An ongoing dialogue on HIV/AIDS, infectious diseases,
January 6th, 2011
Thursday Thienamycins
 Plenty going on in the ID, HIV, and (for the middle of winter) baseball worlds:
Plenty going on in the ID, HIV, and (for the middle of winter) baseball worlds:
- Just out in CID, there’s a comprehensive review of Management of MRSA as part of the IDSA’s Practice Guidelines Series. Soft tissue infections, bacteremia, endocarditis, pneumonia, bone and joint infections, frequent relapses … MRSA in all its painful glory. Some interesting tidbits: 1) no gentamicin recommended for MRSA native-valve endocarditis or bacteremia (a pet peeve of mine, hope that practice disappears); 2) ECHO recommended for all adult patients with bacteremia, with a preference for transesophageal ECHO; 3) no systemic antimicrobials recommended as part of “decolonization” strategies in cases of recurrent MRSA soft tissue infections; 4) no mention of household pets as a source of MRSA.
- Speaking of MRSA, ceftaroline — approved late last year by the FDA — is now actually available for use (that is, obtainable by your hospital pharmacy). This is the first beta lactam with anti-MRSA activity, and while it has been approved for community-acquired pneumonia and complicated skin and soft tissue infections, I strongly suspect it may eventually have another role — namely, management of MRSA bacteremia/endocarditis, especially refractory cases. After all, our current therapy for that condition is pretty dismal. Time (and I hope a prospective clinical trial, though nothing here) will tell whether ceftaroline in fact offers an advantage in this challenging situation.
- Etravirine now comes in a 200 mg tablet, reducing the pill burden to 1 pill twice daily. Although not approved for once-daily use, the pharmacokinetic profile supports giving the drug this way, so I wouldn’t be surprised to see a greater use of this NNRTI as a once-daily “key third drug” in patients without NRTI resistance. (It’s an “unlabeled use”, but so be it.) Turns out that although the new formulation is still uncoated, it may have reduced the quirky chalky texture of the 100 mg tablets, as tests conducted by the company show that it’s easier to swallow. It still can be dispersed in water, if patients prefer to take it this way.
- Rifaximin, the non-absorbable cousin of rifampin, reduces symptoms of irritable bowel syndrome (IBS). Great news — until you read the fine print, which shows that the placebo group did nearly as well (around a 40% response rate for rifaximin, vs 30% for placebo). Oddly, this rifaximin/IBS study comes on the heels of this well-publicized paper, which showed that placebos for IBS still worked even if patients knew they were taking them. I think we’re compelled to think again about how to leverage the extraordinary power of the mind to help control certain diseases.
- As expected (and deserved), Robbie Alomar was elected to the National Baseball Hall of Fame, receiving 90% of the votes. Does his alleged HIV positive status “pose a problem” for the Hall of Fame? I think not — so long as he does the right thing and tells the truth, whatever that may be. Again, as I’ve written before, the acceptance speech he gives in Cooperstown this summer could be the perfect opportunity.
Thienamycin’s real identity? Read all about it.
January 4th, 2011
HIV Year in Review Posted on Journal Watch
Want to catch up quickly in HIV clinical care?
Forgive the bias, but the best strategy may well be to read our “Year in Review 2010” summary over on Journal Watch: AIDS Clinical Care.
Always interesting to speculate what we’ll be choosing next year — I wouldn’t be surprised if progress in eradication (i.e., cure!) starts moving up the list …
December 22nd, 2010
Holiday Hafnias
 Some items to consider in HIV/ID world as you dig into your salmonella-free holiday bird:
Some items to consider in HIV/ID world as you dig into your salmonella-free holiday bird:
- Drug label change for stavudine (d4T): The label no longer has recommendations for dose-reduction in case of peripheral neuropathy, and cites data more strongly linking d4T use to lipoatrophy. The strategy of decreasing the dose to reduce d4T toxicity hasn’t made much sense for over a decade, since it’s long been known that most other NRTIs have less mitochondrial toxicity. Which of course begs the question — why is anyone in the United States on d4T at all?
- Speaking of HIV drug label changes, darunavir is now approved for once-daily dosing in treatment-experienced patients, provided there is no darunavir resistance. This makes sense: once-daily dosing greatly exceeds the required levels for inhibition of susceptible viruses, and the strategy was shown to be OK in the ODIN study. I suspect most of us have been doing this for many months already (certainly I have).
- Another (mostly) negative study of echinacea for colds over in the Annals of Internal Medicine. We are so desperate for something that actually works for colds that we keep flogging this dead horse. Or maybe it’s “not dead yet”? But whether this new study settles the issue once and for all, certainly any large effect of echinacea seems highly unlikely. Which reminds me — remember when pleconaril was seeking an indication for treatment of the common cold? A well-respected ID doc I know thought that if it got approved (it didn’t), hardly anyone would want it since most colds are “mild and self-limited”. But one peek at the “coughs and colds” aisle at your local pharmacy shows you just how wrong he was!
- Want the best site for the latest on the XMRV controversy? My personal favorite source is the Wall Street Journal Health blog, and here’s the most recent entry.
- For those of you vacationing in Missouri, and somehow tempted to eat raw crayfish, check out these case reports of paragonimiasis in the MMWR. My favorite sentence in the report: “Behavioral factors that led patients in this report to eat raw or undercooked crayfish included alcohol consumption, dares, and demonstration of survival skills.” Any surprise that 8 of 9 of the cases were in males?
Happy Hafnias!
December 17th, 2010
Update on Berlin Patient II: Still Cured of HIV
First, who was Berlin Patient I?
Second, over in the journal Blood is the latest update on Berlin Patient II, the guy apparently cured of HIV by bone marrow transplantation:
We have previously reported the case of an HIV-infected patient in whom viral replication remained absent despite discontinuation of antiretroviral therapy after transplantation with CCR5Δ32/Δ32 stem cells… In the present study, we demonstrate successful reconstitution of CD4+ T cells at the systemic level as well as in the gut mucosal immune system following CCR5Δ32/Δ32 stem cell transplantation, while the patient remains without any sign of HIV infection… In conclusion, our results strongly suggest that cure of HIV has been achieved in this patient.
Ever since this was first presented as a poster at CROI in 2008, it was pretty clear that this was a special case, and I’ve written about it several times before — first time here.
What’s different now, of course, is that the longer duration of follow-up has allowed the authors to give much more detailed information about both his virologic and immunologic status — and to make more confident statements that he is in fact cured of HIV.
 And I agree.
And I agree.
But numerous questions about this fascinating case remain, including the biggie — how did this happen? Was it the CCR5-negative status of the donor’s cells? Something about the “conditioning” (there’s a euphemism for you) regimen? The fact that he’d been virologically suppressed when he went into the transplant? (It’s obviously not just this.) Some combination of the above?
And though of course this transplant strategy can’t be widely adopted, one would expect at least one other similar case to surface soon, right?
By the way, for HIV history trivia buffs, this guy was Berlin Patient I. Must be something in the water.
December 13th, 2010
My (Second) Favorite Journal Switches Publishers
 I absolutely love the journal Clinical Infectious Diseases.
I absolutely love the journal Clinical Infectious Diseases.
It’s easily my second-favorite journal.
(Can you guess my favorite? Perhaps this new “About this blog” section will give you a hint.)
But back to CID — here’s why I love it:
- Great content. Seems every issue has fascinating studies, usually of great clinical relevance to the field of Infectious Diseases. In this issue alone, tons of stuff on influenza, but also a randomized trial of cranberry juice for recurrent UTI (negative, oh well), a terrific editorial on MRSA, and the usual smattering of interesting HIV/AIDS studies.
- Lots of it, too. Plenty to read each month (all kinds of studies, editorials, photo quizes, reviews, letters), and more rolling in all the time electronically. Each year content from CID is among the top sources for both our ID and HIV Journal Watch newsletters. To quote our Executive Editor in Journal Watch: AIDS Clinical Care, “Don’t those guys ever sleep?”
- Terrific web site. Could this be the single most user-friendly web site in the business? I love the way the issues are laid out on-line, with the left panel allowing quick and easy access to specific sections of the journal.
- Wonderful covers. Who knew so much art had an Infectious Diseases theme? Great stuff: Congenital syphilis in a Rembrandt portrait, Elizabeth I smallpox medal, St Sebastian lancing a plague bubo … Seems a graphic rendition of various scourges has been a popular art theme for some time, and CID is there to show us!
- Heavy paper. Well, that used to be a plus — now that I read most of the content on-line, it’s less important to me, but boy the shear heft of both CID and JID just exude quality.
Which brings me to their new publishers, Oxford University Press (OUP), who are taking over from the University of Chicago Press. According to Sherry Gorbach in his introduction, OUP won the right to publish CID “after a competitive bidding process” — one envisions something like what’s going on right now for Cliff Lee.
Not surprisingly, the new publishers have a new CID web site, and I must say on first glance it’s going to take a bit of getting used to. The old web site just scanned so easily. And with this revision, you can’t even click on the cover anymore to find out what it’s about — something I always enjoyed. (Here’s a nice example, reproduced in the picture above.)
Now I’m sure I’ll get used to it, it’s only been one issue. And it’s still a great journal.
December 9th, 2010
Chronic Lyme Tough to Diagnose, Tough to Treat
Over at the Chicago Tribune, there is this superb review of the Chronic Lyme disease issue.
Lyme disease is real. The bacterial infection, chiefly transmitted by deer ticks, can cause rashes, swollen joints and inflamed nerves, and usually is curable with a round of antibiotics.
But doctors around the country are telling patients with common medical problems such as back pain, poor concentration and fatigue that their ailments stem from a chronic form of Lyme disease that can evade standard treatment and wreak havoc for years. To fight what they believe is a persistent infection, the doctors often order months or years of intravenous antibiotics, which can cost tens of thousands of dollars.
Strong evidence isn’t on their side. But in a golden age of dubious medicine, that doesn’t matter.
My advice: read the full article, as I cannot recall a better summary in the lay press of this highly-contentious topic.
Oh, and for the record, in my experience there are few encounters more challenging in ID practice than addressing the diagnosis of “chronic Lyme.”
Many patients given the diagnosis are (legitimately) so desperate to find an explanation for their suffering — and to do something rather than nothing — that they latch onto this unproven diagnosis and are willing to receive potentially harmful therapy rather than continue to live in misery without taking action.
And when, as an ID doctor, you review all the history and data and find no evidence of Lyme, you make a person who feels sick feel even worse — because usually there is no alternative infectious explanation for their various complaints.
It’s an unbelievably difficult situation. In many ways, chronic Lyme is even more difficult to treat than HIV — which was my original (jokey) title of this post, until someone told me it might be offensive. But you get my point.
So shared experiences, other thoughts, potential strategies for managing “chronic Lyme” — from my ID colleagues, from other providers, from patients — would be much appreciated.
December 6th, 2010
Tough Diagnoses: Neurosyphilis, Then and Now
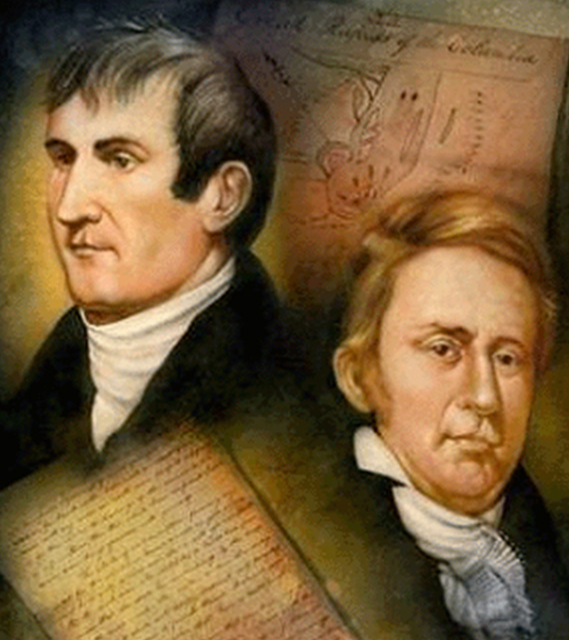 During Thanksgiving, my brother-in-law — who is a professional musician and also a passionate history buff — gave me a scholarly paper to review on the strange death of the famous American explorer Meriwether Lewis, of “Lewis and Clark” fame.
During Thanksgiving, my brother-in-law — who is a professional musician and also a passionate history buff — gave me a scholarly paper to review on the strange death of the famous American explorer Meriwether Lewis, of “Lewis and Clark” fame.
The bottom line? Lewis may well have had neurosyphilis — at least that’s the premise of the epidemiologist Reimert Thorolf Ravenholt, who, in a nearly 13,000 word report, ultimately concludes:
The fabric of evidence that syphilis acquired during the explorative trip to the Pacific Coast was the underlying cause of Lewis’s death includes these threads: (1) Lewis was in excellent health when he set forth up the Missouri River; (2) several Indian tribes suffering from syphilis were encountered; (3) sexual intercourse with women of these tribes by Corps members was frequently urged by the Indians and was commonplace; (4) several Corps members (probably at least eight) did develop syphilis; (5) when encountering the Shoshoni tribe on the Continental Divide, Lewis had both a propitious opportunity and a compelling need for sexual intercourse; (6) a few weeks later, he developed illness which became severe and disabling for several months, but the nature of which was not described; (7) for some months in 1807, following his return from the expedition, he was incapacitated by illness, the nature of which was not divulged; (8) during 1808-809, he developed progressive illness afflicting his central nervous system and diminishing his judgment faculties; (9) his terminal months in 1809 were characterized by progressive, episodic, febrile illness, with severe mental and behavioral disorders highly characteristic of paresis; (10) Lewis himself recognized that he was suffering from a progressive disease likely to be fatal; (11) Thomas Jefferson and William Clark readily understood why his death was a probable act of self destruction.
Emphatically not the Lewis and Clark story I learned in 5th Grade!
But sure, the diagnosis of neurosyphilis sounds plausible. Sexual indiscretion followed by rashes followed by a progressive neurologic disease with increasingly bizarre and unreliable behavior. (Not so sure about the fever part.)
But while these speculative diagnoses are fascinating both historically and medically (Mozart’s death has 325 citations in PubMed), one inevitably gets back to the problem of confirming the diagnosis, which is almost always impossible.
Furthermore, there are several reasons why neurosyphilis is in particular a difficult diagnosis to prove, even today, including:
- Protean symptoms that wax and wane.
- Variable latency period.
- Relatively uncommon, especially since the discovery of penicillin.
- Unreliable diagnostic testing and no readily available culture.
- Clinical and lab-based manifestations have significant overlap with other diseases.
- Lots of what was called neurosyphilis back in the day probably was something else, making much of the clinical teaching about the disease highly subjective.
In fact, with the exception of obvious cases — ocular disease concurrent with secondary syphilis, or CSF pleocytosis and positive VDRL in the setting of a classic clinical presentation — it otherwise seems that the diagnosis of neurosyphilis is made only after an esteemed clinician definitively, confidently, and loudly states THIS IS NEUROSYPHILIS.
Especially if that clinician has a certain well-aged gravitas.
December 1st, 2010
World AIDS Day: See You in Kuala Lumpur
 A few random thoughts on this 2010 World AIDS Day.
A few random thoughts on this 2010 World AIDS Day.
- Now you can mark your calendars for the next three International AIDS Society/World AIDS Meetings: 2011 in Rome, 2012 in Washington, DC — and now, 2013 in Kuala Lumpur, Malaysia. And what do all 3 of these cities have in common? Extreme summer heat! (For Kuala Lumpur, it’s actually just extreme heat, not just in the summer.) Probably some sort of weird compensation for several frigid February’s at CROI.
- Not mentioned in my discussion of the once- versus twice-daily raltegravir study was the study name — which was QDMRK. Yes, the sponsors (can you guess who they were?) continued the self-referential theme that started with BENCHMRK, followed by STARTMRK and then SWITCHMRK. Could a study of coffee be planned, “PERCMRK”? Of the Thanksgiving meal, “TURKMRK?” Or of how to avoid a task, called “SHIRKWORKMRK?”
- On the topic of study names, this really has been a banner period for acronyms. Here’s a partial list just from this year: CAPRISA, CAMELIA, PROGRESS, SPARTAN, ECHO, THRIVE, SHIELD, VERXVE, VIKING, SPRING, SPIRAL, ODIS, ROCKET, SENSE, METABOLIK, ATLAS, ATLIS (yes, there’s both an ATLAS and an ATLIS). Trust me, I live and breathe this stuff daily, and still have trouble keeping all of them straight.
- Some good news on the HIV testing front in this report from MMWR: Compared with 2001, today more people are aware of their HIV status, and “late” diagnoses are declining. However, it’s still striking that even though we’ve had effective HIV treatment for nearly 15 years, around one-third of people are still diagnosed with HIV when they’ve already had complications from AIDS or have severe immunodeficiency.
Anyway — what are your thoughts on these red ribbons? Powerful awareness tool, helpful in keeping HIV on the radar screen? Or over-commercialized, politically-correct, past-its-prime symbol? You decide …
November 29th, 2010
Once-daily Raltegravir “Not Non-Inferior” to Twice-Daily
In your electronic in-box this AM, this press release from Merck:
… although the treatment regimen that included ISENTRESS once daily enabled more than 80 percent of patients to achieve viral suppression, ISENTRESS once daily did not demonstrate non-inferiority to the treatment regimen that included ISENTRESS twice daily. Merck said that based on the initial results, and following the recommendation of an independent Data Monitoring Committee, Merck will end the study
Raltegravir is of course still a great HIV drug, and its approval in 2007 marked one of the great steps forward in the history of HIV therapeutics.
I still remember John Mellors at CROI 2007 preparing us to see the BENCHMRK data for the first time — his exact words were probably not, “this will knock your socks off”, but they could have been. Never before had any antiretroviral agent done so spectacularly well in patients with high-level resistance, and it’s hard to estimate how many patients with longstanding HIV infection have had their lives literally saved with raltegravir.
But is it a once-daily drug? Probably not based on the results of this study, where twice-daily was simply better — or, to be more statistically precise, once-daily did not demonstrate non-inferiority.
And in an odd recapitulation of the early days of the protease-inhibitor era, the story is quite similar to what happened to indinavir, another Merck antiretroviral:
- Both drugs were major advances in the field
- Both drugs had an odd disconnect between PK and response
- Both drugs failed tests of less-frequent dosing
The major difference, of course, is that even the once-daily raltegravir arm in this study did quite well — an 83% response is not too shabby.
It’s just that today, our standard-of-care for first-line therapy is (wonderfully) high, and the twice-daily treatment arm had an 89% success rate, with the advantage seen in particular in patients with HIV RNA > 100k. The difference in response put the once-daily approach just outside of the protocol-specified criterion for non-inferiority.
And this steep price of entry for treatment-naive options is why both elvitegravir/c and 572, though promising, still have their work cut out for them.

 January 1, 2011
January 1, 2011