An ongoing dialogue on HIV/AIDS, infectious diseases,
December 31st, 2008
Free Antibiotics!!!
Yes, the northeast supermarket/pharmacy chain Stop & Shop will now offer antibiotics — for free.
(And they are not the first. Take a look at this amazing advertisement.)
Says Stop & Shop’s “consumer advisor” Andrea Astrachan:
Stop & Shop pharmacies are committed to improving the health and wellness in our communities during the winter season when families are susceptible to coughs, and certain cold-related [emphasis most definitely mine] and bacteria-borne illnesses. As the provider of fresh, wholesome foods that help our customers stay healthy, we feel it is equally important to offer these free antibiotics to fight illness.
Fresh food linked with free antibiotics! What would Michal Pollan say?
And call me cynical, but could it be that someone looked at the profit margins on generic amoxicillin compared with, say, your typical cough/cold remedy, and thought … “Hey, if we can get them here for our free antibiotics, maybe they’ll grab some NyQuil, and some Tylenol PM, and some Tenzaprine AQ …”
(I made “Tenzaprine AQ” up. Not bad, eh?)
The list of free antibiotics is here — not much of a surprise what’s included, as all are widely-used generics. (Sorry, no linezolid.) And it should be noted that ciprofloxacin’s stock seems to have fallen almost as far as Enron’s.
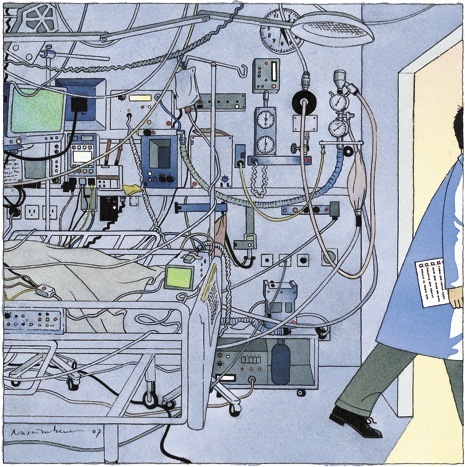
Of course in many situations the generic antibiotic is the right one to use, and I’m sure the consumer will appreciate this $10 or so savings off the pharmacy bill. But if ever there were a time to bring out (again) this wonderful New Yorker cartoon, this is it!
December 29th, 2008
Required Reading: Introducing the “iPatient”
Many HIV/ID specialists first heard of Abraham Verghese from his book My Own Country: A Doctor’s Story, which was published in 1994. He told us what it was like to be a newly-minted ID doctor, thrust into treating the first cases of HIV/AIDS in a remote town in Tennessee during the mid-1980s.
Compelling stuff — I thought the book was terrific. (And apparently I’m not alone, as I’ve received it as a gift no fewer than 3 times.)
In this week’s New England Journal of Medicine, Verghese has a wonderful perspective piece on a phenomenon that will be all-too familiar for doctors working in academic medical centers:
On my first day as an attending physician in a new hospital, I found my house staff and students in the team room, a snug bunker filled with glowing monitors. Instead of sitting down to hear about the patients, I suggested we head out to see them. My team came willingly, though they probably felt that everything I would need to get up to speed on our patients — the necessary images, the laboratory results — was right there in the team room. From my perspective, the most crucial element wasn’t.
What follows is a beautiful description of the tension between the “traditional” ways of clinical medicine — which involve taking real histories and doing actual physical exams — and the new way, which uses in place of the real patient “an entity clothed in binary garments: the iPatient.” And what’s wrong with treating the iPatient?
Pedagogically, what is tragic about tending to the iPatient is that it can’t begin to compare with the joy, excitement, intellectual pleasure, pride, disappointment, and lessons in humility that trainees might experience by learning from the real patient’s body examined at the bedside. When residents don’t witness the bedside-sleuth aspect of our discipline — its underlying romance and passion — they may come to view internal medicine as a trade practiced before a computer screen.
Even if you don’t believe in his premise — that something is lost when “the iPatient’s blood counts and emanations are tracked and trended like a Dow Jones Index” — this is a nifty bit of medical writing. You’ll find here none of the sanctimony such pieces often have (“in my day, we spun our own hematocrits, and were the better for it …”), just common sense about the potential consequences of focusing more on the computer screen than the person being treated.
Highly recommended.
December 23rd, 2008
Flu Resistance to Oseltamivir: The Bugs Win Again
 I must admit, the recent report that 49 of the 50 H1N1 flu viruses tested by the CDC are resistant to oseltamivir caught me by surprise. For the non-math majors among the readership, that’s a 98% resistance rate. Yikes.
I must admit, the recent report that 49 of the 50 H1N1 flu viruses tested by the CDC are resistant to oseltamivir caught me by surprise. For the non-math majors among the readership, that’s a 98% resistance rate. Yikes.
Actually, the rate of resistance is so high that at first I didn’t believe it when my wife told me — thought she’d flipped the numbers. “You mean that 1 of 50 was resistant,” I insisted — wrongly. As usual, the pediatrician has the accurate news on the latest outbreak — I should have learned that long ago.
So … what happened? Last year the resistance rate was only 10%, and it’s not as if since then we’ve put oseltamivir in the drinking water. The bulk of people with influenza never get diagnosed or treated, so it can’t be due to excessive prescribing on the part of clinicians. I doubt there’s much in the way of off-label or illicit use, and certainly nothing like this is showing up in my spam filter:
Brand name T-A-M-I-F-L-U cheap! From bestcanadapharmacy.com
One smart virologist I know suggested it might be the result of preventive programs in nursing home-type settings during flu outbreaks. These preventive treatments can go on for weeks, so if the resistant viruses have any sort of evolutionary advantage, they could become the dominant strain.
For now, interim guidelines for management of patients with influenza are available here. We’ll be using zanamivir (must be the best name for an antiviral ever — too bad it can’t be used in kids or patients with asthma), and our old friend rimantadine — though this latter drug has no activity against influenza B, and of course H3N2 viruses are already likely to be resistant.
Or we’ll be using nothing but TLC, which is kind of where we were several years ago. And chalk another one up for the bugs, they are (in aggregate) pretty darn smart.
December 19th, 2008
Infectious Disease in the ICU: Help Please? Part I
I am currently attending on the inpatient service, which means I spend a good chunk of my day seeing new ID consults and rounding on follow-ups. As I’m sure is true in most hospitals, many of these consults are from the intensive care units (ICUs).
After 18 years in this ID business, I confess I still find myself quite challenged by ICU Infectious Diseases. It’s not due to the complexity of the cases, in fact just the opposite — paradoxically, there’s a sameness to the cases that is worlds away from the wonderful variety of ID/HIV elsewhere: the outpatient with fever of unknown origin, or the inpatients with endocarditis, meningitis, orthopedic infection, HIV-related complication, or tropical fever (the stuff that makes up much of the rest of the consult volume). One intensivist says that once patients get past the first few days after admission, most of the medical issues they face are similar.
From the ID perspective, this means “rounding up the usual suspects,” including searching for line infections, UTIs, C diff, sinusitis, pancreatitis, surgical site infections, acalculous cholecycstitis, drug fever, infected pressure ulcers and — especially — nosocomial pneumonia.
There’s a sameness to these investigations that makes individualizing care difficult, and often forces us to focus on the (abundant) microbiologic data as distinguishing characterisitics. Just how resistant are the bacteria isolated from this patient’s respiratory sample? How many different possible pathogens can be cultured from a surgical drain? What is the significance of candida isolated from several non-sterile sites? How about those few colonies of coagulase negative staph on a removed line tip?
So where to go for help? For a comprehensive “how to” for this patient population, check out the recent IDSA/American College of Critical Care Guidelines. It’s an impressive document.
And give yourself plenty of time — it’s 20 pages long, and has over 200 references.
(In Part II, the issue of empiric antibiotics in the ICU.)
December 5th, 2008
New Case Definition for HIV Infection? Yawn …
The CDC has revised its case definition for HIV infection and AIDS, so that now laboratory evidence — a positive antibody test, or detectable HIV RNA or DNA – is required for the diagnosis.
It’s not intended to guide clinical practice, but still — what took them so long? A clinical diagnosis of AIDS was only necessary before HIV had been discovered. I cannot imagine someone reporting a case of AIDS or HIV infection without a positive blood test, especially since there have been several well-publicized cases of erroneous HIV diagnoses when laboratory confirmation was unavailable, or not performed.
So good move here, glad the epidemiologists have caught up. And nostalgists may enjoy reading prior versions of various AIDS case definitions here.
December 4th, 2008
More Support for HIV Screening
On Monday December 1 — World AIDS Day, if you’re keeping track — the American College of Physicians released a position paper supporting routine HIV screening for adolescents and adults in the United States.
(If you don’t want to read the whole thing, we’ll have a perfectly-executed summary by the inimitable Abbie Zuger on our AIDS Clinical Care site any day now; it’s been written, but somehow getting material up there is harder than it is here. Go figure. UPDATE: Now you can read it here.)
In essence, these ACP Guidelines are highly concordant with those issued in 2006 by the CDC: One-time testing for adults in health-care settings. Frequency of repeat testing to be determined by risk assessment.
This leaves the US Preventive Services Task Force as a mild voice of dissension about the issue of HIV screening, as it neither endorses nor discourages routine screening. The USPSTF does recommend screening “at-risk” populations, a useful strategy but one that still leaves a substantial proportion of HIV diagnoses undetected.
Meanwhile, the number of states still requiring written informed consent for HIV testing continues to fall …
November 25th, 2008
Coming Soon: A Great Advance in TB Diagnostics
An all-too-frequent problem in the ID clinical world is the case where tuberculosis is possibly the diagnosis, but confirming it is difficult, or impossible.
Now, in a scientific breakthrough of such magnitude that it warranted front page coverage in our local newspaper, I am pleased to report that we may have a solution: giant rats.
Yes, giant rats. In a pilot program in Daar es Salaam, rats evaluate saliva samples at a rate of 40 every 10 minutes, signaling with “unmistakable paw motions” when they detect a sputum infected with TB.
And here’s a bonus — they can also sniff out land mines, in case you happen to need that service too.
No doubt these critters will be showing up in our microbiology labs any day now. I can’t wait to read the OSHA regulations for their protection.