, or capable of doing, they have deployed extraordinary strategies that, so far, have been remarkably effective.
Can anything be more of a success story than the NBA? Who could have predicted that they would have zero COVID-19 cases when they placed hundreds of young men into Florida during a surge of cases?
Their strategy of frequent testing, creating a limited “bubble” of exposures, and importantly getting buy-in from both the ownership and the players now is being emulated by other industries.
Not only that, they helped validate a new technique for using saliva for COVID-19 testing.
I’ve made no secret that I don’t like football, and confess I prepared myself to reject whatever plan the NFL came up with to play the games safely. The decades of denials the NFL tossed out about the hazards of the sport gave me no confidence they could possibly go forward with a legitimate plan.
But no! After listening to this Freakonomics podcast, I was frankly blown away at their thoughtful and highly detailed approach. This includes frequent (daily!) testing, active participation of the players’ union and the league in civilized negotiations about policies, reliance on science rather than emotion or politics to do the right thing, wow — this is how to bring an epidemic under control!
Professional sports give many of us something we need right now — a distraction. Pandemic. Fires. Violence. Racial tension. The death of an inspirational public figure. Raging political discord.
Yep, 2020 has it all. Why not enjoy a few moments away from these nightmares to watch Naomi Osaka storm back and win the US Tennis Open, or LeBron James fight Father Time in the NBA playoffs, or Mike Trout continue a career that looks like he could become one of the greatest baseball players of all time?
With echoes of FDR’s advice to proceed with the baseball season despite World War II, again sports can give us a well-needed reprieve from the grind of daily existence, both as fans and as participants.
One of my patients, mostly very isolated since early March due to COVID-19, kindly shared the above picture with me since he knows we share a fondness for baseball. (Ok, “fondness” = obsession.)
It’s a promotional photo taken with Mickey Mantle in 1956, the year he (Mantle) won baseball’s Triple Crown. (I’m sharing it with my patient’s permission.) Take a look at that kid’s face! And thinking about sports still gives him pleasure today.
Some might argue that these professional leagues’ safety measures divert resources (especially testing) away from schools, nursing homes, and other settings that need them more. Fair enough.
But is there any indication that if pro sports didn’t start up again, that the tests would have flowed to the schools? As noted by Will Leitch, “All of us should be able to get tested easily and quickly! But that fact does not inherently mean that what leagues are doing is wrong.”
So let’s play ball — and hope we learn something from these professional leagues about how to control the pandemic by getting buy-in from all involved.
And, most importantly, by following the science.
September 13th, 2020
Restaurants Are Hurting — But Dining Indoors Poses Real COVID-19 Risk
As we learn more about transmission of SARS-CoV-2, the news for restaurants goes from bad to worse.
And while there’s a long list of sad things about this pandemic, the decimation of the restaurant business for owners and the people who work there is right up there. The loss of the restaurant experience for us diners is pretty sad, too.
Importantly, restaurant dining isn’t one of those hypothetical risks for COVID-19, such as surface contamination of groceries and delivered packages. It’s a real, well-documented concern with strong supporting evidence.
In a CDC study conducted at 11 healthcare facilities and just published last week, investigators queried 154 people with symptoms consistent with COVID-19 and positive tests, along with 160 control individuals testing negative. They asked about various activities in the two weeks prior to the onset of symptoms — eating out, shopping, going to an office, visiting a hair salon, taking public transportation, attending a religious service, and others.
People with positive test results were more than twice as likely to have reported dining at a restaurant than were those who tested negative. No other activity conferred significant risk.
It’s a small study, and the authors note several potential limitations, but they amplify the message that crowded settings, close contact, and lack of mask wearing indoors increase the risk of COVID-19.
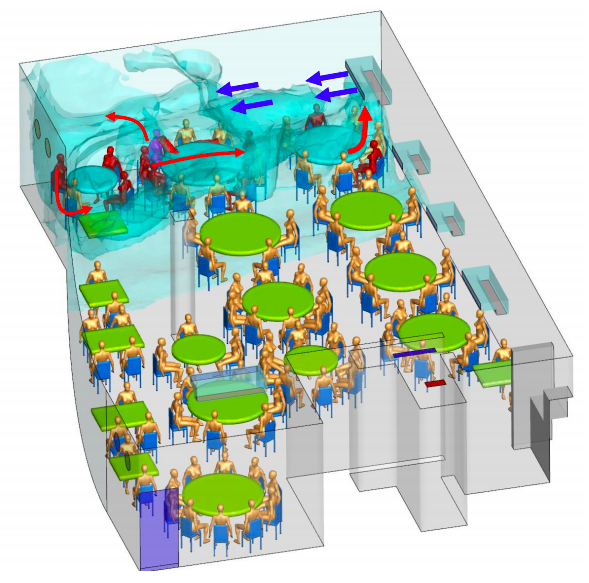
The vagaries of restaurant ventilation — so exquisitely detailed in this investigation of a restaurant outbreak in China — add to the hazards of indoor dining.
Here, one presymptomatic person infected nine other diners, all of whom sat under the the same air conditioning vent that recirculated “old” rather than fresh air.
None of the 68 diners in other areas developed COVID-19, nor did any of the 8 waiters — likely because transient contact is much lower risk.
Meanwhile, Harvard epidemiologist Professor Miguel Hernan compares epidemic curves in New York and Madrid in this fascinating thread:
1/
Look at the shape of these curves.New York and Madrid had similar epidemics until they spectacularly diverged.
In March, both cities were caught by surprise and shut down because of #COVID19.
In September, the situation is under control in NY and alarming in Madrid.
Why? pic.twitter.com/VF0BCl0xyt
— Miguel Hernán (@_MiguelHernan) September 11, 2020
What does this have to do with restaurants?
In New York, indoor dining is CLOSED. Indoor dining in Madrid was OPEN at 60% capacity in June. Bar service opened too. Protocols weren’t aggressively enforced. Since June it has been easy to find crowded bars and tables. The contrast with NY was striking as anyone spending time in both places can tell you.
Is it too far fetched to extrapolate from these cross-city comparisons and conclude that opening restaurants played a role? Not really, when you consider how cases in the southern US spiked when bars and restaurants opened in regions that still had significant community transmission.
(And having had the pleasure of dining late — and I mean late — into the evening in Madrid, I can assure you that these meals are the very opposite of transient when it comes to potential exposure time.)
As noted above, all this information about restaurants and COVID-19 risk makes me very sad. Having grown up in New York — arguably one of the world’s great restaurant cities — I love the way a top restaurant experience provides more than just excellent food. The atmosphere, the conversational buzz, the decor, the rituals, and of course the intermingling of so many different cultures enhance our lives in countless ways. Certainly I’m not alone in missing this colorful aspect of life from the Before Times.
Not only that, but my mother worked as a food writer, and for years wrote a weekly column in the New York Daily News on hidden restaurant gems in the city. If a new Ecuadorian restaurant opened in Queens that generated some buzz, you can be sure we’d soon be sampling some empanadas ecuatorianas or llapingachos.
Meanwhile, awaiting a vaccine and other preventive strategies, what can we do now to support these hurting restaurants?
Dine outside while we can. Tip heavily. Order take out. Buy merchandise. Other ideas here.
But skip the indoor dining in restaurants for now. And while we miss it, it might help to remember that eating out isn’t always so great.
https://youtu.be/K_q4S7lZeik
September 7th, 2020
Relieving the COVID-19 Testing Logjam by Separating the Symptomatic from Asymptomatic
 As the days grow shorter and we celebrate Labor Day here in the United States, the end of summer looms awfully near. With that will soon come colder temperatures, more time spent indoors, kids back in school, and the inevitable respiratory virus season.
As the days grow shorter and we celebrate Labor Day here in the United States, the end of summer looms awfully near. With that will soon come colder temperatures, more time spent indoors, kids back in school, and the inevitable respiratory virus season.
How we address these “viral URIs” in the midst of the COVID-19 pandemic presents a major challenge for clinicians, patients, healthcare systems, and — the focus of this piece — diagnostic laboratories.
Because while certain symptoms might suggest rhinovirus or influenza or RSV or adenovirus or metapneumovirus more than SARS-CoV-2, there is no single clinical sign or symptom that would reliably separate one from the other.
Which means that essentially everyone with a viral respiratory tract infection is eligible for — and arguably needs — COVID-19 testing. This adds considerable volume to an already overburdened testing system that, in this well-argued piece by Atul Gawande in The New Yorker, is “as messed up as a pile of coat hangers.”
What I would propose is that we start by separating out symptomatic from asymptomatic testing. Let’s use a quick and less expensive antigen test for asymptomatic testing, and save the PCRs only for people with symptoms.
We have to do something. The demand for asymptomatic COVID-19 testing is already off the charts, increasing all the time.
One of my colleagues mentioned to me that testing people without symptoms is at least 40% of our hospital’s testing volume. Most of these tests are for admissions (all get tested) and for pre-procedure tests, but increasingly also for travelers re-entering Massachusetts or visiting Maine, people who want to see elderly family or friends, as part of school entry requirements, or just someone worried about a recent potential exposure.
But, you note, aren’t these antigen tests notoriously inaccurate? Won’t they miss cases because they aren’t as sensitive as PCR? Indeed, something of a backlash on rapid home testing appeared recently in a New York Times piece (one I happen to disagree with, for the record), and this lack of sensitivity was highlighted:
Experts also noted that antigen tests aren’t great at sussing out small amounts of the coronavirus, which means they’re far more likely to miss a case that a technique like PCR would catch.
For testing of asymptomatic individuals, it’s worth addressing this concern head-on. Because over the last week, I’ve been asked several times to explain why tests for COVID-19 could be different in symptomatic versus asymptomatic people.
Once it was to a group of research scientists.
Once it was to a local news reporter.
Once it was to a gastroenterologist.
Once it was to a bunch of friends in our backyard, during a socially distanced gathering.
All were worried about lower sensitivity of non-PCR testing.
From this diverse group of people, we can conclude that the concept of accepting a less-sensitive test for testing people without symptoms deserves further clarification — it’s a tough one to master, employing the scary-sounding concepts of Bayes’ Theorem.
So let’s get out our #2 pencils, or our handy Bowmar Brain, and do the math. And, following up on a presentation I made this past week on the topic, and a piece co-authored last month with my colleague Dr. Jeffrey Schnipper, we’re going to consider a very simple case.
(The nice editors at STAT wouldn’t let us publish the full math, except in a linked appendix. Since this is my blog, I can write what I want, so am including it here.)
Here’s the case:
August 2020, Boston.
41-year-old woman planning her summer vacation.
Business consultant; has been working remotely since mid-March.
Lives with husband and 2 children, ages 13 and 9.
Completely asymptomatic; everyone in the household well.
Needs testing for COVID-19 before entering the state of Maine.
What are the chances this woman has a contagious infection with SARS-CoV-2? (She has no symptoms, so that’s the “disease” we are testing for.) We’ll call this estimate our pre-test probability — it’s the likelihood a disease is present even before we do any testing.
In asymptomatic people in Boston currently, the pre-test probability is at most 1%. This is the positive test rate at our hospital now among people without symptoms. Now that we have that estimate, it’s math time!
- For 1000 people like this currently, 10 (1% of 1000) will have COVID-19, and 990 would have nothing.
- A test with 80% sensitivity will be positive in 80% of these 10 — or 8, missing 2 cases.
- The test will be negative in 992 people, which includes the 990 without COVID-19, plus the 2 with the infection we missed.
- The negative predictive value — which is how often the test correctly calls someone negative — is 990/992, or 99.8%.
The chance of missing an infectious case with antigen testing is only 2/1000 — and potentially lower since those who are most infectious have the highest amounts of virus, making false-negative results less likely. This 99.8% negative predictive value is plenty high enough for routine use in asymptomatic people, where the goal is detecting people who might be contagious without knowing it.
In fact, the big worry for testing asymptomatic people is the opposite — a false-positive result. Since false positives are so much more likely in a low prevalence population, all positive results will need confirmation by PCR.
But the take-home message from going through this exercise is that we should not hesitate to deploy “good enough” testing for screening low-risk people without symptoms. The pre-test probability is key to defining the trustworthiness of a test result.
And now you can cue the Jim Gaffigan-esque self-criticizing, high-voice stage whisper: Did he just to write about COVID-19 testing again? Can’t he write about anything else?
Hey, last week I wrote about reinfection!
Take it away, Jim — we need you now more than ever!
August 30th, 2020
Cases of SARS-CoV-2 Reinfection Highlight the Limitations — and the Mysteries — of Our Immune System
In case you didn’t notice, or perhaps were “off the grid” taking some well-earned time away from COVID-19 news, this past week we heard about several cases of SARS-CoV-2 reinfection.
We’ll come back to them in a moment, but first, some questions:
- Why does one parent never get sick when their kids start coughing and sneezing and dripping with colds, while the other gets a cold every single time?
- Why do some tourists happily dine on delicious street food in Mexico City, while this same cuisine will put others in their hotel bathrooms for the whole trip?
- Why are some people repeatedly plagued with strep throat, while others never get it in their lifetimes?
- Why is infection with Epstein Barr virus (nearly 100% in humans by adulthood) most of the time asymptomatic, while a certain unlucky few will be laid up with severe mononucleosis for weeks?
- Why did some gay men in U.S. cities contract HIV in the early 1980s after relatively few exposures, while some others with multiple known HIV-positive contacts never did? How did some commercial sex workers in Africa in the early 1980s escape HIV?
- Or, perhaps most relevant to the COVID-19 re-infection cases, why do some people get the flu twice within the same flu season? Or some (rare) people get chicken pox twice? (The second case is usually quite mild, fortunately.) Or even measles!
I start with these examples (and I could have chosen dozens more) to highlight that there’s a ton we don’t know about infection, immunity, and how they interact to protect us — or not to protect us — from disease.
So after hearing anecdotes about SARS-CoV-2 reinfection for months (many of them false-calls based on persistent low-level PCR positivity, not reinfection), now we have actual cases, and it’s worth considering some of the details.
The first occurred in a 33-year-old man 142 days after his initial symptomatic infection. Authorities picked up the infection on a screening test when he went through the Hong Kong airport, as he had no symptoms. In fact, he remained asymptomatic throughout. A brisk antibody response developed shortly after, a response not detected the first time.
Sequencing the virus from the two infections showed sufficient differences to prove reinfection, rather than relapse.
As noted wisely by immunology professor Dr. Akiko Iwasaki, “This is no cause for alarm – this is a textbook example of how immunity should work.”
Phew.
News then broke with additional cases in Europe and Ecuador, about which we have limited details.
But this U.S. case in a 25-year-old immunocompetent man from Nevada deserves attention, and likely some worry.
Here are the clinical details of the history, summarized from the available pre-print (it has not yet been peer reviewed):
March 25: Onset of sore throat, cough, headache, nausea, diarrhea.
April 18: Tested positive for SARS-CoV-2 by PCR.
April 27: Symptoms resolved.
May 9 and 26: Tested negative for virus by two methods.
May 28: Onset of fevers, headache, dizziness, cough, nausea, and diarrhea. Chest x-ray negative.
June 5: Symptoms worsened, and now with hypoxia; admitted to the hospital and found to have new infiltrates on chest x-ray. PCR positive for SARS-CoV-2.
June 6: SARS-CoV-2 IgM and IgG antibody positive.
The authors state that the viruses isolated from the first and the second illness show sufficient genetic differences to support reinfection, rather than relapse. The likely source of the second infection was a parent, suggesting household transmission, though the sequences from the parent are not available.
These important case reports raise many questions, about which today we can only speculate, which is why many of the sentences following have question marks.
- How often does reinfection happen, and why? It doesn’t appear common, but we must conclude from these cases that it does occur. Perhaps with similar frequency to other coronavirus infections in humans?
- Will cases be as severe as the first infection? Based solely on the Nevada case’s household contact, it’s possible that severity may be related to intensity of exposure. Maybe he was not taking precautions in the household, believing himself immune? Some believe inoculum is an overlooked aspect of COVID-19 disease severity.
- When reinfection happens, will these new cases carry the same risk of transmission as the first infection? We will have to assume so, but it is plausible that an immune response will render people less infectious to others.
- How do these cases factor into policies about screening people who have already recovered from COVID-19? Given the long duration of PCR positivity in some people, some infection control specialists have advocated not retesting people who are admitted with prior disease if they are asymptomatic. Same for preprocedural screening. Seems we may need to put this policy change on hold until we have further data on reinfection, and how often it occurs.
- What are the implications for vaccine efficacy? Will a vaccine even work? If so, for how long? The cases suggest that a vaccine may need to be repeated periodically, but optimists can point to the HPV vaccine as a model of how vaccine immunity can be stronger than natural immunity, so we’ll see.
So remember, there’s a lot we don’t know about our immune system, and how it works — and this is particularly true for a new infection and disease.
But one thing I do know?
“Immunity Passports” are dead.
August 24th, 2020
FDA’s Emergency Use Authorization for Convalescent Plasma for COVID-19 Seems To Be Fooling No One
 Starting late Saturday night, and proceeding the next day — like a relentless series of coming attractions for a blockbuster summer movie or the finale of a reality TV series — we repeatedly heard word that the President planned to make an announcement Sunday evening about a “major therapeutic breakthrough” in treatment of COVID-19.
Starting late Saturday night, and proceeding the next day — like a relentless series of coming attractions for a blockbuster summer movie or the finale of a reality TV series — we repeatedly heard word that the President planned to make an announcement Sunday evening about a “major therapeutic breakthrough” in treatment of COVID-19.
6 p.m. Eastern. Live. Get ready. Here it comes.
And, satisfying the ratings-hungry entertainer he once was (and some would say still is, though “entertainer” must be used cautiously in this context), we turned up to hear him cite this “powerful therapy” that “had an incredible rate of success.”
No, it’s not hydroxychloroquine.
This time it’s convalescent plasma. That liquid gold harvested from recovered COVID-19 patients, swimming in antibodies directed against SARS-CoV-2, and also containing a veritable secret sauce of illness-reversing substances that have fascinated doctors and scientists for decades.
Never mind that harvested convalescent plasma isn’t used commonly to treat any infection currently.
Or that the randomized trials of this treatment have so far been disappointing.
Or that the observational data the FDA used to justify their action come from an unpublished study not yet subject to peer review.
(Here’s the next best thing, for those inclined to take a deep dive into data analysis.)
Or that the very experts employed by the government to review plasma’s safety and efficacy have as recently as last week raised important concerns about the lack of convincing evidence for this treatment.
Or that this action by the FDA will almost certainly jeopardize any existing randomized trials of convalescent plasma in the United States.
Or that the person from the FDA who reviewed the plasma data had his name redacted from the memo.
Or that the emergency use authorization may make patient care more difficult, since this will necessarily be a limited resource — especially if antibody titer turns out to be a critical determinant of whether this works, and since antibodies appear to fade in many people soon after they have COVID-19.
Nope — no matter. On the evening of a major political event — timing that cannot be coincidental — the president got his ratings.
He had to do a little intimidation, but we’re getting used to that.
The deep state, or whoever, over at the FDA is making it very difficult for drug companies to get people in order to test the vaccines and therapeutics. Obviously, they are hoping to delay the answer until after November 3rd. Must focus on speed, and saving lives! @SteveFDA
— Donald J. Trump (@realDonaldTrump) August 22, 2020
The good thing is that no one in the scientific community is fooled. I have not heard from a single ID specialist who believes this action was supported by existing data, and indeed our professional society agrees.
Convalescent plasma may work to help people with COVID-19.
But if it does, we don’t know how much, or who are the most likely to benefit, or how to select the right donors.
Because given the absence of controlled trials, right now in the U.S. what we have are 70,000 anecdotes — that’s how many people have received it in this country — tied together by individual reports and separate observational studies.
For the true evidence, we’ll have to wait for the randomized, controlled clinical trials.
The ones going on in other countries.
August 16th, 2020
Picking the Top Internet ID Resources, and a Wistful Look Back at the CDC That Was
Over on Open Forum Infectious Diseases — and that’s abbreviated “O-F-I-D”, not “Oh-fid”, thank you — I sometimes invite other ID-types to join me on a podcast to pick their favorite ID-related item:
Examples of these mock “drafts”:
And some time this past winter (a million years ago), ID PharmD extraordinaire Monica Mahoney came up with a great idea for one of these drafts — top ID-related internet resources.
We recorded it in my office in February, our wonderful audio editor Meredith Mazzotta edited the audio file to make us sound more articulate — and then, because I was on service in late February, we didn’t post it right away.
Well, you know what happened next. A pandemic happened, meaning the world exploded. It didn’t seem quite right to release something so lighthearted and COVID-free in March.
Tell me — would you have wanted to read something about the joys of air travel in mid-September, 2001? So we shelved it, awaiting a more stable time.
Fast-forward to now, and I’ve decided we’re ready. After all, Monica is thoughtful and funny and loves to teach, so why not expose the world to her talent?
But before you listen to our picks, I’ll share my #1 pick of the best ID internet resource at the time, because it has special resonance now in a post-COVID-19 world. It’s the CDC web site, and here’s what I said (lightly edited):
I think the CDC site is a work of genius. It’s comprehensive. It’s broad. It’s updated all the time. It’s graphically terrific. It shows you sometimes your taxpayer dollars do really good work. I use it for all kinds of things. Example: I am not a travel medicine doctor, but of course, all ID doctors get asked travel questions. I use it for that all the time. Not surprisingly, when there are emerging outbreaks, it is the first place you go to find the latest information. They are extremely diligent about keeping it up to date. … It is really a remarkable thing, and it makes me very proud and very patriotic (sometimes not easy these days), to say that cdc.gov is my number one choice for an ID internet resource.
I bolded that last part, since it’s so painful to read today.
Not because what I said was wrong at the time. If we think back to Zika, Ebola, pandemic flu, West Nile, Candida auris, HIV, HCV, STIs — basically anything except COVID-19 — the CDC site has been the place to go to find the most updated and reliable information.
Now, not so much. Never has so much talent and potential been wasted, undermined by a federal government that seems intent on undercutting what CDC does best, which is responding thoughtfully and carefully to infectious threats, using the best available data.
Wouldn’t it be great if these experienced public health officials were given the resources and allowed to use their expertise to take control of our national COVID-19 response? If they issued frequent briefings with the latest national information? If they remained free of the politicization that has so bedeviled our response to the pandemic right from the start? From a recent outstanding summary, published in The Atlantic:
On February 25, the agency’s respiratory-disease chief, Nancy Messonnier, shocked people by raising the possibility of school closures and saying that “disruption to everyday life might be severe.” Trump was reportedly enraged. In response, he seems to have benched the entire agency. The CDC led the way in every recent domestic disease outbreak and has been the inspiration and template for public-health agencies around the world. But during the three months when some 2 million Americans contracted COVID‑19 and the death toll topped 100,000, the agency didn’t hold a single press conference. Its detailed guidelines on reopening the country were shelved for a month while the White House released its own uselessly vague plan.
Isn’t it the height of irony that no one uses the CDC as a source for the latest numbers on new cases, percentage of positive tests, hospitalizations, and mortality?
Sure, they still do some good COVID-19 related research, and set important policies using the best available information.
But they could be doing so much more, if given the chance. Aaugh! So frustrating.
So take it away, Monica. Let’s hear about some other great internet resources. And use the comments section to let us know yours.
(Read the transcript: Debating the Top ID Internet Resources with Dr. Monica Mahoney.)
August 4th, 2020
Carbapenems and Pseudomonas, Lyme and Syphilis Testing, a Bonus Point for Doxycycline, and Some Other ID Stuff We’ve Been Talking About on Rounds
 As noted multiple times, many of us ID doctors attend on the general medical service. This offers us a chance to broaden our patient care activities and to work with medical students, interns, and residents.
As noted multiple times, many of us ID doctors attend on the general medical service. This offers us a chance to broaden our patient care activities and to work with medical students, interns, and residents.
Boy, that’s fun!
Yes, those of us who attend on medicine enjoy it enormously, though the experience humbles us on a daily basis about what we need to learn in cardiology, nephrology, gastroenterology, rheumatology, hematology, endocrinology — you name it.
Fortunately, the smart trainees (and subspecialty consultants) teach us tons.
Plus, at our hospital we have a co-attending system, meaning my knowledge can be amplified by another experienced doctor — this month an endocrinologist, who has fortunately for all of us never encountered a metabolic disturbance (electrolytes, minerals, glucose) he can’t solve.
https://twitter.com/BrighamChiefs/status/1285652513333686274?s=20
So this week we take a partial break from the COVID-19 coverage, and summarize some ID stuff we’ve chatted about on rounds.
- Meropenem and other carbapenems are not good drugs for treatment of Pseudomonas aeruginosa.. Resistance can develop quickly through alteration of porins or increased efflux pump activity. Ertapenem, for the record, has no reliable activity at baseline. And did you know that ID docs often abbreviate this tricky but common organism as PsA?
- Doxycycline partially protects against the development of C. diff. Yet another a reason why it’s many ID docs’ favorite antibiotic. Bonus podcast at the bottom of this post.
- Diagnostic testing for Lyme disease is a mess. Link is to a very quick slide set. And yes, we still await the final publication of the Lyme IDSA guidelines, released in draft form last year, and expected in the late summer/early fall.
- Diagnosis of another disease caused by spirochetes — syphilis — is also a mess. How many people can clearly explain what a one dilution, one tube, or two-fold change in the RPR means? (Hint, they’re all the same thing.) Link is to another quick slide set. Great new graphic below by the folks from The Clinical Problem Solvers, with a couple of minor suggestions, including a pet peeve — the “need” for LP in ocular/otologic disease. Why do it if you’re going to treat for neurosyphilis regardless of the results?
Very nice graphic! Suggestions:
– Please include the T. pallidum enzyme immunoassay (TP-EIA), which has become the preferred screening test in many places
– Need for LP in ocular/otologic disease is debatable, since we treat for neurosyphilis regardless of results https://t.co/kE2FCihvRm— Paul Sax (@PaulSaxMD) August 4, 2020
- Ocular syphilis has diverse clinical presentations, most commonly blurred vision, sometimes with photophobia and eye redness. The ophthalmologists will often diagnose uveitis. RPRs are usually high (median titer 1:128 in the linked series), suggesting relatively recent acquisition, but eye involvement can occur at any stage of syphilis.
- Enterobacter and certain other enteric gram negatives may develop resistance to cephalosporins through “de-repression” of a chromosomally mediated beta-lactamase. The confusing thing about this mechanism is that the organisms initially test as susceptible to ceftriaxone, with resistance emerging with noncurative therapy. Cefepime and carbapenems retain activity.
- Sputum is more sensitive than nasopharyngeal samples for diagnosis of COVID-19 in symptomatic patients. Keep this in mind when ruling out the disease in those hospitalized with negative nasopharyngeal swabs; serology may also be useful if symptoms are of 7 days’ duration or longer. Hey, I said this post was a partial break from COVID-19. Can’t be a full break, not yet — boo hoo.
- “Hypervirulent” klebsiella is an increasingly common cause of liver abscess. Unlike other causes of liver abscess, these cases are usually monomicrobial, frequently have metastatic spread, and may have a positive “string test” in the microbiology lab, demonstrating hypermucoviscosity. Disease is more common in Asia.
- Actinomycosis most commonly occurs in cervicofacial, abdominal, pelvic, and thoracic sites. Organism also may be found in relation to IUDs, usually without symptoms. This slowly growing anaerobe takes advantage of anatomic breaks, trauma, or radiation damage, and can cross tissue planes and lead to draining sinus tracts, or masses potentially mistaken for malignancy. Treatment is long-term penicillin (or amoxicillin).
- None of the recommended first-line HIV treatment regimens include the pharmacokinetic boosters cobicistat or ritonavir. Such boosters greatly increase the risk for drug interactions. This means previously popular treatments — in particular the mellifluously named Genvoya — should be retired as initial therapy.
- Aztreonam has a similar mechanism of action as beta-lactam antibiotics (inhibiting cell wall synthesis), but does not cause similar IgE-mediated type-1 hypersensitivity reactions. One possible exception is for patients allergic to ceftazidime, which has a similar side chain (and antibacterial spectrum). Active only against aerobic gram negative infections, aztreonam has few other indications aside from this lack-of-allergy niche. OK, maybe no other indications!
- Chlamydia psittaci is a rare cause of community-acquired pneumonia. And it’s a favorite of ID case conferences and CPCs. Since the primary source is household birds — especially parrots — I was luckily given the following clues in the linked CPC to frame the discussion, which reads like a ID board exam question:
The patient lived in New England and installed air-conditioning equipment. He owned a ferret and five snakes, to which he fed frozen rabbits and live or frozen rats that he obtained from a pet supply store. His brother owned a healthy puppy. The patient had returned 27 days earlier from a 10-day trip to Hawaii, where he had cut himself on coral while scuba diving. Several of the hotels that he visited had caged parrots in their lobbies.
- The ratio of trimethoprim to sulfamethoxazole in the combination tablets is 1:5. A single strength has 80 mg/400 mg, and a double-strength twice that — hardly anyone knows these arcane facts (except for pediatricians and pharmacists). And aren’t my math skills impressive? Here’s a tip: Since no one on rounds wants to say “trimethoprim sulfamethoxazole” (too long), go with “trim-sulfa.” It’s a better abbreviation than the brand names “Bactrim” or “Septra” (both of which should be retired), and it makes more sense than “co-trimoxazole.” Oh, and this is one of several antibiotics with excellent oral absorption.
- Anaerobic bacteria can cause urinary tract infections. Consider these organisms when your standard urine culture is negative, especially in patients with anatomic abnormalities. And trim-sulfa (commonly used for UTIs) won’t be active against these organisms. Check with your microbiology laboratory about how to evaluate further.
All this antibiotic talk! On the first day of rounds this week, during introductions, one of the residents asked us to say our name and our favorite antibiotic.
Good time to replay the antibiotic draft I did with my friend Dr. Rebeca Plank!