An ongoing dialogue on HIV/AIDS, infectious diseases,
March 14th, 2009
Maybe It’s Not the Cheeseburgers
 … At least that’s the implied message in this nice paper from the latest Annals of Internal Medicine, which evaluated responses to lipid-lowering therapy among patients with and without HIV.
… At least that’s the implied message in this nice paper from the latest Annals of Internal Medicine, which evaluated responses to lipid-lowering therapy among patients with and without HIV.
The study included patients from the Kaiser Permanente of Northern California integrated health system, with 829 individuals with HIV and 6941 without.
The quick summary is that those with HIV responded less well to lipid lowering drugs than the HIV negative patients — something that comes as no surprise to HIV providers, as we’ve scratched our heads for years while various statins, fibrates, and omega-3s have made barely a dent on some pretty scary lipid profiles.
There were a couple of other key take-aways from the paper. Pravastatin — which just happens to have the fewest drug-drug interactions with HIV drugs — was less effective than other statins. (Oh well.) It’s been fairly unanimous among cardiologists I’ve spoken with that they consider pravastatin a fairly wimpy lipid-lowering drug.
In addition, those on boosted PIs had a blunted triglyceride response to gemfibrizol compared to patients on other forms of HIV therapy. These are, of course, the very people who need triglyceride-lowering the most!
In practice, most patients on a boosted PI are on it for a reason — resistance, contraindications or intolerance to other drugs — so switching them off of it is rarely straightforward. (See this cautionary tale from CROI.) Regardless, we can certainly include “lipid friendly” in our list of desirable attributes for the investigational PK boosters.
February 26th, 2009
Meningococcal Resistance to Ciprofloxacin
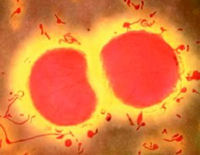 Ciprofloxacin-resistant Neisseria meningitidis has now been documented in the United States. Here’s a nice summary in Journal Watch, with two different perspectives.
Ciprofloxacin-resistant Neisseria meningitidis has now been documented in the United States. Here’s a nice summary in Journal Watch, with two different perspectives.
I suppose we shouldn’t be surprised, but it did take a while. (At least compared to that other famous neisseria-bug, Neisseria gonorrhoeae.)
Oh well.
Why is this important? As every practicing ID doc/primary care provider/public health official knows, nothing strikes fear into a community quite like a case of invasive meningococcal disease. Since household contacts of these cases have a many-fold increased risk of developing the disease, preventive therapy is recommended for any close contact — with “close” being defined nicely by one infection-control practitioner I know as “coughing distance.”
But we all know that prophylaxis extends way beyond this — not surprisingly, many more people request and get preventive therapy than actually need it, and in part this is because it’s so easy to do: a single dose of ciprofloxacin.
Now this needs to be reconsidered. Although it’s up to each local department of health to determine the recommended preventive therapy, I suspect it won’t be long before we’re all back to rifampin (four doses over two days, drug interactions) or a shot of ceftriaxone (ouch).
February 11th, 2009
CROI 2010 Dates and Location Announced
February 16-20, 2010, San Francisco — at least according to John Mellors during his opening remarks here in Montreal.
Is it really one day longer? [Update — no, it’s Feb 17-20.] Really during the week of Presidents’ Day? (School vacation week in New England … but I realize you can’t make everyone happy with schedules.)
In other words, regardless …
February 4th, 2009
Brush with Greatness: Bruce Walker
Bruce Walker has just received a $100 million grant from Terry and Susan Ragon to start a vaccine research institute, with a focus on finding an HIV vaccine. The news of this gift (which as you can imagine has been floating around these parts for some time) is all the more remarkable since it comes at a time when philanthropic efforts are declining precipitously, for obvious reasons.
So what kind of person is Bruce Walker? Aside from his being a genuinely nice guy, several words come to mind: Exuberant, optimistic, energetic. He’s done brilliant translational research in the field of HIV pathogenesis and — no small matter — can explain his work clearly and engagingly to non-lab scientists.
In fact, it may be this last skill that ultimately enabled him to get this incredibly generous gift. Sure, he has the scientific credentials, with literally hundreds of published papers and numerous prestigious grants.
But there are other folks like that in academic medical centers.
Which brings me back to what I think makes Bruce so special. He can describe his research with enthusiasm and clarity to just about anyone — other basic researchers, clinicians, journalists, high school undergraduates, Bill Gates, Elizabeth Taylor, and no doubt the guy he meets in his neighborhood who is out just walking his dog. I’m not kidding.
No matter how abstruse the immunology, he always brings it back to how this work could help — is going to help — actual human beings.
So congratulations to Bruce. After a year of major setbacks on the vaccine research front, this bit of good news is welcome indeed.
(Second in a very occasional series.)
February 1st, 2009
Whither PEPFAR?
Mark Dybul will no longer be running the President’s Emergency Plan for AIDS Relief, or PEPFAR, the multi-billion dollar international program for HIV treatment program started by Bush in 2003.
Some are happy. Others are not.
(Note the exquisite use of euphemism — he was “required to submit his resignation“, not “fired.”)
Experts on global HIV treatment can debate the pros and cons of this move, but can anyone truly be surprised? In this most highly politicized of diseases, how could we expect otherwise?
Right from the start, I viewed PEPFAR as kind of like a lifesaving medication that had a few side effects that you wished weren’t present, but was, well, lifesaving — so you dealt with it. Sure, critics might (and did) carp at the abstinence education requirement, the restrictions on treatment for “sex workers” (some say this isn’t the preferred term now, if not help me with this), and the fact that PEPFAR was set up independently from other already established treatment programs. And what about the 40+ million Americans without insurance? Why no PEPFAR-equivalent for them?
But it’s hard to argue with the results — In some of the world’s poorest nations, millions got HIV treatment who previously could not.
So say what you will about the politics of this recent move, PEPFAR was a groundbreaking piece of legislation by Bush, and Dybul was its on-the-ground leader. And given the past track record of some Repubicans on this disease, for these accomplishments they must get some credit.