An ongoing dialogue on HIV/AIDS, infectious diseases,
March 8th, 2011
Really Rapid Review of CROI 2011 — and No CROI 2012 Dates
 With CROI 2011 now officially over, I offer below the following Really Rapid Review™ for ID/HIV Specialists with limited time — or for those who said they went to the conference but spent the entire week shopping in the Prudential Mall and eating at Legal Seafood:
With CROI 2011 now officially over, I offer below the following Really Rapid Review™ for ID/HIV Specialists with limited time — or for those who said they went to the conference but spent the entire week shopping in the Prudential Mall and eating at Legal Seafood:
- Lots on PrEP. Bottom line — it works if you take it, but lots of people in iPrEx didn’t take it, especially in non-US sites. And bone density goes down a bit in those receiving TDF/FTC, long-term implications not known. Based on conversations I had with colleagues, it didn’t seem that anyone had been prescribing PrEP much thus far.
- HCV treatment is about to get much more effective, and much more complicated. The drug-drug interactions with antiretroviral drugs and the first two HCV-protease inhibitors — telaprevir and boceprevir — are going to be really, really dicey. Sensational web-cast here of a plenary given by Stefan Zeuzem that summarizes lots of the key issues.
- Once-daily raltegravir doesn’t work quite as well as twice-daily. Old news, but detailed data on the trial presented here for the first time. Turns out PK does matter after all in the QD group.
- Speaking of raltegravir, if you predicted that approximately 25% of treatment-naive subjects who were put on boosted darunavir plus raltegravir would experience virologic failure, you are smarted than I am. These are two of our best drugs — how can we explain this?
- Time to learn a new drug name: “S/GSK1349572” = “572” = “dolutegravir” = “DTG”, which really does have antiviral activity against some raltegravir-resistant viruses.
- Two additional studies (here and here) show that blacks in the USA do worse than whites in clinical trials. The explanation must be at least in part socioeconomic, since clearly Africans in Africa are doing just as well on ART as people in resource-rich settings. Critical to figure out why we have this disparity.
- Many studies on inflammation and immune activation, including this incredibly counter-intuitive study of maraviroc intensification of already suppressive ART. Results are too complex for this Really Rapid Review™, but they go something like this: certain markers increased; others decreased; no one knows why; no one knows the clinical implications. Which pretty much sums up this whole “inflammation and immune activation” field right now.
- If you have active TB and advanced HIV-related immunosuppression — that is, CD4 < 50 — the time to start ART is sooner rather than later. (Similar findings in this study.) All this makes complete sense, given what we’ve seen from earlier studies in such sick patients (A5164, CAMELIA). Fact: Untreated advanced AIDS is worse than IRIS.
- Several years ago, plunked right into the middle of a slide session on clinical studies of antiretrovirals, came an out-of-nowhere basic science presentation (this might have been it) on “zinc fingers”. So odd was its appearance that it became something of an inside joke (a very inside joke) among certain HIV clinicians. (“Oh, he can’t tolerate ritonavir — maybe he’d do better on a zinc finger inhibitor.”) And guess what — zinc fingers are back! And it’s actually very cool stuff.
- Does PI-based ART in the mom lead to premature delivery? The Europeans have been saying so for some time, and this randomized clinical trial from Botswana supports that view. The questions remain — how clinically important? And what are the best alternatives?
- You know that question about whether NRTIs are needed in 2nd-line therapy (and beyond)? Based on these two studies (here and here), it certainly seems so. A randomized clinical trial — the so-called OPTIONS study — is ongoing to try and answer this question definitively.
Finally, unlike last year, if the CROI 2012 dates were announced, I didn’t hear them — nor did anyone else I spoke to at the conference. Darn. That “announcement” up there is a mock-up kindly crafted by my sister, who always did help me with my art projects in grade school.
But in case the conference organizers are still looking, there’s plenty of space at the Hynes Convention Center should they want to come back to Boston. Right now, this group is the only meeting booked for the whole month of February!
February 27th, 2011
CROI 2011 Starts Today
 With a fresh 4 inches of snow on the ground in Boston, the 18th Conference on Retroviruses and Opportunistic Infections (CROI) starts today.
With a fresh 4 inches of snow on the ground in Boston, the 18th Conference on Retroviruses and Opportunistic Infections (CROI) starts today.
Pocket program is available here (PDF format). Based on a (very) quick perusal, we can expect the following:
- Progress (lots of it) in prevention, with more from CAPRISA and iPrEx and the whole “treatment as prevention” theme
- Welcome HIV specialists to the new age of HCV therapeutics
- Several big clinical trials, including more details on once-daily raltegravir and studies on early vs deferred ART for HIV-related TB
- Numerous posters and presentations on cardiovascular, renal, neoplastic and bone complications
- Diverse studies on the maturing treatment programs in resource-limited settings
As always with CROI — which is the most concentrated (in a good way) of our scientific meetings — there will be a ton of miscellaneous other interesting stuff.
Come back here later for a more detailed summary and (if they announce it) the date of the 2012 conference!
February 17th, 2011
Zinc May Work for Colds — But Don’t Pretend It’s Not a Drug
Does zinc work for colds?
 Apparently it does, according to this Cochrane Review. From the “Plain Language Summary”:
Apparently it does, according to this Cochrane Review. From the “Plain Language Summary”:
This review identified 15 randomized controlled trials, enrolling 1360 participants of all age groups, comparing zinc with placebo (no zinc). We found that zinc (lozenges or syrup) is beneficial in reducing the duration and severity of the common cold in healthy people, when taken within 24 hours of onset of symptoms. People taking zinc are also less likely to have persistence of their cold symptoms beyond seven days of treatment.
Based on these results, and the ecstatic “I-told-you-so” reader comments on this New York Times report, there is likely something real going on here. It’s potentially pretty exciting, actually — a treatment for the cold!
But one thing is clear: Zinc for colds should be considered a drug — even though you can get it without a prescription, the FDA hasn’t reviewed it, and the lozenges may carry the word “natural” or “organic” on the label.
Why? Because in addition to their benefits, all drugs have side effects. And because there’s nothing “natural” about zinc supplements in people who don’t have zinc deficiency, it won’t be long before more side effects (remember this one with zinc nasal swabs?) or drug interactions occur in a least some individuals.
So stay tuned for further research on this area — and be ready for results that may be good and not-so-good.
February 14th, 2011
Pspring Training Pseudomonads
 A few ID/HIV issues to ponder as we welcome back the most important sport in the universe:
A few ID/HIV issues to ponder as we welcome back the most important sport in the universe:
- Interesting new Guidelines on UTIs from IDSA — especially their recommendations not to use fluoroquinolones for uncomplicated cystitis and to promote nitrofurantoin for 5 days to first-line for this indication. And welcome to fosfomycin — though this could eliminate one of the ID consultant’s few remaining tricks when getting a challenging UTI consult.
- So opportunistic infections are decidedly uncommon after prolonged virologic suppression, even if the CD4’s don’t increase. (Read the full paper for details.) I was asked once to give a talk to a group of HIV providers on what to do for persistently low CD4s despite effective therapy. It would have been a very short talk — the answer is basically “do nothing.” One could argue that we should stop CD4 measurements entirely after a couple of years of successful ART. What’s the point?
- Thought M abscessus infection was difficult to treat? Turns out it’s even harder than we thought — some of the macrolide-susceptible strains are actually “susceptible” (note quotes), as they have an inducible macrolide resistance gene (called “erm”) that cannot be detected on susceptibility testing. Read this latest study suggesting the importance of surgical therapy here, and this outstanding (and entertaining) editorial here for further info on this always-challenging entity.
- The latest ADAP Watch is here (PDF) — and it’s not pretty. To quote the report: “As of February 10, 2011, there were 6,235 individuals on AIDS Drug Assistance Program (ADAP) waiting lists in 10 states. This is a 32 percent increase from the 4,732 individuals on the December 2010 ADAP Watch.” Looks like more than half (3,204, to be precise) live in Florida — seems like some sort of action there is likely soon, right?
- I’ve been reading — and enjoying — Mark Crislip’s ID blog over on Medscape for several months now. It’s terrific! Well-written, funny, wise, and full of just the sort of cases we ID doctors see all the time, plus an impressive smattering of literature-citing even in situations that don’t obviously lend themselves to this approach. I cannot recommend it highly enough.
By the way, for those planning the trip out to Boston later this month for the Retrovirus Conference, we have a decided warming trend this week. Snow gone by the opening plenaries?
February 3rd, 2011
Disparities in HIV Diagnoses, and Interpreting CDC-ese
In anticipation of National Black HIV/AIDS Awareness Day (February 7), the CDC has issued a new report on the disparities in HIV diagnoses in the United States.
During 2005–2008, blacks/African Americans accounted for 13.6% of the population in the 37 states and 50.3% of the 156,812 diagnoses of HIV infection during that period … HIV transmissions in black/African American males were classified most frequently as male-to-male sexual contact (61.1%), followed by heterosexual contact (23.1%), injection drug use (IDU) (11.9%), and both male-to-male sexual contact and IDU (3.6%)… Among females, blacks/African Americans accounted for the largest percentage of diagnoses of HIV infection (65.9%) during 2005–2008. Most black/African American females diagnosed with HIV were exposed through heterosexual contact (85.2%), and the next greatest percentage by IDU (14.0%).
Some additional findings in this report:
- From 2005-2008, new diagnoses increased in black/African American Males; in all other groups, it was stable (see figure)
- The disparity between racial/ethnic groups was highest among persons aged 13–24 years, women, and persons with infection attributed to heterosexual contact
- In 2008, black/African American males and females were diagnosed with HIV infection at 8 and 19 times the rates for white males and females; 2 and 4 times the rates for Hispanic/Latino males and females, respectively
The authors of this report comment that “the higher rates of diagnoses among blacks/African Americans suggest that adolescents and adults from this population who are at higher risk for HIV infection might benefit [emphasis mine] from more frequent testing to facilitate earlier diagnosis.”
As usual, this is an outstanding report from the kind folks from Atlanta (who must feel this year like they’ve been tricked into living in New England).
But one of the things I’ve learned to recognize over the years of reading MMWR and other CDC reports, is that when they bring out the word “might” — a classic word from the CDC Manual of Style — what they really mean is: “We think you should do this but something is keeping us from stating it so bluntly.”
So let me be so bold: More frequent HIV testing is recommended for people at high risk for HIV — and the risk is high in certain black/African American communities, regardless of “risk factors”, as my colleague Kim Smith has wisely stated. Clinicians should be aware of the data presented here so that they can implement these recommendations appropriately.
January 28th, 2011
Wow, That Was Fast: PrEP Guidelines Appear
 With the ink barely dry on iPrEx — still tricky to type — along come “interim” guidelines from the CDC on pre-exposure prophylaxis (PrEP).
With the ink barely dry on iPrEx — still tricky to type — along come “interim” guidelines from the CDC on pre-exposure prophylaxis (PrEP).
Based on the results [iPrEx], CDC and other U.S. Public Health Service (PHS) agencies have begun to develop PHS guidelines on the use of PrEP for MSM at high risk for HIV acquisition in the United States as part of a comprehensive set of HIV prevention services. Completing the guidelines and obtaining expert input and public comment will take several months before they can be published. Concerns exist that without early guidance, various unsafe and potentially less effective PrEP-related practices could develop among health-care providers and MSM beginning to use PrEP in the coming weeks and months.
Since government organizations often move at glacial speed, the rapidity with which this appeared is truly impressive.
Some initial points worth emphasizing:
- This is just for TDF/FTC. Sure, other drugs might work — but let other studies determine that first.
- This is only for MSM at high risk for HIV. Yes, this was the group studied in iPrEx, and should be the predominant population treated. But if you knew of a heterosexual female at high risk (let’s say through domestic violence with a known HIV positive partner), would you exclude her?
- It is critical to exclude established or acute HIV infection before starting PrEP. The boxed recommendations at the bottom of the report are quite clear about this. Certainly this will increase the use of HIV RNA as a diagnostic test, and makes the combined HIV antibody/antigen assay seem much more valuable.
- Most people getting PrEP are at risk for other STIs. Screen them appropriately.
- Ongoing assessments of adherence, safety, and HIV serostatus are critical. PrEP only works if people take it, and continuing dual therapy if HIV is acquired could rapidly lead to resistance.
- Intermittent PrEP cannot be supported. Here I think the guidelines will not be widely followed, at least based on anecdotal discussions I have had with certain providers. But I understand why they needed to say this — intermittent PrEP hasn’t been proven effective — yet.
- Give a maximum of a 90 day supply. Important not to continue prescribing the drug without periodic monitoring, as noted above. I wonder where they came up with 90 days? Did they consult the rules?
I still want to know how they got this guidance out so fast — suspect they were working on it behind the scenes, awaiting publication of the study. Regardless, this is a timely release indeed, and the larger “comprehensive” set of guidelines on HIV prevention promise to be very interesting.
January 26th, 2011
Insurance Company Cheese Shop Redux
 I had an interesting exchange with one of our nurses this week about a long-term patient of ours.
I had an interesting exchange with one of our nurses this week about a long-term patient of ours.
The e-mails went something like this:
Got a fax from —-‘s insurance that his Lipitor won’t be covered anymore. They will cover simvastatin, lovastatin, and pravastatin. Let me know what you want to do.
Charlie
He’s on darunavir, and all three of those statins are contraindicated because of drug-drug interactions. Rosuvastatin?
Paul
Checked with them — rosuvastatin needs prior approval, and will cost him a lot more, but less than Lipitor. I’ll get the paperwork ready.
Charlie
An hour or so passes, and then this:
What dose rosuvastatin?
Charlie
5 mg daily, thanks.
Paul
Another hour, and then:
Just heard from them — after all the fuss, they approved the Lipitor after all. Seems they just wanted to waste our time.
Charlie
Hysterical.
Look, I get it that generics are usually more cost-effective than branded drugs. And I understand that health care costs are wildly out of control, and one way of controlling costs is to use generics whenever they are safe and effective, which is most of the time.
But think about the absurdity of the above case.
- The insurance company is paying for this man’s antiretroviral therapy, so they must know he’s on darunavir.
- They nonetheless are suggesting he switch to a contraindicated generic statin drug.
- They initially refuse to continue covering a drug that is working well and that the patient has been tolerating for years, but grudgingly will cover a slightly cheaper alternative.
- They set up barriers to jump over and tunnels to crawl through (the “prior approval” paperwork) even though there’s sound evidence to back up the requested brand-name treatments.
- After the obstacle course is navigated successfully by our experienced nurse, they relent and say that they’ll cover the original prescription after all.
And here’s the best part: The exact same thing happened last year with this patient — with the same insurance company!
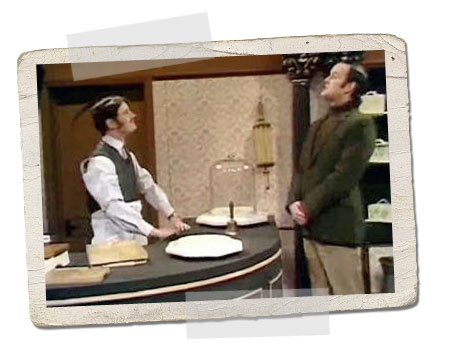
Reminds me of the classic Monty Python “Cheese Shop” sketch, where the customer (John Cleese) methodically asks cheese shop guy (Michael Palin) for dozens of different cheeses — all of them unavailable. When Cleese asks at the end if they have “any cheese at all”, here’s the response:
No, sir, not a scrap. I was deliberately wasting your time, sir.

 As another major snow storm
As another major snow storm 