An ongoing dialogue on HIV/AIDS, infectious diseases,
February 12th, 2018
Shingles Vaccine Video, New Name for C. diff, Flu B Rising, and More — A Pre-Valentine’s Day ID Link-o-Rama
With Valentine’s Day and early spring training baseball both on the horizon this week, it’s obviously time for an extra special ID Link-o-Rama.
On to the links, with a bonus non-ID section and a highly recommended video at the end:
- The ACIP issued its official recommendations for herpes zoster (shingles) immunization. Preferred: the new recombinant zoster vaccine, abbreviated RZV, for people 50 and older. They do not recommend it (yet) for immunocompromised individuals — stay tuned. Does the recommendation include our stable, on-therapy HIV patients, who in increasing numbers are over 50? I say “Yes.”
- The new zoster vaccine is very “reactogenic.” Pain and swelling at the injection site, malaise, generalized aches, symptoms sometimes bad enough to interfere with daily activities. The incidence of these side effects is much higher with RZV than with the live virus vaccine, presumably due to the adjuvant that makes it so immunogenic — and effective. Warn your patients! And as noted above, I strongly suggest all clinicians watch the video, which is embedded at the end of this post — it’s highly informative and useful.
- CDC has issued dietary advice for Valentine’s Day. I’m a huge fan of the CDC, the people who work there, and the excellent work that they do. But boy, this link is no fun at all.
- Multiplex respiratory panels face off in a head-to-head study. Isn’t it extraordinary that we can make a definitive diagnosis of what causes respiratory infections with a single nasopharyngeal swab? Nineteen different pathogens in this particular panel. The key to getting these tests more broadly adopted is decreasing the cost of implementation. Nonetheless, this approach is (in my opinion) the future, especially from a hospital infection control standpoint — even though for most of these viruses, there is no available therapy.
- In this terrible flu season, should we be choosing one type of flu vaccine over another? In the absence of head-to-head trials, it’s difficult to make an official endorsement. But as this interesting piece notes, there are differences between the available vaccines, differences that may lead to different rates of protection. Credit to Helen Branswell, a local journalist who has done superb reporting on the flu this year.
 As the flu season progresses, a higher proportion of cases are due to influenza B. Our local surveillance data mirror this national trend. Good news for those of us who have been vaccinated, as the vaccine appears to be more protective against influenza B than H3N2. And if you haven’t had your vaccine yet, it’s not too late — and please, don’t listen to this advice!
As the flu season progresses, a higher proportion of cases are due to influenza B. Our local surveillance data mirror this national trend. Good news for those of us who have been vaccinated, as the vaccine appears to be more protective against influenza B than H3N2. And if you haven’t had your vaccine yet, it’s not too late — and please, don’t listen to this advice!- More testing for C. diff artificially increases the rate of diagnosis. Nucleic acid testing for C. diff identifies carriers as well as people with the disease — hence the more we test, the more non-disease cases we “diagnose.” This finding is important, as healthcare associated infections such as C. diff are a major hospital quality metric. (Note I avoided writing the full first name of C. diff, very much intentionally as a protest about the discouraging news in the next link.)
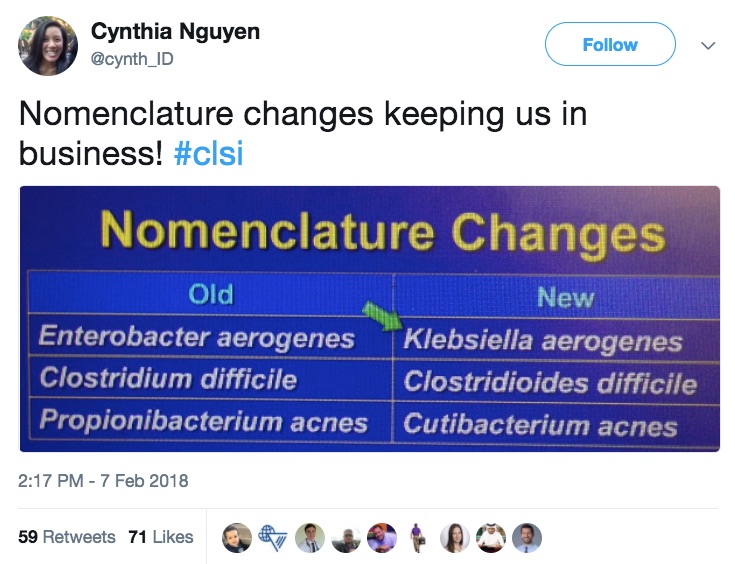
- Clostridium difficile is now Clostridioides difficile. So says the Clinical and Laboratory Standards Institute (CLSI) in an update issued last week. If that’s not bad enough, Enterobacter aerogenes and Propionibacterium acnes also have new names. Sigh. I remember when Stenotrophomonas maltophilia was Xanthomonas maltophilia, those were the days. And whatever happened to Xanthomonas, anyway? Loved that word.
- FDA approves bictegravir/FTC/TAF for initial and switch HIV therapy. Now come two inevitable questions: 1) When will my patient’s insurance/ADAP/etc. cover it? 2) Who came up with that brand name? Biktarvy, jeepers.
- Elsulfavirine, an investigational NNRTI, is also approved for HIV therapy. OK, OK, so it’s approved in Russia, not here. Here’s a clinical trial comparing it to efavirenz from last year’s CROI.
- Adjunctive rifampin does not improve outcomes in MSSA bacteremia. Important negative randomized clinical trial. Although better approaches to this life-threatening condition are needed, imagine if this became standard of care — the drug interaction challenges would be nightmarish.
- Rabies immunizations given in U.S. emergency rooms can be shockingly expensive. Since the ER is where most people go after possible rabies exposures, this cost is an important barrier to a lifesaving intervention. Another excellent example of how our byzantine and opaque healthcare “system” (I use the word loosely) can lead to outrageous charges — the patients are the ones who suffer.
- Streptococcus pneumoniae as the cause of community-acquired pneumonia continues to decline. It’s gone from over 90% in the pre-antibiotic era down to 10–15% today, a remarkable drop attributed mostly to immunization practices. Higher in Europe, where pneumococcal vaccine used less often. Great figure here.
- In a prospective study of community acquired pneumonia, clinical symptoms did not predict etiology or outcome. Seems that the “atypical” in “atypical pneumonia” applies only to the extra-pulmonary manifestations of Mycoplasma (e.g., rash, hemolysis, neurologic disease, et al.) — which are very rare.
- A brief course of empiric antibiotics in the ICU does not appear to cause harm. The study suggests this “just in case” administration of broad spectrum therapy is fine, provided treatment is stopped when cultures are negative, or narrowed once a pathogen emerges — a good role for antibiotic stewardship teams.
- Invasive dental procedures may be associated with a significantly increased risk of streptococcal prosthetic valve endocarditis. The statistical acrobatics done in this complex cohort study notwithstanding, the results suggest a fraction of endocarditis cases are attributable to invasive dental work. The study furthermore found no protection from prophylaxis. However, given the limitations of the observational design, this should not change our practice — prophylaxis for this high-risk group is still indicated.
- More evidence that cefazolin is safer than anti-staphylococcal penicillins. In this meta-analysis of 14 studies, the point estimates all favored cefazolin. It’s unlikely anyone would fund a randomized clinical trial, but that would be most welcome. For now, I am switching patients from oxacillin to cefazolin as soon as bacteremia clears.
Ok, non-ID section — a few medical, one not medical at all.
- Here is a brilliant summary of how doctors assume predictable roles when discussing “code status” with their patients. Several recognizable types here. We can all learn something about improving our approach with this difficult conversation.
- This American wanted narcotics after her surgery in Germany, but all she got was herbal tea. Congratulations to the author for adopting the perfect tone in this very funny commentary — one that says quite a bit about how we ended up in such a mess with opiates in this country.
- Medical students forced to use fax machines are perplexed by this ancient technology. That headline reads like an Onion piece, but it’s true! And when I first wrote about this anachronistic practice over 4 years ago, never did I think it would remain so firmly entrenched in how we communicate. Is there no end in sight?
- A person is ranking all 205 Beatles songs. This effort joins prior similar lists, like this one, of 213 songs — about which I have major disagreements on his rankings. This time the anonymous author is posting a new one almost every day, which adds to the fun. For Beatles fans, be warned — a huge time sink!
Pitchers and catchers, music to my ears!
And take it away, Dr. Fryhofer — nice job on this video!
https://www.youtube.com/watch?v=GTDqY8WM-dk



Patient question: if you’ve had the old shingles vaccine, should you get the new shingles vaccine as well for added protection?
Simple answer is “Yes.” A more nuanced answer can be found by fast-forwarding the video to around 3 minutes, where the discussion of “waning efficacy” of the old vaccine is reviewed.
So the longer ago you had it, the more benefit you’ll get from the new vaccine.
Paul
Great post as always! One name still befuddles me: is it Chlamydophila pneumoniae or Chlamydia pneumoniae? What about psittaci? File this one under things that keep nerdy internists up at night.
Patient question: Can a 65 yr old HIV+ patient with a CD4 count >900 get RZV. The patient has already gotten ZVL 4 years ago.
Sure thing!
Here’s what I wrote: “Does the recommendation include our stable, on-therapy HIV patients, who in increasing numbers are over 50? I say yes.”
There might be some who disagree, but that’s what clinical judgment is for.
Paul
Got a question about the Influenza. I never heard of the same person getting Influenza A AND B the same season, neither simoultaneously nor subsequently. Doens’t it happen? Isn’t ist tested?
Over here in Germany we have mostly B this year (59% is the official number), and my personal impression is that of a pretty good protection offered by the vaccine, btw.
For patients who test positive for flu on flu swabs & are symptomatic: should I be giving them the flu shot? (The ACIP guidelines don’t help much here; they just list ILI symptoms as a “precaution”)
maybe i’m a dinosaur, but faxes are hippa compliant. our ehr can print to fax and we receive efax with no paper, the efax received can go into the ehr directly or delted etc..
Feel free to disagree with me vehemently!
I got my first vaccine last week since I received the live vaccine 15 years ago. I thought the price would be the most painful component since it isn’t covered by Medicare. I can’t overemphasize how painful that shot was. I could perform most of my daily activities once I was able to put a shirt on. When it came to swimming my daily mile of freestyle which I rarely miss that was delayed for 3 days when I could finally raise my arm.
Not for publication:
I have an email from our hospital that details (lightly; you’ll see) a novel way to “spread” C diff.
Key words also include “encephalopathic” and “rectal tube.” Oh, and some centrifugal physics…
I can’t ID the facility, for obvious reasons.
Send?
tom
re: CDC has issued dietary advice for Valentine’s Day.
this is a wind-up, right? Someone is getting February 14th and April 1st confused?
Every physician should read and memorize what is quoted by the anesthesiologist about pain:
“Pain is a part of life. We cannot eliminate it nor do we want to. The pain will guide you. You will know when to rest more; you will know when you are healing. If I give you Vicodin, you will no longer feel the pain, yes, but you will no longer know what your body is telling you. You might overexert yourself because you are no longer feeling the pain signals. All you need is rest. And please be careful with ibuprofen. It’s not good for your kidneys. Only take it if you must. Your body will heal itself with rest.”
Brilliant!
He obviously was not a person who carries the gene for feeling greater pain than the average person, like many redheads do. Too much pain interferes with healing and a patient’s willingness to move at all and therefore bloodflow to the wounded area. There needs to be a balance, not a calous doctor.
I make a plea to the microbial taxonomists of the world: if you feel the need to change an organism’s name where there is an important pathogen and a less clinically-relevant variant in the mix (e.g., Pneumocystis, Propionobacterium), please change the name of the latter and not the former. I am not very worried about the names of rodent commensals and soil saprophytes, but “Cutibacterium” and the like are getting in my nerves.
On the topic of influenza, I am getting a lot of questions on 2nd dose vaccine. Typical scenario is a health care worker who has received their vaccine in September and are concerned about ongoing exposure and waning immunity. The CDC and ACIP do not recommend 2nd dose vaccine in the same season except in certain pediatric population. But some studies suggest that it might be reasonable to go for that second shot.
http://www.eurosurveillance.org/content/10.2807/ese.18.05.20389-en
What is your take on this?
Ramesh
The new name of Clostridium difficile is wrong. It should be Clostridioides difficilis (like Bacteroides fragilis, not fragile), as the suffix -oides should be masculine in Latin, not neuter..