An ongoing dialogue on HIV/AIDS, infectious diseases,
January 7th, 2015
Are the STI Screening Guidelines for Gay Men Overkill? (And Pedro Video.)
 Our “healthcare system” recently distributed a set of guidelines entitled, Primary care for gay men: screening and treatment recommendations.
Our “healthcare system” recently distributed a set of guidelines entitled, Primary care for gay men: screening and treatment recommendations.
It included, among other things, recommendations for screening for sexually transmitted infections (STIs) and anal cancer. The former it adopted from CDC guidelines, which are this this:
Screening at least once a year for syphilis, chlamydia, and gonorrhea for all sexually active gay, bisexual, and other men who have sex with men (MSM). [Emphasis theirs.] MSM who have multiple or anonymous partners should be screened more frequently for STDs (i.e., at 3-to-6 month intervals)
The anal cancer screening guidelines were kind of made up — pretty much like all recommendations for this form of cancer, since we don’t have solid data linking screening to a reduction in cases of invasive anal cancer and/or death. But in essence the guidelines recommend annual screening with anal pap smears for HIV positive men, and to “consider” screening HIV negative gay men every 2-3 years.
(Brief reminder here: Cancer screening — prostate, breast, colon, lung, ovarian, you name it — is kind of a complex issue. That, my friends, is so far the understatement of this baby year. In short, just because we can screen for some cancers, doesn’t mean we should. )
Anyway, the release of these guidelines prompted an email from one of my colleagues, a primary care physician, as follows:
I was reading the guidelines regarding recommendations for STI screening in all MSM (including annual HIV, urethral/rectal GC/chlamydia swabs, pharyngeal gonorrhea swab and syphilis testing) — is this something that you recommend in practice? I have a number of MSM patients in monogamous relationships so my approach has been to screen if new partners, etc. — and I have not been screening for everything, e.g., asymptomatic pharyngeal gonorrhea… seems silly, what’s the evidence?
They are also recommending consideration of anal pap 2-3 years in MSM who are HIV negative… Is that something you recommend? I worry that the benefits of downstream evaluation/treatment are not clear. Thanks so much for your wisdom!
Emily [Not her real name #1]
Moments after this Emily query, along came this, from a different physician-colleague, who is a gay man:
Hi Paul,
Wondering what you think of these recommendations for STI and anal cancer screening for gay men. I can tell you that my PCP read aloud the guidelines from his computer screen during a routine office visit. He did not ask me about specific risk behaviors and did not take a sexual history, but recommended anal pap because “according to the guidelines” I should have it done. Because I respected and liked him so much, I did not object, even though I thought it was a ridiculous waste of time and money. It would be helpful to know the strength of the evidence for doing an anal pap in HIV-negative men.
Charles [Not his real name #2]
So what’s going on here? Why did both these smart doctors — one as a clinician, the other as a patient — question the guidelines?
As usual, when faced with this kind of clinical quandary, I turned to the most brilliant person I know about patient dynamics, challenging encounters, and the mysterious emotional world of the people we see in clinic — our extraordinary social worker Susan Larrabee. Here’s her comment, quoted in full since it gets “right to the heart” of the issue, if I may use a phrase commonly employed by one of my favorite writers.
Is it possible some MD’s avoid difficult conversations (i.e. conversations they are uncomfortable having) by doing tests? And perhaps some of these same MDs are making these recommendations? I’m not above this in my own life, especially with my teenage kids and their visits with their pediatricians… they’re certainly not telling me (or maybe not their doc) everything. That is to say, there are many difficult conversations and many ways to compensate for our discomfort or the discomfort of our patients, with over-testing perhaps being one.
Susan [her real name]
This is, of course, exactly the issue. In fact, if one reads the guidelines carefully, it includes this key phrase: “these recommendations should be tailored to an individual patient’s risk profile.”
In other words, you can modify the screening according to the risk behaviors of the patient — but only if you take the time to assess it. Cynics will say that everyone lies about their sexual behaviors, but do we know if that’s really true? Better to ask and to talk about this stuff than just proceed blindly.
Speaking of brilliant, I enthusiastically agree that Pedro Martinez deserved his first-ballot induction into the Hall of Fame. (OK, admittedly a sudden transition, hence the Dominican Republic flag above.) He was perhaps the most extraordinary pitcher I’ve ever seen pitch live, and I’ve seen this guy, this guy, and this guy too.
Baseball fans, see what you think:
December 30th, 2014
Common Curbsides: The Patient with “Recurrent Zoster”
 Just in time for the New Year celebration, here’s a curbside consult I’ve received several times, probably because the answer isn’t in most textbooks. As usual, the actual question is slightly edited, as well as lightly (and affectionately) annotated:
Just in time for the New Year celebration, here’s a curbside consult I’ve received several times, probably because the answer isn’t in most textbooks. As usual, the actual question is slightly edited, as well as lightly (and affectionately) annotated:
Hey Paul — Quick question [of course] — I have a patient with a history of irritable bowel, otherwise well, who had shingles on her lower back a few years ago, approximately L5-S1. It was pretty bad, but ultimately improved on Valtrex. Since then she’s contacted me several times with recurrent zoster in the same distribution, each time it improves with more Valtrex. She’s not immunocompromised, HIV negative, not on steroids, etc.
Should she be on chronic suppressive treatment? If so, what drug and what dose? And how long should she be on it? Any role for the shingles vaccine? [Hey — you said “Quick question” — not “questions”! She’s only 42.
Thanks!
Anita [not her real name]
There’s a reason doctors have questions about their patients with frequently recurring zoster — it’s because the entity doesn’t really exist. That makes finding guidance for management extremely difficult!
Even a single recurrence is fairly uncommon in the same dermatome — an outbreak may boost native immunity — which is why patients with a history of shingles were not included in the pivotal study of the live zoster vaccine.
Recurrent zoster is rare enough that some question whether it makes sense to give the vaccine to people with a history of shingles, though in my experience these are understandably the patients with the greatest motivation to get vaccinated, so I’m glad the guidelines do endorse this practice. And one population-based study did find that a single recurrences of zoster occurred in people with a history of shingles at about the same rate as an initial episode. Prolonged pain was a risk factor for having another episode.
So if it isn’t recurrent zoster most of these patients are experiencing, what is it? So far all of the cases I’ve been referred have been one of these three things:
- Herpes simplex. This is far and away the most common mimicker. Obviously the skin lesions can look a whole lot like zoster, and since HSV is usually found in the oral or anogenital areas, the clinician and patient just don’t think about it when clusters of vesicles crop up somewhere else. (It’s what our very young patient summarized above had, of course.) Establishing the diagnosis is usually straightforward, either through a careful history or viral culture/DFA of an active lesion. Warning — some people with a history of “recurrent zoster” aren’t too thrilled to hear they have herpes instead, especially of the Type 2 variety, so caution when informing him/her of this diagnosis. All kinds of relationship turmoil can ensue.
- Post-herpetic neuralgia complicated by “neurodermatitis.” I put that last word in quotes, because that really isn’t the most common use of the term, but it truly fits. Here’s what happens — the patient with zoster has, as a manifestation of post-herpetic neuralgia, tingling and itching at the site. He/She then scratches and picks at it relentlessly, until the skin is red and bumpy — which is then mistaken for “recurrent zoster.” These itchy red bumps really look nothing like shingles, and of course are associated with no viral replication, but the location right at the site of prior shingles fools people.
- Wolf’s isotopic response. I’m lucky to have a brilliant dermatologist as a colleague; he clued me in to this oddly named entity, which is a fancy way of saying “a new skin disease at the site of an already healed, unrelated disease.” Turns out herpes zoster is the most common initial skin lesion, and then a whole host of other things can occur in that same site. Despite the name, it has nothing whatsoever to do with radioactivity, but sure will impress your friends if you mention it in casual conversation.
I’m sure this short list isn’t comprehensive, but you get the point. If you and the patient think it’s recurrent zoster happening over and over again, it almost certainly is something else, and the three entities listed above are a good place to start.
December 20th, 2014
New HCV Option Effective, Safe, Well-Tolerated — And Use Will Likely Be Driven by Payors
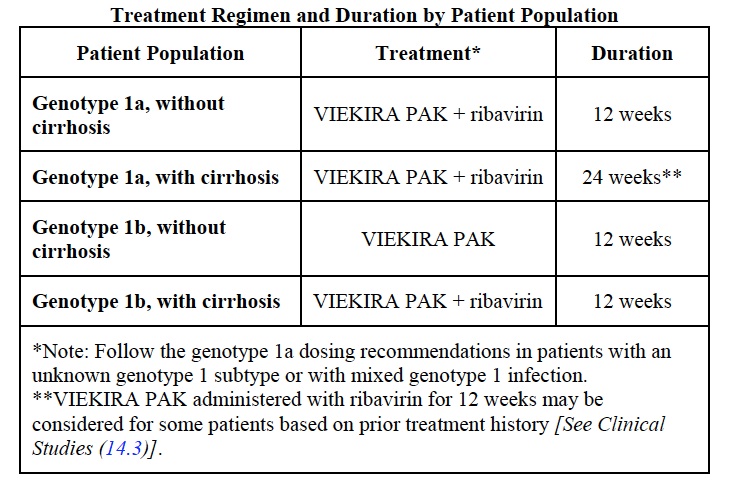
As expected, the FDA approved the next treatment option for HCV on Friday — “Viekira Pak”, a (sometimes complete) regimen consisting of ritonavir-booted parataprevir and ombitasvir given as a two pills once a day, plus one pill of of dasabuvir given twice daily. It is indicated for treatment of HCV genotype 1.
For those of you mechanistically inclined, parataprevir is a protease inhibitor, ombitasvir an NS5A inhibitor, and dasabuvir the first approved non-nucleoside polymerase inhibitor. Ritonavir is there for PK boosting.
Cure rates have been outstanding — 90% and higher — and severe adverse events rare. All good news so far.
So what’s the issue? The full prescribing information is here, but this is the key table:
Obviously, many patients will require concomitant administration of ribavirin, which makes this a considerably more complex regimen than the sofosbuvir/ledipasvir combination pill that has been available since October. Two other disadvantages include more drug-drug interactions (ID/HIV doctors are certainly familiar with ritonavir), and the potential for broader antiviral resistance if the treatment fails.
Whether these make a difference or not in clinical practice is a key unknown. But you can bet good Hanukkah gelt that payors are highly motivated to find out. Here’s some proof.
Hey, Happy 20th Birthday to this classic:
December 14th, 2014
2014 Top Stories in HIV Medicine
Boy do we love end-of-year “Best of …” and “Top Stories of …” lists! Love them! They never gets old! Until January, that is.
My own particular favorites are the Best Movies of the Year lists, since for whatever reason it always seems like some masterpiece slips by. Missed it! So we leave it up to the list-makers, either critics or review-aggregating sites, to remind us. Then we can print out the page, post it next to some Netflix- or other gizmo-enabled viewing device — and, if you’re like me, watch hardly any of the films, since if they were that good and the premise appealed to us when they were first released, then we’d have seen them already in the theater. Oh well.
(While I’m on the topic: There are literally dozens of Best Movie lists to choose from — hey, a list of lists! — just select your source: Rotten Tomatoes, Metacritic — which for the record I like more than Rotten Tomatoes, even though it’s less well known — New Yorker, New Yorker again, New York Times, some other city’s newspaper’s opinion, (LA and Boston haven’t weighed-in yet), IMDB, and Little White Lies, which gave us the nifty video at the end of this post.
Anyway — back to ID/HIV. For the last several years, the nice folks over at Medscape have allowed me to post brief videos on various HIV-related topics, including a “Top Stories in HIV” one each December.
These are decidedly low-budget affairs, shot on a antiquated Flip (remember those?) knock-off and usually set in my dining or living room. Here’s the most recent one, and for a special treat filmed this time on location on Tahiti.
(Actually, it’s my office.)
And since I’ve been told that these clips must be short — optimal length is around 3-4 minutes — allow me use this space to expand a bit more on the choices, roughly divided into Prevention, Treatment, Complications, and Cure. And this brevity definitely doesn’t allow digressions about Best Movies of 2014, or the relative value of metacritic.com vs. rottentomoatoes.com, both of which are probably owned by the same giant media conglomerate anyway.
Sorry, there are only seven. Why is 10 so important anyway?
- A more emphatic recommendation for pre-exposure prophylaxis (PrEP). I initially thought that PrEP was a niche prevention intervention, with the barriers to implementation just too high — the highest-risk patients didn’t get regular health care, compliance would be a chronic problem, and the cost of intervention unsupportable. So what changed? Plenty: a stronger endorsement to use it from CDC; research demonstrating efficacy in gay men even when they are only intermittently compliant; and the results of two other studies (PROUD and IPERGAY, ahem). This has translated into far greater enthusiasm from patients referred to me to discuss the PrEP option — all of the above has made me a believer. Not everyone agrees, of course, most emphatically the head of the AIDS HealthCare Foundation.
- Raltegravir beats darunavir and atazanavir in head-to-head-to-head clinical trial. First presented at CROI 2014, this important study showed that virologic outcomes were the same, but the safety and tolerability of raltegravir meant that overall it was simply better. Note that if subjects wanted to switch therapy — say, for a touch of atazanavir-related jaundice — they were allowed to do so and still stay in study, with the alternative medication provided. This no doubt lowered the threshold for ATV discontinuation substantially, but it is in fact what would happen in clinical practice. Two other quick notes: 1) One could argue that the real winner of this study is, ironically, dolutegravir, which we know is just as good as raltegravir, is once-a-day, and comes in a tiny little pill; 2) this is the kind of large clinical trial that the ACTG does so well — or I should write, did so well, since the research agenda has understandably switched to the next scientific challenges of cure and pathogenesis.
- Two-drug treatment approaches get some traction. While the NEAT study of darunavir/ritonavir plus raltegravir and the MODERN study of darunavir /ritonavir plus maraviroc added still more disappointing data on NRTI-free, two-drug combinations, along came the impressive results of lopinavir/ritonavir plus lamivudine — again just two drugs — in the GARDEL study, showing that less can definitely be more: the two-drug combination was just as effective, and better tolerated. Furthermore, the boosted PI plus lamivudine combination also seemed just fine for maintenance in the SALT and OLE trials. What about integrase/NNRTI as the two drugs? Cabotegravir (744) plus rilpivirine did quite well as maintenance in LATTE-1, suggesting a completely novel approach to less-is-more. This last result has prompted the development of a single tablet of this combination, along with the ongoing work using both of them as long-acting injectables — the LATTE-2 study, for those keeping track.
- Efavirenz associated with a more than twofold increase in risk of suicidality. Ever since efavirenz was approved in 1998, it has been something of a miracle drug from a virologic efficacy standpoint, beating or tying all challengers until it was compared to dolutegravir in the SINGLE study. Sure, efavirenz caused wacky dreams and dizziness, but serious CNS toxicity was difficult to pin down — until now. Acting on a hunch derived from reviewing safety reports from multiple studies, lead-author Katie Mollan designed an analysis that combined several randomized controlled trials, greatly increasing the chance of finding a concerning safety signal, which the paper most certainly did. Results were strengthened by the finding that deaths from injuries or unknown causes were also more common in the EFV-treated subjects. Note that even though the absolute risk of suicidality was low, this is such a serious side effect that it really should give us all pause before prescribing efavirenz to patients with a history of psychiatric illness. (Disclosure — I’m a coauthor on this study.)
- Interferon-free treatment of HCV (finally) arrives. Important because 1) a significant proportion of people with HIV also have HCV ; 2) patients with HIV coinfection now appear to respond just as well as those without HIV (unlike in the interferon days); 3) interferon truly stinks (that was not the first word I typed), and ribavirin isn’t so great either; 4) the first and second generation of interferon-free options — simeprevir plus sofosbuvir then the single-pill sofosbuvir/ledipasvir — are just so amazingly well tolerated; 5) the high cost of something this much better than the existing standard of care raises enormous pharmacoeconomic challenges; and finally, 6) how could the most dramatic advance in treatment of an infectious disease since the discovery of penicillin not be listed as a top story? Enough said.
- Early antiretroviral therapy for cryptococcal meningitis worsens outcomes. The COAT study has pretty much settled this controversial issue, with those given ART early having a 45% mortality at 26 weeks, versus 30% in subjects who waited 5 weeks to start ART. Low WBC in CSF was a particularly bad marker for poor outcome in the early ART group. Right now, cryptococcal and TB meningitis are the only exceptions to the rule that early ART is beneficial in patients with advanced immunodeficiency and AIDS-related complications. It’s likely no coincidence that both are forms of subacute meningitis associated with elevated intracranial pressure, where an increase in inflammation — IRIS — can be catastrophic.
- Curing HIV — it was hard before, now it’s even harder. The relapses of the two stem-cell transplant patients from Boston and the baby from Mississippi underscored that not only will curing HIV be a monumental challenge, but that the necessary step of getting there — a diagnostic test to tell us if our cure efforts are successful — remains an unsolved problem. In other words, all three of these patients had undetectable (or at most extraordinarily low) reservoirs as measured by the most sophisticated techniques. Not low enough, apparently, and not sophisticated enough either. One important thing to keep in mind as this research proceeds: we’ll need to make sure we don’t harm anyone with our investigational cure strategies, as current ART is pretty safe and effective.
Back to Top Movies of 2014, now with a video list. Just put your headphones on first.
December 6th, 2014
Holiday Season 2014 ID/HIV Link-O-Rama
 A little spin around the internet brings us these ID/HIV tidbits, all of them designed to go well with holiday music, egg nog, and potato pancakes, plus a can’t-miss video clip:
A little spin around the internet brings us these ID/HIV tidbits, all of them designed to go well with holiday music, egg nog, and potato pancakes, plus a can’t-miss video clip:
- Flu vaccine match with circulating virus doesn’t look so great. This could mean it’s going to be a tough flu season, but estimates of flu season severity are notoriously terrible. And here’s a un-bold prediction — this news will make the flu vaccine skeptics (patients and health care providers alike) feel more entrenched about not getting or giving the vaccine than ever. Until there’s a shortage of shots in the midst of a bad flu season, that is.
- “The Excrement Experiment” is the title of a highly entertaining article on fecal microbial transplantation (FMT) in the New Yorker. Probably should be required reading for all ID doctors and gastroenterologists, if for nothing else than for the nicknames of the “professional” stool donors.
- Should we reconsider our enthusiasm for PrEP to prevent HIV? Have been holding this one for a while (sorry, it was published a few weeks ago), but it’s one of the best summaries to date describing the conflict between policy makers (such as CDC), who favor PrEP for high-risk HIV negative gay men, and the AIDS Healthcare Foundation, led by Michael Weinstein, who most certainly does not. Comments section demonstrates the strong feelings people have on this issue.
- Even our microbiome gets jet lag says this Cell paper, providing yet another reason why crossing time zones makes us feel so horrible. And not only that, these sleep-deprived bacteria may promote diabetes and obesity. In other words: “These findings provide evidence of coordinated metaorganism diurnal rhythmicity and offer a microbiome-dependent mechanism for common metabolic disturbances in humans with aberrant circadian rhythms, such as those documented in shift-workers and frequent flyers.” Exactly!
- More fat gain with atazanavir than darunavir-based initial regimens. In this small randomized clinical trial comparing ATV/r with DRV/r (both with TDF/FTC), subcutaneous and total fat increased more in the ATV/r arm, along with triglycerides and markers of insulin resistance. This is exactly the opposite of what I would have expected, which is why doing randomized trials is so important!
- Polio crisis worsens in Pakistan. Bad news out of what’s called the “world’s incubator” for this scary disease. (Just ask anyone from the pre-immunization era how scary.) Pakistan has reported 260 cases this year, four times the 2013 number. Blame refugee displacement, political chaos, and a Taliban-held belief that immunization efforts are a CIA-driven, covert Western plot. The glimmer of hope here is that the government of Pakistan is deeply committed to broadening immunization rates, and there is apparently good external aid.
- Is depression really an infectious disease? Could be, says this provocative (but highly speculative) piece in the New York Times. It’s entitled “What if We’re Wrong About Depression?”, and let me answer that question right now — YES WE ARE WRONG, just as we are wrong (or more kindly, “still learning”) about treatment of virtually all major psychiatric diseases. We clearly haven’t figured them out yet. But before we start seeking referrals from our psychiatry colleagues to treat cases of depression with antibiotics, here’s the cited lead investigator’s much more nuanced take: “There’s never been enough compelling data to isolate one or even several infectious agents that are reliably associated with the development of depression.” Sounds right to me.
- Tapeworm parasite slowly eats a man’s brain. No, not a 1950s horror movie, just the cause of this poor patient’s four years (!) of “experiencing headaches and strange smells.” Serial MRIs demonstrated something slowly crawling through his brain, or more accurately, “migration of the lesions from the right hemisphere through the thalamus” to the left. Ultimately, the diagnosis of sparganosis from Spirometra erinaceieuropaei (you knew it all the time) was made by sequencing tissue from a second brain biopsy sample. And check out the coverage of the case report in The Guardian — the “Related Content” and comments from readers at the bottom of the page are intentionally and unintentionally quite amusing (that is, if you’re an ID doctor).
Hey, what a treat — a Colbert interview with the one-and-only Dr. Paul Edward Farmer:
(Seasonally appropriate hat tips to Drs. Carlos Del Rio and Ralph Blair for helpful suggestions. And you can receive a 100% sterile, autoclaved notification of new posts by entering your email address in the subscription box on the right. Our holiday gift to you, free of charge.)
December 2nd, 2014
CROI 2016 Dates Announced — You Read That Right — and What Will We Be Talking About Then?
As any HIV/ID specialist knows, the Conference on Retroviruses and Opportunistic Infections, or CROI, is one of our very best (I think it’s the best) HIV scientific conferences, bringing together basic and clinical researchers for several days each winter in some cold, North American city for high-minded, scholarly pursuit.
But it has historically had a peculiar habit of releasing the dates of the upcoming conference unconscionably late, prompting all sorts of conspiracy theories and sleuthing, some of which I’ve playfully engaged in here.
No more — thanks to Donna Jacobsen from IAS-USA and the organizing committee, last year the CROI 2015 dates were announced before the 2014 conference.
And this year they’ve done even better:
Let the record show that we know the dates of CROI 2016 a full 449 days from now.
And what will the top news from that 2016 meeting be?
November 23rd, 2014
Five ID/HIV Things to be Grateful for this Holiday Season, 2014 Edition
Amidst outbreak hysterias, anti-vaccine imbecility, electronic medical record whining, and slug-related eosinophilia, I bring you this year’s version of the good news — the 2014 edition of Five ID/HIV Things to be Grateful for this Holiday Season, just in time for your holiday turkeys.
(Needless to say, the bird will be properly cooked to ensure it’s salmonella-free, with all cooking surfaces and utensils kept scrupulously free of cross-contamination. Gosh we’re an interesting bunch, aren’t we.)
So a humble and very sincere THANK YOU for the following, in rough order of impact:
- Interferon-free HCV treatment has finally arrived. With the December 2013 approval of sofosbuvir following closely after simeprevir, and the stellar results of the COSMOS study — limitations notwithstanding — we finally had an interferon-free regimen that worked (>90% cure!), and one which was blissfully free of significant side effects. Notably, the guidelines agreed, and this quickly became the most commonly used treatment for HCV genotype 1 in the United States. Then last month the news got even better with the approval of sofosbuvir/ledipasvir, along with a substantially greater body of data supporting its use and a a one-third lower price. Yes, the cost issues remain substantial, which is why I invited a colleague to join me at our Medical Grand Rounds recently to discuss it (you can watch here) — but the bottom line is that these advances in HCV treatment will transform the lives of literally millions world-wide.
- Many brave doctors and nurses are volunteering to assist in the Ebola relief effort. The health care workers who have chosen to go to Western Africa to help treat patients with Ebola virus disease deserve our profound thanks. Think about it: they are volunteering to leave home, volunteering to live in relatively poor surroundings, and most importantly, volunteering to put themselves at the greatest risk of contracting Ebola by caring for the sickest patients, all in the regions without sufficient “staff, stuff, systems, and space”. (That 4-s phrase is Paul Farmer-ism. I might have gotten the order wrong.) Needless to say, lunk-headed quarantine measures, imposed for political reasons or to fan the flames of fear, are not popular among ID doctors. Here’s an interview with Paul describing the Partners in Health relief efforts; you can guess his view on the governor of New Jersey.
- Treatment of HIV continues to look like the best way to prevent it from spreading. TAP might be best known as the abbreviation for Air Portugal, and the cardiologists might use it to describe transesophageal pacing, but to us ID/HIV specialists, it stands for “treatment as prevention”. The great news is that even 3-plus years after the publication of the 052 study, the data continue to show that effective HIV treatment all but eliminates transmission of the virus to others. An example: a study from CROI 2014 not only demonstrated that the rate of HIV transmission from on-treatment individuals to their uninfected partners was zero (caveat: there were confidence intervals), it also introduced many of us to the term “condomless sex.” And let’s face it, that kind of sex is here to stay, whether we like it or not!
- Fecal microbiota transplantation (FMT) not only works for recurrent C diff, but it is becoming the treatment of choice. Once all of us got over the “eww” factor (probably overrated to begin with), practitioners have increasingly made FMT available for patients with recurrent C diff — which is a very good thing because the treatment actually works. That’s more than we can say for these cobbled-together antibiotic tapering regimens, for which the supporting evidence was scant at best. The logistics of how best to go about delivering the healthy bacteria to these imbalanced colons still need sorting out, but one could envision something like these frozen poop pills — “poopsicles”, anyone? — as a prescription item in the not-too-distant future.
- Incentives for antibiotic development seem to be bearing fruit. In 2012, the Generating Antibiotic Incentives Now, or GAIN, provisions were signed into law with bipartisan (fancy that) support, extending by 5 years the exclusivity period for novel antimicrobials before generic competition. Whether this ultimately will be a good law or not remains to be seen, but it certainly is stimulating much-needed antibiotic development for drug-resistant bacteria. This year we saw three new agents active against gram positives, tedizolid, dalbavancin, and oritavancin; coming soon will be ceftazidime-avibactam and ceftolozane-tazobactam, both gram-negative cephalosporin-beta lactamase inhibitor combinations. Interesting overview of drugs in development here.
A few runners-up: The slow but certain end of the Western blot for HIV testing, conjugate pneumococcal immunization decreases childhood admissions for pneumonia, chikungunya cases might be declining in the Caribbean, and the CROI dates are now known well in advance (academic and vacation schedulers around the world thank you!).
What are you thankful for this late November 2014?
November 16th, 2014
Electronic Medical Records and the Demise of the Useful Medical Note
 Electronic medical records (EMRs) are much on my mind, as last week at Medical Grand Rounds Robert (Bob) Wachter, chief of the medical service at UCSF, gave a brilliant talk on the unanticipated consequences of our move towards what he calls the “Digital Doctor.”
Electronic medical records (EMRs) are much on my mind, as last week at Medical Grand Rounds Robert (Bob) Wachter, chief of the medical service at UCSF, gave a brilliant talk on the unanticipated consequences of our move towards what he calls the “Digital Doctor.”
Bob has thought a lot about this issue, so much so that he’s about to publish a book on the topic. In his talk, after a brief history of how we got to where the vast majority of U.S. physicians use EMRs, he focused on three main consequences:
- The fact that doctors now interact as much (if not more) with screens as they do with patients — the “iPatient” phenomenon. The no eye contact problem. The lack of doctors on the medical wards, as we gravitate toward “work rooms” full of computers. You know how pediatricians sometimes get drawings from their school-age patients that include the doctor? He showed a remarkable example, in crayon of course, of a doctor facing away from the artist (the child), the MD staring at a computer screen and typing. From the book: “I’m guessing this one didn’t make it onto the doctor’s Wall of Fame.”
- The loss of interaction between doctors when the data are digital rather than something you can hold. Remember that brilliant radiologist who used to go over all chest films on your medical team? Now a radiologist may be reviewing films at home overnight, or in India, reports filed digitally and not requiring any human-to-human contact with the ordering doctor. Radiology rounds are slowly disappearing, along with the time for clinicians to pause — and think collectively — about what the images mean.
- The potential for automated systems to amplify medical errors. We’ve grown increasingly reliant on computers to help with decisions, for better and worse. In a taut, complex story involving a series of increasingly unlikely errors, he described how a child received a massive overdose of medication during hospitalization — all the indirect result of how a poorly designed systems can usurp clinician autonomy.
What he didn’t have time to cover (but does so in the book — he shared the excerpt with me), is the powerful effect EMRs have had on clinical notes.
It’s a fact that the note as means of communicating how the patient is doing has all but been destroyed. Notes even from the best clinicians routinely have the following features:
- A massive amount of repetition. Cut/paste phenomenon #1.
- “Required” elements that serve no clinical purpose. How useful is a lengthy review of systems? And isn’t a history-directed, targeted physical examination of far greater value than a comprehensive one “done” merely to meet higher billing criteria?
- Giant chunks of computer-generated data. Cut/paste phenomenon #2. It’s mostly lab and imaging results, with no interpretation of what the data mean.
- Factual errors. Cut/paste phenomenon #3. In the ambulatory record, one of my favorites is that some children never age: “Has three children, a son age 10, daughters ages 8 and 1” — which is then written unchanged in the social history over the next five years. Reminds me of The Simpsons — Bart, Lisa, and Maggie never age either. On the inpatients, we routinely see this: “ID consulted, considering pneumonia, UTI, C diff, disseminated fungal infection as cause for fevers” — then these same words are repeated for many days after some or all of these diagnoses have been ruled out.
- Sentences whose sole purpose is to avoid getting sued. You know ’em when you see ’em. They sound defensive, are depressing to read, and communicate no useful clinical information.
- Boilerplate text of highly dubious relevance to the individual case. During a mandatory “compliance” review of my notes (shudder — is there anything in modern medicine more painful?), I had someone suggest I add the following phrase to all of my notes: “More than 50% of this 30-minute visit was spent counseling the patient on the chronic nature of his/her condition, the rationale behind the laboratory tests ordered, the importance of taking medications directed, and the directions for making follow-up visits. Contact information provided, and patient’s questions answered.” The rationale? “You don’t do a procedure, so you need to improve the documentation of what you’re doing with your time.” Lovely.
The genesis of this problem, of course, is that the medical note is trying to do too many things at once. Previously a way of summarizing the clinical course of the patient, both for our own individual use and to communicate with other clinicians, it now has other masters with different motivations. Facilitated by EMRs, the note has subsequently evolved into a Jackson Pollock-like canvas of disjointed text, much of it of marginal or no clinical significance, with sections held together only loosely by the name and medical record number at the top of the page or screen.
Here’s a solution that will never happen — let’s have the medical note evolve even further, breaking it down into distinct sections based on their primary purpose. Imagine three tabs on the top of the note; you get to read only the one you want or need:
- Clinicians, here’s your section — it includes the stuff you really want to know, such as the history, exam, and lab/imaging results that matter (not all the labs/imaging, thank you), plus what the clinician writing the note thinks is going on, and what he/she plans to do.
- Billing compliance folks, read this part — it will have the required review of symptoms (most of them irrelevant), lengthy rubber-stamp documentation of counseling and education, and whatever other parts are required by whatever payor this patient has. And it will be inserted there by someone who’s not a doctor — or even better, by some automated bot — because successfully generating this kind of documentation is not why we went to medical school.
- Medicolegal guys, this is for you — lots of defensive phrases here, none of them of any clinical relevance, but they’re here just in case something untoward happens and the case ends up in court.
Have fun.
November 10th, 2014
Common Curbsides: The Tuberculin Skin Test and IGRA That Don’t Agree
 Here’s one I’ve received twice in the past week, plus my answer.
Here’s one I’ve received twice in the past week, plus my answer.
As always, names/some details changed to protect patient confidentiality, plus my annotations in brackets/italics.
Hey Paul,
Quick question [Need I even comment about the “quick question” phrase, and how this unintentionally devalues what ID docs do? OK, I’ve commented, and yes I’m hypersensitive] — one of my patients, a 38-year-old woman from Serbia, is about to start biologics for rheumatoid arthritis [you can see this is going to be a latent tuberculosis testing question from miles away].
She’s not sure if she got BCG as a child [yep, called that one], so I did both [uh-oh] a PPD and sent a quantiferon gold [note this is not the crazy alphabetizing of the branded interferon gamma release assay (IGRA) products, which for some reason is “QuantiFERON®-TB Gold“ or the other one, which just goes with all-caps, “T-SPOT.TB”, and throws a period in the middle — jeeze, marketers]. The PPD is positive at 20 mm, but the quantiferon is negative [of course — otherwise there’s no question]. Her CXR is negative.
My conclusion is that she does not have TB and therefore does not need preventive therapy prior to starting biologics [that’s notable — putting your money down!]. Is that the correct conclusion?
I’m sure this is a very easy question [ah, not so easy after all] as you must get it all the time [second part is most certainly true].
Thank you very much sir [so formal! or maybe he was in the military] for your time.
Archie [not his real name, but it was the name of a dog we had growing up, a long-haired dachshund]
As noted above, nope, not so easy. Let’s consider the variables:
- She’s from a part of the world with a higher rate of TB than we have here. So the prior probability of latent TB is greater than if she was US-born, though it’s not as high as this.
- She’s about to get “biologics”, which by convention means some sort of expensive immunosuppressive drug, probably a TNF-inhibitor. These are of course great potentiators of TB, some worse than others.
- She may have received BCG, which can give you a false-positive tuberculin skin test. But this effect typically wanes over time, and even if she did get BCG, it’s probably not very effective in preventing adult TB.
- The sensitivity of the skin test vs IGRA is all but impossible to determine — because there is no gold standard for latent tuberculosis.
To summarize, the positive skin test could be a true positive, or could be a false positive from the (maybe) BCG. And the negative IGRA could be a true negative, or could be a false negative because it’s not 100% sensitive.
So what to do? Here was my answer:
The problem is that there is no gold standard — either one could be right. You might consider sending a T-SPOT, since it could be a bit more sensitive than the QF. But since biologics are strong potentiators of active TB, in general I’d recommend preventive therapy for a couple of months before she starts it (then completing a full course) since she’s from a part of the world with more TB than we have here.
PS: we had a dog named Archie when I was a kid.
So my question for you TB specialists out there — since this is such a common question, why doesn’t managing it appear in all the various guidelines and textbooks? Or am I missing it somewhere?
And speaking of dogs, it’s been a while since I showed a picture of Louie.
October 30th, 2014
Why the IPERGAY (Yes, That’s Its Name) Study Could Substantially Increase Use of PrEP
Yesterday, the French IPERGAY study of intermittent pre-exposure prophylaxis (PrEP) was stopped early by the Data Safety Monitoring Board, and for the best reason — the evidence demonstrating that it prevented HIV was overwhelming.
For those who read French, here’s the official announcement. (Scroll down for the English.) And for those who can’t believe the name, it stands for “Intervention Prophylactique pour Et avec les Gays”. Of course.
Here’s a short English version of the study: IPERGAY was a randomized trial of intermittent, “on demand” PrEP vs placebo done in high risk, HIV negative, men who have sex with men (MSM) in France and Canada. The specific strategy tested was:
- Two tablets of tenofovir/emtricitabine (Truvada) from 2-24 hours before sex
- One tablet 24 hours later
- Another tablet 24 hours after that one
So a total of 4 tablets over 3 days for episodic sexual activity, with an option for daily use for more frequent exposures.
We saw the pharmacokinetic data from IPERGAY in Melbourne, which showed that this strategy generated blood levels of tenofovir highly predictive of protection, and that appears to be borne out in these results. The full study detail are not yet available, but encouragingly they are reported to be better than iPrEx (the first study of PrEP in MSM). These results, along with the PROUD trial done in Britain — also stopped early for efficacy — substantially strengthen the data for PrEP in MSM.
So will the results increase the prescribing of PrEP? Even though the FDA has only approved tenofovir/FTC for daily use for prevention? I say it will, and here’s why:
- Patients have been asking about intermittent “on demand” dosing since the first day people were even thinking about PrEP.
- Even though iPrEx was a study of daily PrEP, it appears that many study subjects were taking it intermittently — and still were protected if they got drug levels correlating with 4 or more pills/week.
- Compared with daily dosing, this IPERGAY strategy will cost less.
- It will also reduce drug exposure, and hence likely toxicity.
- No one can say “IPERGAY” without smiling. Said with a French accent, of course.
Just like this film clip (it’s Monty Python week). Roll ’em!
(Hat tip to the excellent Myles Helfand for alerting me to the results.)