An ongoing dialogue on HIV/AIDS, infectious diseases,
April 28th, 2023
What is the Future of HIV Primary Care?
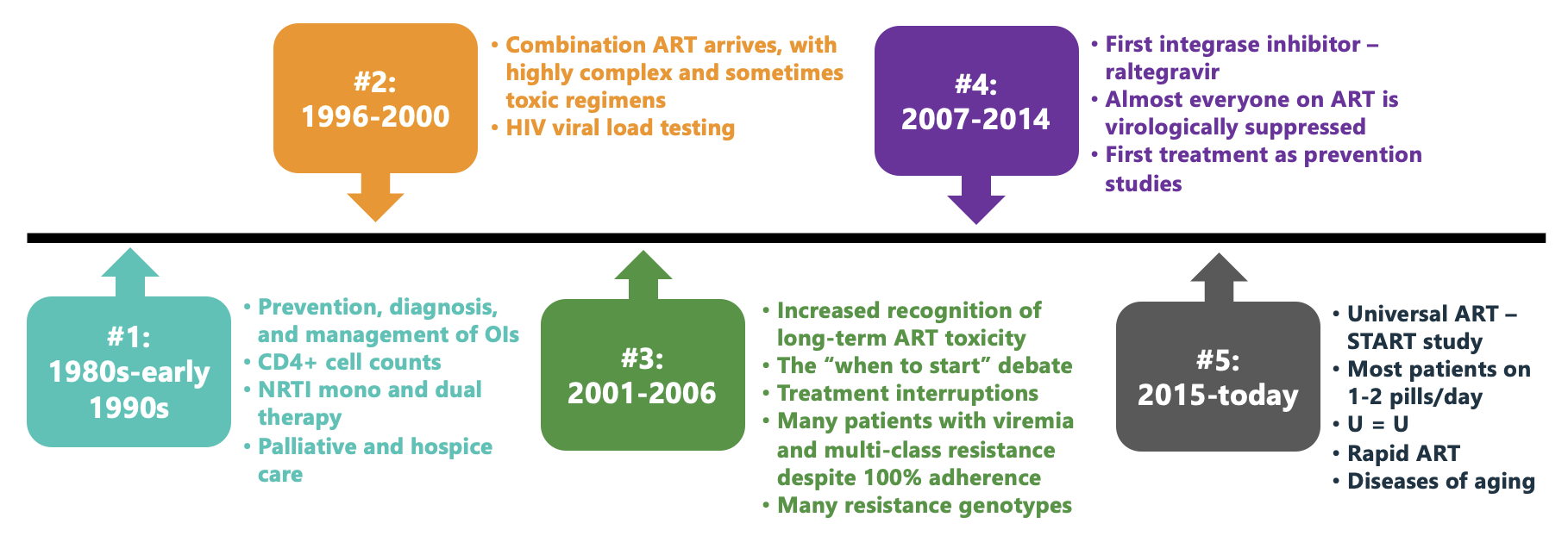
Here’s a figure I’ve made for an upcoming talk, which is entitled “The Future of HIV Care.” It summarizes several eras in HIV treatment, finishing up with the current unprecedented successful phase where most people with HIV take 1–2 pills a day, have virologic suppression and no clinically apparent immunodeficiency. HIV is often the least of their medical problems.
To put this into context, a patient at our hospital recently found out that the cause of their several months of fatigue and weight loss was HIV, and expressed relief that it wasn’t diabetes or cancer. And on hearing this comment, all the people on our HIV treatment team agreed that the management would indeed be easier, and more likely successful.
I don’t mean to diminish the potential severity of HIV, which of course can, undiagnosed and untreated, still be lethal. Far too many people in this country with HIV are either undiagnosed, or diagnosed and not engaged in regular care or treatment. Getting them on therapy remains an urgent individual and public health priority.
But for those in care, as an example of medical progress, HIV treatment stands out as a phenomenal success.
This success begs the question, once again, of the role ID specialists should play in the management of people who have HIV once they are on stable ART. When I last covered this topic here on this site nearly a decade ago, we were in the tail end of Era #4 above — and since then treatment has only gotten better.
For emphasis, I still believe ID doctors and HIV specialists should play a primary role in handling new HIV diagnoses, managing opportunistic infections and other complications, interpreting resistance testing, and helping guide treatment switches, especially as new options arise. The nuances of figuring out the best candidates for long-acting cabotegravir-rilpivirine certainly have put a recent premium on our expertise.
But the stable septuagenarian on one-pill ART whose major problems are hypertension, osteoarthritis, and, yes, type 2 diabetes? Who among us can claim that we’ve kept up sufficiently with these non-ID issues to be their ideal primary provider? If you, as an ID specialist, were given the option of attending an educational session from a brilliant speaker on “Advances in the Management of Invasive Fungal Infections” or “Advances in the Management of Type 2 Diabetes,” which would you choose?
We should not give up HIV care, but potentially shift it to be handled more like other medical specialties. Oncologists and rheumatologists, to cite two examples, play the dominant role in their respective diseases when treatments are active and monitoring is intense. But neither specialty takes on full primary care once the patients are rock-solid stable.
Pushing against any such distribution of HIV care to generalists is that most (importantly, not all) of the primary care workforce hasn’t been doing very much in HIV management. It’s notably concentrated in a very small fraction of U.S. clinicians. As an example, a patient of mine recently was told by their PCP that they wouldn’t order their routine monitoring tests — CBC, comprehensive metabolic panel, and HIV RNA — because “only ID can do that.” This is of course an extreme example (and certainly not true), but the anecdote shows how far from HIV general practice is for most people doing primary care.
Another important perspective comes from our patients, some of whom we’ve followed for decades. They may not be comfortable switching primary care, especially with a disease that still sadly confers some societal stigma.
So let’s re-do the poll and see what you think. As usual, I very much welcome in the comments section your opinions about this issue — and will select a few choice views for the talk!
Thank you.


It would be great to see/hear your “The Future of HIV Care” talk! Will it be a webinar available for registration?
Dr Sax observations as always are both interesting and fascinating.
I am quite saddened and a little bit surprised at the initial response where 71% of ID physicians believe it is time to move on and delegate HIV care to “ generalists “ . No one knows more about HIV infection and care of HIV infected persons than an ID physician . A generalist physician will not be able to recognize the subtle symptoms or lab data which may indicate an HIV person is not a stable as the data may otherwise suggest . That is the reason that we, ID physicians are who we are , to be able to “ see “ what other non ID physicians wouldn’t be able to see till it is too late .
I believe this attitude is a reflection of the “ malady “ which is now destroying medicine in America , where in cities like Louisville ,KY , where i live , 100% of ID physicians are either employed by a hospital or at the local medical school. I believe the same is probably true in most USA cities. It is very , but very disturbing . Somehow i always thought , we ID physicians were different in our concern for patient care.
As a family practitioner and ID specialist (sadly still less than 10% of ID specialists in my country) I can comment that this is what we have been waiting for. With so many procedures being performed on an outpatient basis, if not in community settings, it is high time that we actively encourage family medicine specialists to qualify in Infectious Diseases.
They will then be able to act as the link between hospital-based ID service and the community “generalist” – often a specialist in Family medicine.
The HIV patient dilemma is one of many which could be handled by Community-based ID specialists.
Read the question carefully. It is about primary care, not about managing HIV. Even in stable cases, everyone agrees an ID specialist should be monitoring it.
I think it’s a partnership between myself (an ID doc) and the PCP. As my patients get older and have more comorbidities, they need a great dedicated primary care physician.
I do my best, but it’s a disservice to them to not give them an excellent primary who will help me ensure my patients are up to date with all their health screenings & carefully manage all their comorbidities.
How about flipping this around? View family practice/internal medicine as a specialist.
ID specialist continues to care for HIV patient on a long-term basis, and refer the patient to Family Practice/internal medicine (not Endo or cardio) when, for example, questions about DM or HTN arise?
Great idea! Is it done anywhere like that?
Paul
Yes! Totally agree primary care is a specialty unto itself, though people don’t treat it as such.
Hi Paul –
I would not want to deny any ID specialist who embraces their inner Internist and does primary care along with HIV care; whoever keeps themselves up to date so they can deliver integrated HIV and primary care is in my mind very welcome to do so, as patients undoubtedly appreciate it. That said, as you recognize, HIV long ago evolved to a point where motivated PCPs who learn HIV primary care (i.e. everything but choosing/changing ART and managing OIs) have been able to do this same kind of integrated HIV and primary care that patients love. We’ve been doing it for years in FQHCs with Family Medicine MDs, DOs, NPs and PAs who are supported by Family Medicine HIV specialists whenever that next level of expertise is needed. It is a powerful way to destigmatize HIV and provide excellent care in the patient’s medical home, close to where they live and with the cultural competency and active case management that FQHCs are known for (particularly those with Ryan White programs). We absolutely still need ID docs in HIV medicine, but as ID struggles to maintain its ranks and HIV prevalence steadily rises, primary care providers need to step up and take a more prominent role in managing those majority of stable and uncomplicated cases and train others who wish to become HIV specialists themselves (I am in fact waiting for a flight to the Society of Teachers of Family Medicine annual conference to promote that very message!)
The stable patient can see both doctors.They could schedule an annual wellness visit with their pcp and also an annual visit with their ID doc.These visits could be spaced 6 months apart.The 2 docs could touch base from time to time.If any health issues arise the pcp would defer to the ID doc on all matters HIV and the ID doc would defer to the pcp for everything else.
I think the answer should be yes, and yes, and yes. Yes – ID should continue to manage HIV primary care, as should primary care providers, as should public health STD clinics, as should pharmacists. Our US healthcare system is too complex and broken to have only one level of clinical care take on the bulk of responsibility for this important patient care and public health intervention.
Wish there had been an option C – Hybrid model or Both.
In reality, as an ID doc, I still see legacy patients or ones that I have known for a decade-plus, but the majority of the new and chronic care is done by the NP and PharmD. This also allows me to focus more on the hospital and ICU ID.
I miss clinic HIV care, but as Dr. Sax says, it becomes primary care after the first few visits.
I would warn; however, the delusion that primary care will add HIV to their already overpacked plates is ludicrous. They are looking for ways to offload the 5,000 patient panels they have and the back-breaking amount of emails and inbox chatter.
ChatGPT to the rescue. As the recent Jama article shows, it is already better at some responses, and over time it will get better and better.
Maybe there should have been an option D – AI/ChatGPT10
Paul,
Thank you once again for stimulating an interesting discussion.
I do not believe this is a “straight forward” yes or no question. We, as long-term HIV care providers (and some trained as Internists, who practiced IM for several years), would be comfortable providing most primary care for our HIV patients. We do have the advantage of knowing our patients very well. As others have stated, some of our older patients do not want to see be referred for primary care.
However, like any good physician, we need to know when we are “over our heads” with challenging patient care issues. The example of diabetes is a good one. I, like many others, cannot keep up with the various forms of insulin, oral agents and such. I would not want to start dofetilide for a patient or attempt to determine the proper chemotherapy regimen. We do need the assistance of our colleagues in other areas.
Refer when you realize you need more for your patient than your knowledge allows you. Know your limits.
We also need to realize the number of ID physicians and HIV care providers is not expanding as rapidly as needed. Some have retired and many of the early HIIV care providers are “reaching their lifespan” in HIV care. We may need to consider maximizing the expertise we can provide patients with through our ID and HIV training and seek assistance for other care.
Perhaps these are not answers but considerations as we contemplate the ever-expanding health care options and the best care for our patients.
Thank you
Al Taege
I have been an HIV PA for almost 17 years and I think PAs and NPs in HIV clinics can continue to help close this gap. We are able to provide primary care for HIV patients and I believe that we can continue to be well utilized in this capacity. I also agree with the commenter above who stated that primary care does not have the capacity to absorb HIV care, no matter how stable the patient is. In our FQHC we have come up with a design where interested primary care/family medicine providers can see an HIV panel if they are interested and engaged in keeping up with changing guidelines and treatments. But to try to add HIV care to an already overwhelmed field is much to ask. Thanks
It’s likely insurance will require soon that PCPs manage HIV as well. They already manage CAD, DM, cancer follow-up et c. Insurance only has to pay one preventive RVU to manage all of the patient’s multiple conditions and 10s of medications vs all the EM codes it would generate seeing specialists.
Paul,
primary care practitioners are often even in shorter supply and struggling to maintain their morale even more than ID specialists so I think the answer depends on the patient and the local situation (ID in short supply ample primary care then more shift to the latter for example), Having a long standing relationship with patients is one of the joys of the practice of medicine. Having helpful and available specialists is often the means to help keep up quality for other conditions (ie diabetes). That being said, our diabetic clinic is swamped . In our HIV clinic we have been utilizing more MP/PAs/Pharm Ds as a part of the patient care team which is a hybrid approach mentioned by others. The ID fellows rotating in clinic seem to immensely appreciate both the ID/HIV expertise provided by the experienced HIV specialist as well as the in-clinic availability of the other team members.
Good discussion Paul!
Keith Henry
As a Family Practitioner who started and ran a Ryan White Funded, CHC based HIV clinic for 30 years I think the model of comprehensive patient care we all developed likely provides both the best specialty and primary care in the country. Ryan White funding provided us the time and the ancillary support to deliver superb care. My CHC colleagues were envious of the time we had for patients and the support we had as well.
Our goal should be to raise the floor not lower the ceiling.
Marshall Kubota an early FP HIV expert predicted decades ago that someday HIV therapy would be so good that everyone would be able to do it. We may be there there now. But, however potent our therapies, we still are falling short when we look at the national clinical cascade. I think the model needs to shift. I think we need Ryan White Funded Centers of Excellence that provide expert comprehensive care of complicated HIV-infection/OI’s etc but also actively support large numbers of community providers willing and able to care for less complex, stable HIV infection AND retain those patients in care.
Many ID doctors are hitting retirement age.
Long term patients like myself are choosing our primary care practices on cost and locality.
The more important point here is the role of outpatient HIV programs. The benefit of the expansive focus on social determinants of health cannot be overstated. Ryan White Programs have superior outcomes in engagement, retention and viral suppression. This is not a result of physicians who know how to prescribe one pill daily, or how to order viral loads every 6 months. The success of these programs is the multidisciplinary approach, with a focus on social issues, as well as cultural competence, and the ability to create a welcoming environment to many who would otherwise be marginalized in our health care systems. These programs are also probably best situated to provide prevention and sexual health services to a broader population.
I am intrigued by the “shared” care model mentioned above, where a primary care provider is involved in the care of patients with complex comorbidities.
Thank you very much, Dr Sax, for your always wise view.
I have to say that the discussion is very much centered in US. If you open your scope, and come to Europe (which is very heterogenous, I agree), maybe the situation is different,
In Spain, HIV care has been centered from the beggining in ID departments, in hospitals. Many of us, who care for PLWHIV have been in the ground since the late eighties of the previous century (OMG!), when we were the only people to care for them, and for many patients we have been the only doctors (…and nurses, and psychologists, and social workers, and drug addiction physicians, and family planners, and…). Now, more than 30 years later, when their HIV infection is very well and easily controlled, we care for their many comorbidities (…at the end we are also Internal Medicine specialists before ID, and we have also the help of other specialists), and it is very difficult for them to rely in other doctors. Of course, we send them to thier PCP for many complaints that they can solve, but unfortunately the Primary Care is very much stressed in our country just to “transfer” our thousands of patients to them.
For the new diagnosed patients, I think that our experience is also unvaluable, not only in the scientific field, but also in the emotional.
Having said that, we also have to do PrEP, new drugs clinical trials, clinical research, medical students and residents teaching and any other ID care (…yes! prosthetic joint infections, endocarditis, COVID, as some examples…).
My major concern is not if HIV care is going or not to Primary Care but if we are going to have what I call “generational relay”. And here we have a great problem, because I don’t see that the new Internal Medicine or ID specialists are interested at all in HIV.
Thank you again, Dr Sax, for all what you give to us.
Antonio Antela, MD, Ph D. Santiago de Compostela, Spain.
Lots of great points here. The reality I’ve found in our area (mid-sized city with a large, populous, rural catchment) is that there is a DIRE need for good primary care and that most PCPs around here cannot manage anything remotely complex in any specialty because they’re being asked to see excessive numbers of patients. By maintaining our practice as a specialty practice where we manage HIV with several embedded key services (colposcopy, anoscopy, gender affirming hormone therapy) we are able to have longer visits with our patients and manage their primary care as well. We opted to recruit a family med physician and train them to become an HIV expert in order to improve our ability to stay on top of complex primary care related concerns.
I agree with many of the above people that primary care is already swamped, and that this should be dependent on regional down to individual factors. One of those factors should be whether the HIV specialist is willing to keep up with primary care management topics. If they aren’t, they shouldn’t do work they aren’t qualified to do. It’s an insult to primary care to think you can do their job without having attended a relevant conference in the last decade.
The hard thing is that HIV affects so many primary care topics (like CV and cancer risks and vaccine schedules) so there needs to be good collaboration. Alternately, the main pathways for getting information in primary care need to start including HIV in their risk factors like they do for DM or smoking. That would also go some way to normalizing the idea of HIV being present in the general population.
Patients having both a PCP and an HIV specialist has been the model in our system all along, and it works well. It was set up this way because we have few ID docs, and patients had primary care in many different systems.
There are some hiccups, tho, such as when the PCP and ID are not in the same medical record system– we have no idea what vaccines the patient has gotten, and getting lab results can be a chore.
But I feel that the patient gets better primary care this way, and I still oversee their HIV care. And in this era of a shortage of HIV docs, it makes a lot of sense.