An ongoing dialogue on HIV/AIDS, infectious diseases,
September 10th, 2025
When Required Learning Modules Surprise You (In a Good Way)
 Like most clinicians, I have a checkered history with required online learning modules. You know the drill: click play, get lectured in monotone about hand hygiene or fire safety, then spend the next 8 minutes desperately searching for the fast-forward button, hoping it’s not disabled.
Like most clinicians, I have a checkered history with required online learning modules. You know the drill: click play, get lectured in monotone about hand hygiene or fire safety, then spend the next 8 minutes desperately searching for the fast-forward button, hoping it’s not disabled.
My personal low point (or high point, depending on your perspective) came years ago, when I proudly earned my Certificate of Completion for Disinfectant Wipes — Inpatient Settings. I even tweeted about it at the time, suggesting the Nobel Prize committee might want to give me a call.
(I’ve done you the favor of uploading proof to this site as the featured image, in case you doubt my credentials and are allergic to social media.)
So, when our hospital system announced an incentive program that required completion of something called the Equity-Informed High Reliability Organization (EIHRO) Level 1 Module, I wondered — who comes up with these titles? Is it a team of consultants paid by the syllable? My expectations hovered somewhere between “this is going to be tedious” and “could they imagine anything more soul-crushing?”
But here’s the shocker: it was excellent.
It’s not that the message was so profound or novel. It was the presentation — dynamic, engaging, and useful. Kudos to the narrator for keeping the topic moving along at a brisk pace and the video producer for including images and videos that didn’t look like they were pasted from a royalty-free site or bargain basement clip-art. The content came from a company called SG Collaborative Solutions, which was acquired years ago by a much more familiar player in this usually grim space, HealthStream.
The topic was how to address risk. Instead of the usual “don’t do this, do that” checklist, or calling bad events “mistakes” that trigger new policies, we need to understand the settings and systems that lead to adverse outcomes. It’s not enough to slap “Safety First!” into a mission statement. If you don’t understand the pressures of the actual workplace, the slogan does nothing. The recommended approach instead acknowledges that we all have competing priorities — productivity, efficiency, personal lives — and aims to optimize care in that realistic context.
Call me convinced. It’s a good lesson whether you’re a clinician caring for patients or at home reaching for a dish on a shelf that is a bit too high to reach comfortably. Wouldn’t it be smarter to keep a step stool handy than to wobble precariously on a kitchen chair? And for people who text and drive, just stop already. Which reminds me — to the cab driver in Philadelphia who was texting our entire drive to the airport, it’s not safer just because (as you confidently said when I asked you to stop), “It’s just my son.”
Now, if you’ll excuse me, I’m going to update my CV:
- 2019: Certified in Disinfectant Wipes
- 2025: Equity Informed High Reliability Organization (EIHRO) Level 1 Module
Could this addition tip the scales for the judges in Stockholm?
September 4th, 2025
End-of-Summer Musings — Hepatitis B, Dalbavancin, Alpha-Gal, and More
 The last time I did one of these quick “musings” posts, I listed 21, and someone asked me, “Why 21?” The answer — obviously — is that I originally planned on writing 20, but then had to add a 21st, just because that’s exactly how many points you need to win a ping pong game.
The last time I did one of these quick “musings” posts, I listed 21, and someone asked me, “Why 21?” The answer — obviously — is that I originally planned on writing 20, but then had to add a 21st, just because that’s exactly how many points you need to win a ping pong game.
So here are a bunch more, in honor of another important racquet sport, tennis, which this weekend will reach the culmination of its grueling season in the finals of the US Open. Stick around to the end to see how I tie it in.
1. Hepatitis B transmission occurred in a nursing home from a contaminated glucometer. As is commonly done, glucometers at the skilled nursing facility were shared among several residents. Even though the disinfection protocols were apparently followed appropriately, a person with chronic hepatitis B was the source of a transmission. In an era of near-universal hepatitis B immunization and dropping prevalence of chronic HBV, it’s worth remembering that among our blood-borne pathogens (HIV, HCV, HBV), HBV is by far the most contagious.
2. A strategy of two doses of dalbavancin 1 week apart for Staph aureus bacteremia was noninferior to 4-8 weeks of daily therapy. However, it was not superior based on the primary “desirability of outcome ranking,” or DOOR endpoint. I think noninferior for clinical endpoints is still important for something as transformative as just two doses, though cost remains a huge barrier for dalbavancin. And get ready for a bunch of studies that use this novel DOOR composite endpoint, which incorporates clinical success, infectious complications, safety complications, mortality, and health-related quality of life.
3. Alpha-gal syndrome is tick-related, is increasingly common — but no, it’s not an infectious disease. Raise your hand if, as an ID doctor, you have been asked anyway to comment on the diagnosis or management of this allergic reaction to the sugar molecule galactose-alpha-1,3-galactose. Here’s the chemical structure, in case you’d like to synthesize it during your free time.
4. I thought you couldn’t put the toothpaste back in the tube. Tell me — who would buy this gizmo? Even for only 10 dollars, I just can’t see the use case.
5. Two-drug initial therapy with dolutegravir/lamivudine provided similar results to a standard three-drug regimen of TDF/FTC plus dolutegravir, even in people with advanced HIV disease. I’ll have more to say about this important study in a later post, along with the fine editorial by Dr. Laura Waters — who also issued some wise career advice as she is about to leave her current position in Britain’s National Health Service.
6. China this summer battled an increase in chikungunya cases in Guangdong Province. We periodically see cases in the United States in returning travelers, especially coming from the Caribbean and South America. It is impressive how debilitating the post-infectious arthritis can be with this dengue- and zika-like virus.
7. I received a bunch of supportive comments and emails about my rant against learning objectives, thank you. A favorite was one from Andrea Demeter, who cleverly took to AI to find reasons to get rid of them — which she must have known would prove my point! But if they’re here to stay, maybe in the future AI can generate the learning objectives, generate the lecture and PowerPoint slides, and then generate the evaluation of whether the lecture met the learning objectives. Magic! And no learning required.
8. Federal, state, and professional societies now issue competing (and sometimes contradictory) vaccine recommendations. Examples: Florida plans to eliminate school requirements for vaccines, while California, Oregon, and Washington band together to ensure communication of “credible information” on vaccines, and Massachusetts makes COVID boosters available for all older than 5. You’d think we live in different countries or something. My Boston ID colleague, Dr. Shira Doron, said it best: “The chaos just doesn’t end.”
9. This group argues persuasively that we should designate Chagas disease endemic in the United States. There’s no doubt that this parasitic infection is far more common in our country than we realize, and that autochthonous transmission occurs here — especially in the Southwest. The labeling of the United States as nonendemic leads to inadequate surveillance and clinical knowledge about this potentially serious parasitic infection.
10. Some of the “friends” that dogs bring home are more welcome than others:
11. In this randomized clinical trial conducted in adults older than 65, high-dose influenza vaccine did not prevent pneumonia or hospitalization better than standard dose. The study was large and well-conducted, enrolling 332,438 participants. 332,438! Is this study the final word on this strategy as we await a better flu vaccine?
12. Switching people with HIV on second-line boosted-PI regimens to BIC/FTC/TAF was noninferior to continued PI therapy. Results reinforce the results from the 2SD and VISEND (Arm A) studies, but add baseline retrospective proviral DNA resistance testing in the bictegravir arm, which demonstrated a high prevalence of NRTI resistance. Hat-tip to Drs. Patrice Severe and Serena Koenig and the GHESKIO team for completing this clinical trial during a time of extraordinary civil unrest in Haiti. (I was a co-investigator.) Good accompanying editorial.
13. There have been six rabies deaths in the US in the past 12 months. This is more than the usual number — typically one to three, some years there are zero — for reasons that are unclear. Can anyone find reference to this on the CDC site? Because tracking rabies and the previously mentioned Chagas disease are exactly why we need a strong agency to do national surveillance for infectious threats. The states simply can’t do it all.
14. If you like documentaries about brilliant songwriters, put these two on your list. The first is about Billy Joel — you might have heard of him (you think?); he has a fascinating biography to back up his impressive song catalogue. I enjoyed it a ton even though I’m lukewarm about much of his music. The more obscure offering is about Charles Fox, a person unknown to me before watching this film. But let’s just say if there’s a soundtrack for us boomers who watched TV growing up, he’s written it.
15. HHS cancelled nearly half a billion dollars in research support for mRNA vaccines. This follows cancellation of a grant to Moderna of 800 million dollars. Vaccine experts consider this technology the most efficient way to respond to a pandemic threat; it also has promise for immune-based cancer therapeutics. Discouraging.
16. I liked this critical piece that highlights issues with excess screening requirements in primary care. Problems include misplaced incentives, strategies that are hardly evidenced-based, and fatigued or distracted providers who then miss the important aspects of patient care. We saw this recently as our electronic medical record flagged absence of hepatitis B immunity in all patient’s charts — for what reason, exactly? Drove multiple clinicians nuts with frustration.
17. What’s going on with pivmecillinam? With gepotidacin? With sulopenem? All three have FDA approval to treat UTIs, none is yet available in US pharmacies. The full name of the last one is “sulopenem etzadroxil with probenecid,” but I defy you to type that out every time you write it.
Seventeen Musings! That’s the age of Serena Williams when she won her first tennis Grand Slam title in 1999. And now, in all it’s glory, is a piece that explains why you should play tennis if you can:
18. We fanatics all read and cheered this tribute to the world’s greatest sport. So much here to love: the growing popularity (pickleball notwithstanding), the fitness advantages, the effects on brain health, the chance to play a sport for a whole lifetime. For the record, I think there’s room in the world for lots of racquet sports — tennis, pickleball, padel, squash, racquetball, badminton, ping pong… And not that she needs it, but I’d bet this is the first time that the writing of Alexandra Moe has been featured in an ID blog.
Ok, eighteen Musings — that’s a good number. It even has its own Wikipedia page!
August 29th, 2025
Watching the Chaos at the CDC — with Sadness and Alarm

Image by Jackson Moccelin from Pixabay
Throughout my career as an infectious diseases doctor, the CDC has been a rock-solid source.
- Need reliable data on an outbreak? The CDC.
- Need thoughtful, evidence-based guidelines? The CDC.
- Need an authoritative reference for a consult question or to steer a colleague or trainee to the right place? The CDC.
- Need the latest, most accurate surveillance information on HIV or influenza or dengue or you-name-it? The CDC.
- Need advice for your friend doing anthropology research in rural Bolivia and wondering whether they should take malaria prophylaxis (yes), and what it should be (multiple options)? The CDC.
Did I always agree with every word? Of course not. Show me an ID doctor who always agrees with every guideline, and I’ll show you a cephalosporin that covers enterococcus.
For example, for years I’ve thought we’re too aggressive with “bat in bedroom, no bite” postexposure prophylaxis, preferring the Canadian approach. But I never doubted the people making the U.S. guidelines had done their homework with integrity; they weren’t part of some sinister rabies vaccine/immunoglobulin cabal. It was a difference in opinion, that’s all.
And I trusted the people. The ones I’ve known who have worked at the CDC are mission-driven and incredibly hard-working. They’re not looking for fame or fortune, to cultivate a brand, or to make a splash in the media. You don’t expect to see a TikTok video from a CDC official. They’re the kind of colleagues who disappear into data sets, surveillance reports, and fieldwork, all in the service of preventing disease and saving lives.
So what happened?
In a word: COVID. The pandemic was the public health earthquake of our lives, and the aftershocks continue. The CDC is one of its casualties. Instead of learning from missteps and strengthening the institution, we’re watching it be weakened — deliberately, in some cases, and it seems with pointless vengeance. The critics who scream the loudest treat it as if every imperfect COVID recommendation, every adjustment of guidance in real time, every policy now viewed as incorrect with 20-20 hindsight, was a betrayal and not a best effort to help us cope with this new, tricky virus.
Let’s acknowledge that perfection was impossible in the face of an unprecedented global crisis. Guidance had to evolve, sometimes rapidly. To punish the agency now is like telling tennis star Carlos Alcaraz he can’t compete in the U.S. Open because he lost in the Wimbledon finals.
Yes, the stakes were high during COVID, but nobody — NOBODY — got it 100% right.
The result? One of our most reliable public health institutions is being destroyed by non-experts in medicine and public health. People with disturbing beliefs about infectious diseases in general and vaccines in particular. And who knows what the next year or years will bring? Who will we turn to then?
For those of us who have leaned on the CDC our entire careers, watching its destruction at the hands of non-experts is not just disorienting — it’s heartbreaking, and makes me very, very sad.
August 22nd, 2025
On the Internet, Nobody Read My First Blog
Not the site’s banner, but you get the point. (AI generated.)
In 2007, during the boom in online blogging, and right before the economy crashed, a medical education company contacted me and three other ID doctors to write a blog about HIV. The pitch was irresistible — write something about HIV on a regular basis (they didn’t say what), and we’ll promote it widely. Oh, and you’ll get paid!
The lead from the company certainly conveyed enthusiasm. He made the inevitable “viral” pun (ha ha, we all chuckled politely), and unveiled a clever name. It had “expansion potential,” he said: We’ll start with this one on HIV, but later we could launch one on Oncology, Dermatology, Hirudotherapy*.
(*Leech therapy — so not really that.)
He also mentioned how much interest he’d already received from the various companies that developed HIV treatments. Indeed, they planned to sell ads once the internet traffic came pouring in. It was all very promising.
I enthusiastically signed up. Then I wrote a few pieces, none of them in hindsight very good, and sent them to the person responsible for posting them online.
It launched in the spring of 2007, including an inaugural piece of mine called “Some Non-Scientific Thoughts on CROI” where I complained about CROI holding its opening night during the Academy Awards — in Los Angeles, no less. (Yes, they did that.)
Then I waited for the flood of insightful comments. You know, Web 2.0.
The response?
It got worse from there. Reader engagement went from sparse to nonexistent. The site was glitchy, forcing people to reset their passwords for no apparent reason. You can only clear your browser cache so many times before bolting. Even in 2007, patience for that kind of frustration was in short supply.
And the design of the site? It typified the overall look of the early-ish internet — low resolution, bad colors, possibly done with an open-access graphics program by someone’s 8th grader. You want pop-up windows? We’ve got pop-up windows!
The combination of sporadic content and technical obstacles hardly created the kind of user experience to encourage participation. The site closed up shop in less than a year, a much less famous failure than Lehman Brothers, which shared a similar fate and termination date.
But despite the false start, I’m grateful to the organizers for their optimism and for getting me going — you have to start somewhere. That was the lesson I learned in hindsight. It won’t always be a success, but it’s worth putting the words on the page, even if you later cringe at the whole effort.
That’s true for any creative pursuit — painting, music, pottery, bonsai tree cultivation. False starts are still starts, cringeworthy though they may be.
Most importantly, when the NEJM Journal Watch editor Matt O’Rourke considered expanding the Journal Watch content to include blogs, I had some experience with the medium, and could send him some of my posts — now revised, reworked, and improved, of course!
(Revision is an amazing thing. Another lesson learned.)
Would I have been able to launch this effort without that initial experience? Unlikely.
And as a reminder that even the most enduring internet creations start somewhere, here’s Peter Steiner talking about his own legendary contribution to world humor — the brilliant, timeless cartoon “On the Internet, nobody knows you’re a dog.”
It started just another sketch in a pile of many, and was hardly his first try.
August 16th, 2025
Anal Cancer Screening in HIV: When Guidelines Get Ahead of the Evidence
 Should every person with HIV over age 35 (if MSM or transgender woman) or 45 (everyone else) have an anal Pap smear, a digital anal rectal exam (DARE), and possibly a high-resolution anoscopy every 1–2 years? According to recent guidelines, yes. But here’s the problem: we don’t know if this screening effort actually prevents cancer.
Should every person with HIV over age 35 (if MSM or transgender woman) or 45 (everyone else) have an anal Pap smear, a digital anal rectal exam (DARE), and possibly a high-resolution anoscopy every 1–2 years? According to recent guidelines, yes. But here’s the problem: we don’t know if this screening effort actually prevents cancer.
First, some facts:
- Human papillomavirus (HPV) infection is necessary, but not sufficient, for the development of anal cancer.
- Both HPV prevalence and anal cancer incidence are higher in PWH than in those without HIV.
- The natural history of HPV leading to anal cancer is similar to cervical cancer.
- Cervical cancer screening programs have reduced incidence of that disease.
- In the ANCHOR trial, treatment of biopsy-confirmed, high-grade squamous intraepithelial lesions (HSIL) in PWH reduced the risk of anal cancer.
So far, so good.
The temptation, therefore, is to apply our cervical-cancer-prevention model directly to anal cancer, and that’s an approach many have advocated for years. But here’s the problem — there’s no proof this works. As Dr. Hayden Andrews wrote in a recent State-of-the-Art review in Clinical Infectious Diseases (Note: I am currently editor-in-chief of this journal):
To date, no trial has been conducted to determine if anal cancer screening among PWH decreases anal cancer incidence.
And if you think about it for a nanosecond, that’s not surprising! Demonstrating that cancer screening improves outcomes is notoriously hard. Just ask anyone who studies breast, prostate, lung, or colorectal screening — and those cancers are far more common than anal cancer, and have been far more widely studied.
This gets to the core of why I believe the International Anal Neoplasia Society guidelines — later reinforced by the Department of Health and Human Services HIV guidelines — are premature and overly aggressive. They’re posted in our clinic workroom, so I’m constantly reminded of just how broad they are. The recommendations show up in this Bluesky post of mine, along with my incredulous query:
Calling all HIV/ID providers: How many are able to do this screening for anal cancer according to IANS? Including the HRA and repeat screening every 1-2 years (!!) for normal results? Wow, that's a lot of screening tests in a lot of people! #IDSky #HIVsky onlinelibrary.wiley.com/doi/10.1002/…
— Paul Sax (@paulsaxmd.bsky.social) 2025-08-15T17:39:22.614Z
Wow (again) — all MSM and transgender women older than 35? All men and women older than 45? Referral of all abnormal results to high-resolution anoscopy? Then repeat the process if normal results every 1-2 years? My goodness.
Some issues that make broad screening problematic:
- Poor test performance: Anal cytology via Pap smears has low sensitivity for HSIL even in high-prevalence populations; it also has high interobserver variability and lots of unsatisfactory or ASCUS results. Read Dr. Amit Achhra’s paper describing their experience at Yale — disappointing, both in terms of accuracy of anal cytology and patient participation! Digital anal rectal exams (DARE) can pick up anal cancer, but lack sensitivity for HSIL, the key precancerous lesions.
- Limited access to the best test: High-resolution anoscopy (HRA) is superior to anal cytology, but many clinical sites have few or even no trained providers to do the exams. I know of one site that cares for thousands of patients and has zero access to HRA.
- Patient burden: Local anaesthesia, discomfort, repeat visits, cost, and anxiety aren’t trivial.
- Unclear screening frequency: The evidence for how often to screen is even weaker than whether we should screen at all.
Add to this the medicolegal bind these guidelines create — if you follow them, you may overwhelm your local system or excessively burden your patients; if you don’t, you risk looking negligent in hindsight. It’s the perfect recipe for a frustrated group of HIV providers, as we’re doomed to fail (and we obsessive ID types hate failing). I really do wonder what fraction of us are in “compliance” with these guidelines. I’d bet good money it’s very low!
As the late David Sackett, one of the founders of evidenced-based medicine, once wrote, “the fundamental promise we make when we actively solicit individuals and exhort them to accept preventive interventions must be that, on average, they will be the better for it… Without evidence from positive randomized trials … we cannot justify soliciting the well to accept any personal health intervention.”
That’s exactly the unease many of us feel with these guidelines (and thanks to Amit for pointing me to this great quote).
I shared my concerns with Dr. Grant Ellsworth, a member of the DHHS guidelines committee who heads the HPV section, and obviously knows a lot more about this field than I do. In addition to looking forward to a time when HPV testing is routinely incorporated to reduce over-screening, he made some additional valuable comments:
Amit Achhra’s paper really highlights how poor a screening tool cytology can be. They had high unsatisfactory rates and frankly outlying poor performance — even at a place like Yale. If Yale can’t pull it off, who can? My other hesitation with the current recommendations is that I’m not sure ANCHOR’s results can be reproduced in the real world. The study sites had an onerous and expensive training process, with ongoing audits to maintain quality. Sure, we can screen for anal HSIL, but will your clinic be able to find and treat it at the same level as ANCHOR?
That last question is key — if the idealized trial environment can’t be replicated in everyday practice, then the guidelines risk being aspirational rather than accomplishing their goal.
Here’s what I’d do until we have better evidence.
- State up front that although we know that anal cancer is more common in people with HIV, we don’t know if screening helps reduce the risk over a strategy of not screening.
- Start discussions at age 50 (or younger if other strong risk factors: low nadir CD4, smoking).
- Offer shared decision-making, not automatic screening. What does the patient want? We do this with the PSA, why not this test?
- Skip the anal Pap entirely, and go directly to HRA for those who choose screening. If HRA isn’t available, focus on HPV testing.
- Repeat no more often than every 3-5 years, or some other interval to be determined by baseline risk.
This approach acknowledges that the ANCHOR trial answered only one question — whether treating HSIL reduces cancer incidence. It emphatically did not address the important questions of how to screen, whom to screen, and how often to do it.
I’m afraid answers will only come from further clinical studies.
August 6th, 2025
Does the Fact That AI Is Brilliant at Writing “Learning Objectives” Prove They’re Not Really Needed?
Paramount Pictures, 1932.
Recently, I was invited to speak at a primary care conference on a terrific topic: “Can’t Miss Diagnoses in ID for the PCP.”
Love it. So many great examples come to mind — endocarditis, Lemierre syndrome, vertebral osteomyelitis, acute HIV. A wonderful opportunity to teach about the “rare but there” diagnoses hidden among everyday outpatient complaints: fatigue, sore throat, back pain, and “mono,” respectively.
I was all in.
You know what I wasn’t all in on? The inevitable mountain of paperwork that followed. Veterans of academic medicine know what’s coming: the dreaded email with five attachments, multiple forms, and of course — the request for Learning Objectives.
First, let me remind everyone of the Universal Rule of Email Avoidance:
The likelihood of an email being answered promptly is inversely proportional to the square of the number of attachments.
Now, back to the Learning Objectives, which will occupy the remainder of this post. They’re short statements (usually three, range 2–5) that describe what the audience is supposed to learn from a lecture. Education experts say they help focus the talk and make evaluation easier. Accrediting bodies like ACCME require them for Continuing Medical Education (CME) credit. (Mea culpa: This is true even for our course, ID in Primary Care, despite this rant to follow. Sorry.) Hence their ubiquity, and the fact that every talk now asks for them.
Some excellent educators defend them as a helpful way to structure a talk. Fair enough; if they work for you, terrific. And there are numerous authorities in both written and video form on how to write effective Learning Objectives, so you can study up to your heart’s content.
(Go ahead, watch one of those videos in its entirety. I dare you. To me, they are mind-numbingly boring — but to each their own, I guess.)
But let’s not pretend Learning Objectives are an essential part of effective teaching. So much of what will be conveyed in a talk can be communicated in the talk’s title, plus (if requested) a 2–3 sentence summary. And that process of using learning objectives to organize a talk? We used to call that “making an outline.” No pre-talk submission required, no adhering to SMART criteria — which stands for “specific, measurable, achievable, relevant, and timebound,” in case you were wondering.
Fortunately, there’s now a solution: Artificial Intelligence — which has gotten so good at writing Learning Objectives that the task is now completely frictionless. I guess this is no surprise, as even in the stone age of AI (like, last year), it was great at streamlining workplace drudgery.
Here’s the prompt:
“Write 3 learning objectives for a talk called ‘Can’t Miss Diagnoses in ID for the Primary Care Provider.’”
Now watch the magic, example #1 from ChatGPT:
At the end of this presentation, learners will be able to:
Identify key clinical features of uncommon but serious infectious diseases that may initially present with nonspecific symptoms in primary care settings.
Apply diagnostic reasoning to distinguish these conditions from more common, benign illnesses through targeted history, physical examination, and appropriate use of laboratory and imaging studies.
Initiate timely management and specialist referral when these high-stakes infections are suspected, to reduce morbidity and improve patient outcomes.
Bravo. These are far better than anything I could have done, mostly because my Learning Objectives are always written with a combination of mild annoyance and the driving motivation not to let “perfect” be the enemy of “just get it done already.”
Didn’t like these ChatGPT products? Go ahead and try Gemini. Or CoPilot.
Voilà! Problem solved. These are so good, it’s downright scary. No thinking required. Copy, paste, submit. Or just send the organizers a link or generate a QR code for handy scanning.
But here’s the problem: if AI can generate them instantly — without context or understanding or board certification in Infectious Diseases — what are Learning Objectives really worth? How many people actually read them? At the end of a talk, no one says, “Wow, those Learning Objectives were beautifully met.”
Instead, we say:
Was that a good talk? Did I learn something useful? Was I engaged? Or was I bored out of my mind, checking my phone?
So I’m sticking with the view that it’s hardly ever about the Learning Objectives. Let’s stop pretending otherwise.
And a plea to the leaders of medical education: could you please — please — lighten the paperwork load for clinical teachers? That would be hugely appreciated.
Let’s close with a scene that proves exasperation with institutional nonsense in education is timeless. These guys had it pegged nearly a century ago.
August 2nd, 2025
The Short Political Half-life of a Medical Contrarian
 In early May, I wrote about the surprising FDA appointment of Dr. Vinay Prasad to lead the FDA’s Center for Biologics Evaluation and Research. Prasad is a UCSF hematologist-oncologist known for his views on COVID-19, oncology clinical trials, and his sometimes sharp-elbowed communication style, in particular directed at people with whom he disagrees. My goal was to write something balanced, and even hopeful, acknowledging both Prasad’s impressive skills in interpreting medical evidence and his well-documented provocations, at least as viewed from the perspective of an ID doctor.
In early May, I wrote about the surprising FDA appointment of Dr. Vinay Prasad to lead the FDA’s Center for Biologics Evaluation and Research. Prasad is a UCSF hematologist-oncologist known for his views on COVID-19, oncology clinical trials, and his sometimes sharp-elbowed communication style, in particular directed at people with whom he disagrees. My goal was to write something balanced, and even hopeful, acknowledging both Prasad’s impressive skills in interpreting medical evidence and his well-documented provocations, at least as viewed from the perspective of an ID doctor.
Let’s just say: not everyone loved that piece.
I wrapped up that post with this:
Ultimately, my deepest hope — and I suspect everyone’s — is that this appointment of Dr. Vinay Prasad leads to a continued focus on improving the safety, efficacy, and public trust in biologics, especially vaccines. We need rigorous science, honest communication, and thoughtful leadership more than ever.
That doesn’t sound too bad, does it? The comments I received here on this site were quite thoughtful, led by Dr. Jonathan Blum’s clever “I am cautiously pessimistic” — ha! I also got a nice note from Dr. Adam Cifu, who is a friend of Prasad’s and co-founded the interesting Sensible Medicine newsletter with him.
But, judging by some of the responses I received by email or on social media, you’d have thought I’d volunteered to ghostwrite for RFK Jr. For those who think Bluesky is the kinder, gentler social media platform, allowing only polite and balanced responses — I have some strong evidence to the contrary. Yeesh. Turns out anonymous burner accounts are nasty no matter where they post.
Now, not even 3 months later, Prasad is out. Officially, he resigned — the classic “time with family” explanation. Unofficially? He’s gone because he did what we say we want FDA leaders to do: he questioned the approval of an expensive, potentially toxic therapy with scant evidence of benefit.
And no, this wasn’t about COVID-19. Or vaccines. Or even infectious diseases.
It was about a treatment for Duchenne muscular dystrophy — a tragic and incurable disease that understandably generates passionate advocacy and whose therapies have a long track record of FDA controversy.
But after a Wall Street Journal op-ed from a non-physician critic and some well-placed accusations of political disloyalty (apparently, he’s too much of a Bernie guy now?), he’s gone. Just like that.
This raises a disheartening possibility: that both his appointment and his dismissal had less to do with his ability to interpret clinical studies and more to do with politics, all while mixing in an unhealthy tincture of conflict of interest.
That’s deeply unfortunate — because whether you loved or loathed Prasad’s presence at the FDA, one thing is clear: science-based public health leadership shouldn’t be a partisan tug-of-war. Not when trust in our institutions is already on shaky ground.
I’d like to give the last word to one of my long-term mentors, a now-retired ID doctor who held some important government positions during his distinguished career. He’s been watching this turn of events with detached amusement from his summer home, and wrote me this sage comment in a terse email:
It’s a lot easier throwing bombs at others from the outside than taking criticism coming in.
Isn’t that the truth?
And speaking of sharp thinkers who challenged conventional wisdom, and because last week I finished with a tribute to some recent celebrities who died, this past week we lost satirist-mathematician Tom Lehrer at age 97. His songs were a master class in wit, skepticism, and brainy mischief — all qualities that (whether you like him or not) Prasad might admire.
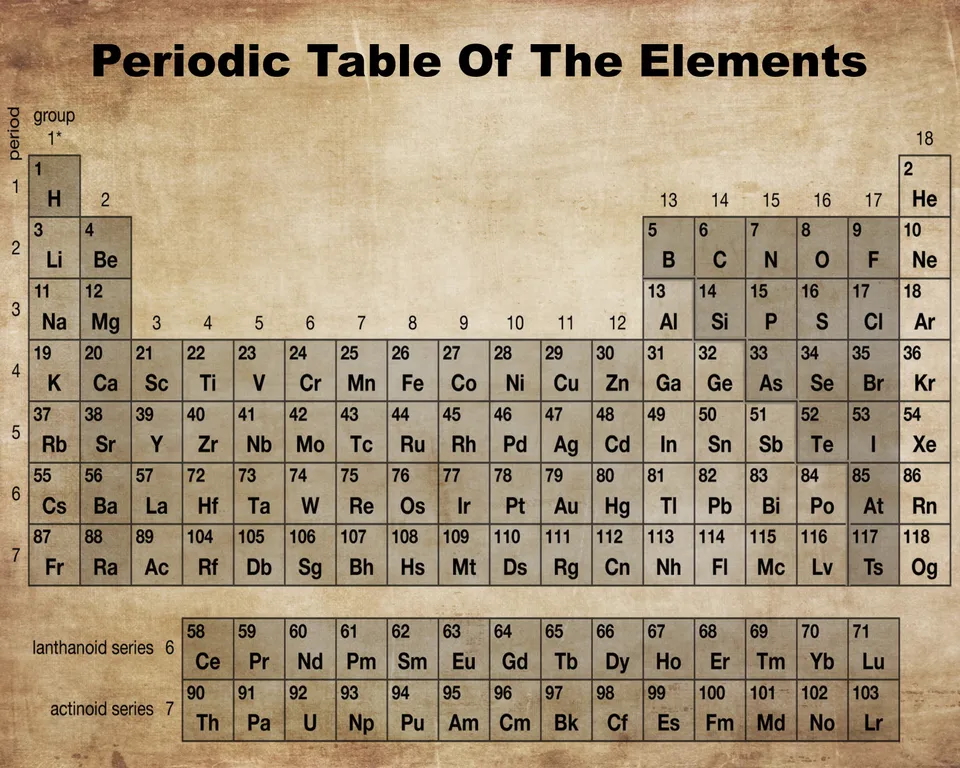
Lehrer’s work also brings back fond memories of the smartest kid in my school, my friend Jimmy P, who introduced me to these nerdy musical gems. (I was an 8.5/10 on the nerd scale; Jimmy easily 10/10.) If you’ve never seen it — or just want to be reminded how funny chemistry can be in the right context — here’s one of the all-time classics:
What a talent — even rivals Ozzy Osbourne.
July 25th, 2025
Who Gets Sent to ID Clinic? A Field Guide to Outpatient Referrals
 Sometimes people ask me what kind of cases get referred to ID doctors in the outpatient setting. Despite what the latest television series might suggest, it’s rarely suspected Ebola (fortunately) or Tsutsugamushi fever — a disease that is much more fun to say by its Japanese name than its common one, scrub typhus.
Sometimes people ask me what kind of cases get referred to ID doctors in the outpatient setting. Despite what the latest television series might suggest, it’s rarely suspected Ebola (fortunately) or Tsutsugamushi fever — a disease that is much more fun to say by its Japanese name than its common one, scrub typhus.
(In Japanese, “tsutsuga” means “hindrance” or “illness,” and “mushi” means “insect” or “vermin”. Now you know!)
Instead, the cases generally fall into one of these four broad categories:
1. Diagnostic dilemmas. The clinical gestalt suggests infection, there’s no diagnosis, and the patient isn’t getting better. You know, Box #4 of the Four States of Clinical Medicine — “No diagnosis, not improving,” the most unstable box to be in. Let’s see if our diagnostic skills can get the patient out of that box as fast as possible.
Fever of unknown origin is the classic example, but it could be a red limb unresponsive to empiric antibiotics, refractory diarrhea, disabling night sweats, or the cough that just won’t go away.
A somewhat different version of these dilemma cases (but still in this category) is the patient reporting extensive infectious exposure, and now new symptoms that could be related. If a construction worker has just returned from an excavation project in Tucson, where he oversaw trenching and grading operations (or whatever excavators do), you’d think of a certain fungal infection if he now showed up with a cough and low grade fever. Or it could just be a viral upper respiratory infection.
Closer to home, infection would be top of the list if a restaurant worker from a New England seafood restaurant had slowly growing nodular red bumps up her arm. Fun fact: the person most likely to have M. marinum isn’t your friend with the aquarium — it’s the sous chef cleaning lobsters with a Band-Aid on a scraped knuckle.
Sometimes it’s just profound fatigue after an infection — in ID, we were seeing post-infectious fatigue long before COVID-19 (after sepsis, Epstein-Barr virus, cytomegalovirus, influenza, lyme), and COVID has certainly increased that pool of unfortunate patients. Yes, many of these referrals turn out not to be active infections, or infection-related, at all — but that’s for us to figure out. We’re the “it might be an infection” people.
2. Unusual diagnoses to nonspecialists. These are infections that primary care clinicians might see only occasionally, but that land in our inboxes daily. HIV, osteomyelitis, endocarditis, tuberculosis, nontuberculous mycobacteria, prosthetic joint and other hardware infections, multi-drug resistant bacterial infections, and the full spectrum of syphilis. (Examples of this last one: secondary syphilis with uveitis, or tinnitus, or some other bizarre manifestation of this quintessentially protean disease.) Hepatitis C used to fall into this category, especially in the interferon and early direct-acting antiviral era, but now treatment has become so simple that most patients get treated (and cured!) in primary care. Still amazed at that transformation.
Vertebral osteomyelitis is a striking example of this category — rare to primary care, common to us. A busy first-year ID fellow may see more than a dozen of cases over the year on the inpatient consult service, whereas a primary care clinician will evaluate hundreds of patients with back pain over several years. But chances are good that none of them has vertebral osteomyelitis.
Not surprisingly, many of these patients are diagnosed during a hospital stay. Since most generalists today focus on either inpatient or outpatient care (not both), we often inherit these cases post-discharge after an inpatient consult.
3. Unusual diagnoses — even to us! These are the real fascinomas, the ones that earn a coveted slot in ID case conferences and elicit audible gasps, especially if there are good images.
Here in temperate Boston, parasitic infections and tropical diseases make the list, as do systemic fungi, nocardia (which straddles the line between fungus and bacterium — I hope that’s not insulting to nocardia), and various other medical oddities. Infections that were once common but are now mostly vanquished also show up, and here’s when having gray hair as a “seasoned” clinician (I wonder who that could be) is a plus. One recent example is a referral we received for a fever and an unusual pustular rash that turned out to be … varicella … better known as chickenpox.
But for many of these true rarities (not chickenpox, but rather melioidosis or leishmaniasis or cysticercosis, et al.), there are usually only a handful of true experts, and we ID doctors often act as the conduits to them. Luckily, they’re often generous with their time when we call or email. Thank you, remote consult heroes!
4. Very common diagnoses — but with a twist. Finally, the largest category. These are the bread-and-butter infections that just won’t go away, or keep coming back, or are sometimes particularly severe. Recurrent cellulitis, sometimes complicated by bacteremia and requiring hospitalization. Chronic sinusitis. Nonhealing wound infections. And leading the pack by a wide margin: urinary tract infections (UTIs).
UTIs may never make the headlines in medical mystery columns, but what they lack in novelty they more than make up for in frequency — and in misery, for the frustrated patients who suffer through them. Challenging UTIs are so common in ID clinic that we really ought to start a loyalty program. Fortunately, two of my colleagues — Drs. Sigal Yawetz and Jacob Lazarus — specialize in these cases and generously share their expertise with the rest of us.
If you’re looking for guidance on managing UTIs, you’re in luck: two outstanding new publications have just come out to help clinicians navigate both recurrent and complicated cases:
- A State-of-the-Art review on Recurrent Uncomplicated UTIs in Women, published in Clinical Infectious Diseases.
- A comprehensive IDSA Guideline on Complicated UTIs, which includes my colleague Sigal on the panel.
Each comes with practical tools, evidence-based recommendations, and at least one flowchart you’ll find yourself referring to again and again — whether you’re in clinic or on the wards.
Wow, quite the week for deaths of some notable celebrities from my youth and young adulthood — Ozzy Osbourne, Hulk Hogan, Chuck Mangione, Malcolm Jamal Warner (particularly sad, given his age). I can’t say any of them was a particular favorite, though of course I knew of them all, with Chuck Mangione’s “Feels So Good” playing on perpetual repeat during my senior year of high school.
Who to feature here at the end of this ID blog? I’m going to go with Ozzy, in honor of the self-awareness he developed later in life (especially on the reality TV show he did with his very appealing wife Sharon), and as a gift to my mother, who turns 91 today. She loved his music.
That, my dear readers, is sarcasm. Happy birthday, Mom!
July 17th, 2025
Ceftriaxone Is a Narrow Antibiotic Now — and Other Musings
Mather and Company, 1929.
In no particular order, 20 things I’ve found interesting lately — a mix of ID (mostly), language quirks, clinical stuff, even tennis, and an apology (#21) at the very end. Bonus videos embedded because we all need a break.
1. Isn’t it amazing how, over time, an antibiotic once considered “broad spectrum” later becomes the drug we use after the term “narrowed?” Example: “He was on meropenem, but his cultures came back with just Strep mitis, so we narrowed him to ceftriaxone.” Fair enough — it’s narrower than meropenem — but it’s crazy that ceftriaxone is now a “narrow” antibiotic!
2. Someone who has scant knowledge about healthcare — but has nonetheless risen to a position of power and influence — said that “50 percent of revenues to most pediatricians come from vaccines.” What the …? You might as well say that they get the other 50% by charging for the stickers they hand out at the end of the visit. In fact, pediatric practices take on financial risk and incur high up-front expenses to have vaccines available; for some, providing and administering vaccines can lose money.
3. On the topic of pediatrics, childhood hospitalizations last year from mycoplasma did indeed sharply increase, accounting for half of hospitalized children with pneumonia. We also saw way many more cases in adults, including many with those strange non-respiratory presentations (rashes, neurologic disorders, hemolysis). While cyclic variations in mycoplasma incidence are expected due to waning immunity, this past year saw a bigger increase than usual.
4. I’m not gonna lie — it has always amused me that many people (including me!) highlight certain comments with, “To be perfectly honest…” What does this imply about when we don’t say this? That we’re not being honest? And yes, “I’m not gonna lie,” “truth be told,” “truthfully,” and the rest of the bunch all fall into the same category.
5. A patient I’ve been following for years had a CD4 nadir of 3 at the time of their HIV diagnosis in 2010; it’s now over 2000, an astounding increase. Meanwhile, a similar patient I saw recently has had virologic suppression for almost as long, and the absolute CD4 count still can’t quite crack 100. This variation in immune response to antiretroviral therapy is one of the unsolved mysteries in HIV medicine.
6. Learned recently that pair of words that is used in a fixed order in an idiomatic expression is called an “irreversible binomial.” You know — wet and wild, mac and cheese, wear and tear, rock and roll. The first ID one that came to mind? Glucan and galactomannan — fungal diagnostics aficionados will agree, no one says it the other way
7. The continued universal susceptibility of Treponema pallidum and group A strep to penicillin remains a great gift to humankind, one we should be grateful for every day.
8. We complain about electronic medical records a bunch, but let’s face it — they have made a whole lot of things better than back in the pre-digital age. Near the top of the list? The ability to review radiographic studies without having to trek to a reading room, where the films may or may not be available. It’s especially great since we can now use Teams or Zoom to review the images with our radiologists, with them highlighting the areas of greatest interest.
9. How does anyone ever learn English?
10. We’ve had BCID (Blood Culture Identification) testing in place for around a year now; it rapidly identifies the bacteria in positive blood cultures, and tests for genetic determinants of common resistance mechanisms, too. Trust me — once you have this in place, you can’t imagine ever going back.
11. Even a year after my rant, and over a decade since generic tablets hit the market, some clinicians still think linezolid is too expensive. That’s because patients go to pharmacies, get told their insurance won’t cover it, and aren’t told they can just pay out-of-pocket at a reasonable price. Even worse, one large chain still charges a crazy high price, presumably for the branded version. Because they can? It’s madness.
12. I used to pride myself on knowing all of the FDA-approved cephalosporins, including obscure oral formulations. Confessing right here that the blizzard of recently approved and late-stage compounds (most of them cephalosporin-beta lactamase inhibitor combinations) has challenged this party trick. Let’s see — there’s already ceftazidime-avibactam, ceftolozane-tazobactam, cefepime-enmetazobactam, and cefiderocol; coming soon will be cefepime-zidebactam and cefepime-taniborbactam. Wow.
13. By the way, in addition the cephalosporins, I can also name the fluoroquinolones that were withdrawn due to safety issues — temafloxacin, sparfloxacin, gatifloxacin, grepafloxacin, and trovafloxacin. Branded Zagam, Trovan, Raxar, Tequin, they sounded like action figures fighting it out in an animated science fiction movie. Fun times!
14. Which reminds me: A resident recently told me they couldn’t go into ID because it required “too much memorization” — antibiotics and microbiology, specifically. My reply: it’s not like you become an endocrinologist by spontaneously deriving the hormonal feedback loops. Every specialty has its learning curve. Memorization follows interest.
15. Since the topic of party tricks came up (Name that cephalosporin! That discontinued quinolone!), I often find myself watching videos of card tricks with amazement, admiring the talent of people with a large repertoire. This guy, who says he has a million such tricks, is my favorite of many such magicians — something about his very regular-sounding voice makes him tremendously appealing:
16. Since those were Keith Haring playing cards — you noticed, right? — I must cite that IAS 2025, the 13th IAS Conference on HIV Science, happened this week in Kigali, Rwanda. Not surprisingly, there were several presentations on disruptions in patient care resulting from recent policy changes and budget cuts by the USA — disruptions that will lead to more HIV infections and more HIV-related deaths. Sad to see this proud chapter in U.S. foreign policy come to an end.
17. The letters to the editor at NEJM protesting the Sounding Board written by Drs. Vinay Prasad and Martin Makary on vaccines for COVID-19 make fascinating reading, as does Prasad’s and Makary’s response to the correspondence. It’s remarkable how a group of intelligent, experienced, and well-meaning people can look at the same body of evidence in medicine and come up with starkly different interpretations. I think both sides having valid points.
18. Related, what I’d really like to see is Prasad — who is a strong advocate of evidence-based medicine — take aim at some of the quite outlandish statements we’ve heard about the epidemiology and causes of autism, or the perils of seed oils. Hey, why not? He’s never been shy about voicing his opinion in the past.
19. My favorite new phrase mobilized by our ID fellows when coming up with a treatment plan for an ID consult? Course it out. “He’s improved on cefepime day 3 empirically for pneumonia; I think we can course it out with 4 more days and sign off.” Love that phrase — “course it out” — now a part of our service lingo. Plus, 3+4 = 7. Because of course it does.
20. Congratulations to Jannik Sinner, who blitzed his way past Carlos Alcaraz in this year’s Wimbledon final, as well as Iga Świątek, who “bageled” Amanda Anisimova, 6-0, 6-0. But the best single point of the competition? I’d give the nod to old-timer (38!) Novak Djokovic who, on his way to a semifinal finish, pulled this one off in an earlier round:
21. I was hard on Djokovic in the past when the guy refused to get the COVID-19 vaccine, comparing him to a bully athlete from my school days, but he has really grown on me. In my defense, the world was crazy those first 2 years of the pandemic; I wasn’t always so tolerant. Which is why I was delighted to read a piece entitled Novak Djokovic, I Was Wrong About You, as it summarizes my current views on him perfectly.
So my apologies, Novak!
July 12th, 2025
The Patient Did Well — So the Insurance Company Won’t Pay
 Sometimes, you can predict a bad outcome. Examples:
Sometimes, you can predict a bad outcome. Examples:
- Proposing marriage after an awkward first date — and doing so over gas station nachos.
- Moving to a Cambridge apartment with no off-street parking, then buying a Tesla Cybertruck.
- Trying to recruit for ID fellowships from a group of cosmetic dermatologists.
But predicting what happens in clinical medicine? Not so easy. Which is why the clairvoyance expected by certain health insurance companies baffles the mind — they seem to believe we can diagnose, prognosticate, and determine outcomes with the omniscience of the Oracle of Delphi.
Take this recent gem. I’m sharing it here not because it’s unusual, but because the absurdity deserves a moment in the spotlight.
(Part of a series.)
Here’s the scenario (some details changed to protect privacy):
The patient, a 64-year-old man, went to our emergency room with fatigue, acute kidney injury, and a hemoglobin drop. He’d recently undergone gastric sleeve surgery, making the clinical status more uncertain than usual — plus a background of diabetes and high blood pressure as medical comorbidities. Given the symptoms and risk factors, he was admitted to medicine for hydration, monitoring, and endoscopy. He got better. We all celebrated. Cue the credits.
But then… the sequel. (Spoiler alert: It’s a horror film.)
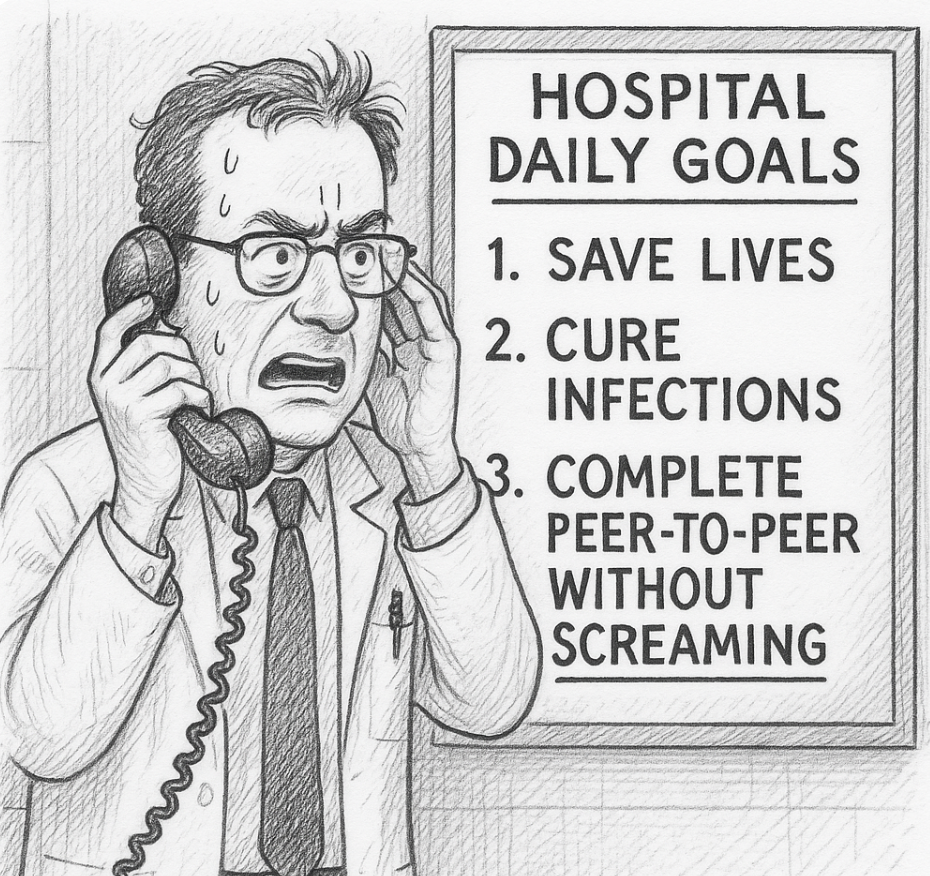
A few days later, I received an email saying that the insurance company had denied inpatient level of care — in plain English, they didn’t want to pay. Would I have time to do a “peer-to-peer” discussion to try and reverse the decision?
They might as well have asked me to call an airline to rebook a cancelled flight during a massive Nor’easter, that’s how much I was looking forward to this task. But given how justified the admission was, and my trying to be a team player to defend good clinical practice in the face of our Private Insurance Overlords, I set up some time to talk with my “peer.”
I use quotation marks because while I’m sure she was, technically, a healthcare professional, her role in this drama felt more like prosecutor than peer.
She had some of the hospital data. Not all. Enough to cherry-pick to support their refusal to pay, but not enough to understand the full context of the case since, of course, she had never seen, spoken with, or evaluated the patient.
She asked me a series of questions, some of which were about information she already possessed, as if hoping I’d contradict myself like a suspect in a police procedural. (“So you’re saying the patient had a drop in his hemoglobin during the hospitalization? Interesting, doctor… very interesting. I see here it remained 7.5–8.3 during his stay. Do you consider that a drop?”)
I explained, again, the patient’s presentation. The drop in hemoglobin from his baseline of 10.5. The post-bariatric surgery. The concerning acute kidney injury in someone with diabetes, hypertension, and obesity. You know — the reasons why he was admitted.
But then came the decision, delivered with the cool finality of a game show host eliminating a contestant. Because the patient had no hemodynamic instability during his stay, and no ongoing bleeding, the hospitalization was deemed… unnecessary.
Denied.
“I cannot overturn the decision,” she said, as if quoting some higher order of evidence from randomized clinical trials rather than a faceless algorithmic edict she no doubt had up on her screen as she was talking with me.
I took a deep breath.
Then I asked her to imagine herself as the patient — sitting in the ER, post-recent surgery, with those symptoms and those lab results. Or better yet, as the clinician doing the initial assessment, deciding whether to admit or to send him home.
Would she have discharged this man? Would her judgment have changed if she weren’t now on the payroll of Giant Healthcare Insurance Company? Had she, like so many burned-out clinicians, left clinical medicine because of pointless, time-wasting demands like this conversation — only to end up perpetuating the same dysfunction from the other side?
No answer. Silence on the other end. Then, she repeated, “Thank you, Dr. Sax for your perspective. I cannot overturn the decision.”
Because of course, the outcome — the good outcome — was only apparent after the fact. One reason to admit people is when we don’t know if they’ll do well.
So yes, the patient got better. No, he was not critically ill. But that’s not evidence the admission was unnecessary; that’s evidence the admission went about as well as could be hoped. Isn’t that what we all want?
Unfortunately, our healthcare system now seems to reward retrospective omniscience more than clinical judgment. “If only you had known he wouldn’t bleed again!” they say. Right. And if only I had known to buy Nvidia stock when it first went public in 1999.
I’ll stop now — time to call my airline because my flight has been canceled due to an unexpected mid-summer blizzard. Should be more fun than this call.

