An ongoing dialogue on HIV/AIDS, infectious diseases,
October 31st, 2021
Interesting and Important Studies from IAS 2021 and IDWeek That Caught My Eye

Vintage Halloween postcard, 1913.
As noted in my previous post, attending virtual meetings poses some serious challenges.
The biggest obstacle: trying to do one’s regular job while periodically checking in (or more likely not checking in) on the meeting. And while I might have been able to pull off some Really Rapid Reviews© after a few virtual meetings, not so for the last two.
So instead, I’ve packaged 2 into 1, hoping this gives you sufficient value for your blog-reading dollar, lack of really rapidness notwithstanding.
Here, then, are some highlights from these two meetings, in a not-so-rapid (but I hope still interesting) review. The International AIDS Society (IAS) 2021 took place in July, IDWeek in early October.
As usual, but even more so now with virtual attendance, I’m bound to miss some important studies. Let me know in the comments what those might have been.
IAS 2021 is first up:
Single high-dose liposomal amphotericin-based treatment for HIV-associated cryptococcal meningitis is just as effective and less toxic than standard of care. This devilishly difficult-to-treat opportunistic infection continues to take a major toll globally, in particular in Sub-Saharan Africa, where this study (called Ambition-cm) took place. The comparator arm (daily amphotericin for a week with 5FC) is both less convenient and has more side effects. Two questions: 1) Can we make liposomal amphotericin and 5FC more widely available? 2) Does this study have implications for us here, where we use two weeks of induction amphotericin and 5FC?
PrEP failures with TDF/FTC may have drug resistance at HIV diagnosis: While the title of the abstract cites “High rates of drug resistance …”, the actual infection incidence was reassuringly rare. This study was done in Africa, giving us a far different view of PrEP than here — 75% women. Out of over 100,000 PrEP users, HIV was diagnosed in 208, and 27 had resistance mutations. Note the higher than expected incidence of K65R, probably because of subtype C virus, along with the transmitted NNRTI mutations.
No selection of INSTI resistance among women in HPTN 084 who acquired HIV while receiving cabotegravir. Good news, and the results contrast with the small rate of resistance seen in HPTN 084 among MSM. One very challenging HIV diagnosis occurred in a woman who had (in retrospect) very early acute HIV (detectable virus but below 40 copies/mL), was randomized to cabotegravir, then had viral suppression and no seroconversion until week 33 of the study. Once this gets into clinical practice, assessments for HIV breakthrough will be challenging! 35/36 of those in the TDF/FTC arm who failed PrEP had suboptimal adherence.
On-demand TDF/FTC PrEP just as effective as daily PrEP among MSM in China. Analogous to the PREVENIR study, here the participants could choose how they wished to take the PrEP — daily or with the 2-1-1 on-demand strategy. In other words, the study was not randomized. An interesting observation — they enrolled MSM who chose not to go on PrEP at all; perhaps not surprisingly, they had the highest HIV incidence.
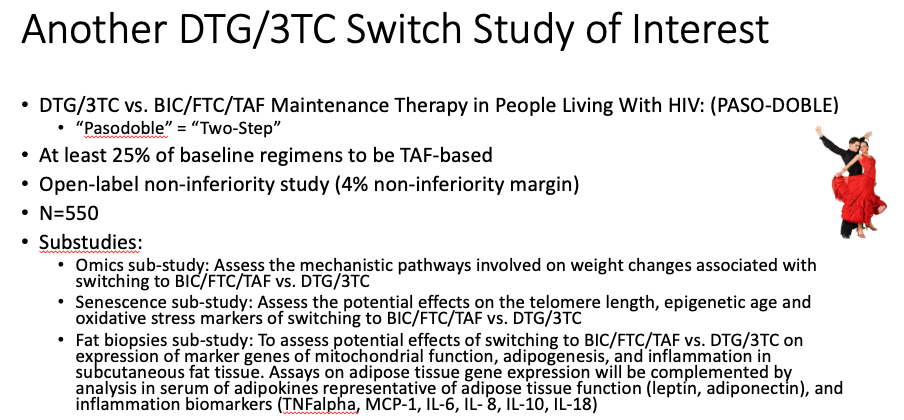
DTG/3TC maintains viral suppression in patients with a variety of baseline regimens. Unlike the TANGO study, where all participants were on TAF-based ART, in this study (called SALSA) they could be on any standard ART regimen, provided no history of treatment failure or resistance. The results demonstrate again that DTG/3TC is clearly a safe strategy virologically for this population. Note that there was more weight gain in the switch arm, likely because around half the baseline regimens included TDF (see first summary from IDWeek, below, for an explanation). An ongoing study — called PASO-DOBLE, get it? — will investigate whether maintenance therapy with DTG/3TC offers objective benefits over BIC/FTC/TAF, such as improvements in metabolic, bone, and various aging outcomes. Here’s a slide summary I made of that study, including the requisite dancers!
Lenacapavir as a subcutaneous injection every 6 months in treatment-naive patients achieves high rate of viral suppression at week 16. There were several different strategies in this phase 2 study which ultimately include two-drug maintenance, but the most novel were those that included lenacapavir given subcutaneously every 6 months (after an oral lead-in) with TAF/FTC. Over 90% had virologic suppression at week 16 (a planned interim analysis); BIC/FTC/TAF had 100%. One case of treatment-emergent resistance to both lenacapavir and FTC occurred in a participant who started treatment with a baseline viral load just over 100,000 cop/mL, implying that the resistance barrier to this novel drug isn’t as high as second-generation INSTIs.
No apparent worsening of outcomes from COVID-19 among people with HIV. This registry-based study included 21,528 hospitalizations, out of which 220 were people with HIV. Given the gazillion studies that have looked at this issue, it’s reassuring to note that not all demonstrate that HIV is a risk factor for more severe COVID-19 disease. My hunch? If you take our healthiest PWH (on ART, viral suppression), and carefully control for demographic factors and comorbidities known to worsen COVID-19, there won’t be much of an effect, if any, of having HIV.
Giving ART to “blipping” HIV controllers improves some immunologic markers. In this observational analysis of 301 controllers followed for a median of nearly 15 years, 90 started ART for various reasons — 83 with viremic “blips” before starting, and 7 with always undetectable viral loads. For those in the former group (the “blipping controllers”), ART led to reduced activated CD4 and CD8 T lymphocytes and total CD8 T cells, and increased CD4/CD8 ratio but did not increase the CD4 cell count. No changes were observed in those who were always undetectable. Whether to treat people with this virologic phenotype remains one of the truly unanswered questions in HIV today.
Patients with a history of K65R from prior virologic failure and currently suppressed on ART switched successfully to BIC/FTC/TAF. The study included 71 people, half of whom also had M184V (hence resistance to both tenofovir and FTC). Viral suppression has been maintained in all of them now followed for a median duration of 47 weeks. These results are perhaps not surprising given the results of the NADIA study with TDF/3TC + DTG in people with treatment failure (many of whom had K65R), but they are reassuring to see nonetheless with this slightly different integrase inhibitor. My colleague Serena Koenig is studying this strategy in a randomized clinical trial being done right now in Haiti. Isn’t it remarkable how NRTIs retain activity even after genotypic (and high-level phenotypic) resistance?
Shifting now to IDWeek, with a few HIV and in particular COVID-19 studies of note:
A meta-analysis of seven clinical trials in 19,359 HIV-negative people shows that TDF is associated with weight loss. The strength of this comprehensive study is that the control arms received placebo, and that any “return to health” (which leads to weight gain) from treatment of HIV is excluded. The mechanism by which TDF induces weight loss is not clear, but we should definitely counsel our patients that discontinuing this drug may lead to weight gain. Some big questions remain — why does TDF do this more in some people than others? What is the mechanism? Is it harmful or salutatory? And — not relevant here, but clearly the case — why is the effect strongest when TDF is given with EFV?
Antibody responses to COVID-19 vaccines may be impaired in some people with HIV. Leading predictors of a good response were CD4 cell count (higher better), suppressed HIV RNA (suppressed better than viremic), and which vaccine was given — mRNA-1273 (Moderna) did better than BNT162b2 (Pfizer).
Another dual monoclonal antibody treatment reduces the risk of hospitalization and/or death in outpatients with COVID-19. The antibodies are BRII-196 and BRII-198, and the effect was in line with other treatments — a 78% reduction in risk. Provided there is no viral escape, I suspect the distinguishing characteristics of these various treatments will be their pharmacologic properties — half-life, formulations, mode of administration, cost. If that’s not enough for you …
Regdanvimab reduced the risk of hospitalization in high-risk outpatients with COVID-19. Hospitalizations occurred in 4.0% of the treatment group, and 8.7% receiving placebo, a 70% reduction in risk. (Amazing how consistent these results are.) Apparently regdanvimab binds to a different location in the spike protein than the other monoclonals.
AZD7442 (Tixagevimab/Cilgavimab) given as pre-exposure prophylaxis to high-risk outpatients significantly reduced the risk of acquiring symptomatic COVID-19. After 83 weeks of follow-up, only 8/3460 (0.2%) of the AZD7442 group vs. 7/1737 (1.0%) of those receiving placebo developed COVID-19, a 77% reduction in risk. Importantly, the study population was not vaccinated, and only 4% were high-risk based on being immunocompromised. Nonetheless, the results strongly suggest that AZD7442 — given as two 1.5 ml IM injections — will be a viable prevention strategy for the not insignificant population of immunocompromised people who have suboptimal responses to vaccines. The company has requested Emergency Use Authorization (EUA) for this indication — there will be many patients eager for this treatment!
Another study demonstrates that casirivimab and imdevimab improves outcomes for hospitalized patients. We’ve known about the survival benefit of this treatment for seronegative patients from the RECOVERY trial for several months. Here a similar finding of benefit — a reduction in mortality — was found for the seronegative patients, with no signal of harm in those who were seropositive. This treatment (better known as REGEN-COV) is now limited in the United States to outpatients at high risk for COVID-19 disease progression, or for post-exposure prophylaxis. The results of these two studies suggest that modification of the current EUA to allow inpatient use, at least for seronegative patients, cannot come soon enough!
Remdesivir for 3 days given to outpatients with COVID-19 significantly reduced the risk of hospitalization. Only 2/279 of those receiving remdesivir required hospitalization, vs. 15/283 receiving placebo, an 87% reduction; there were no deaths in either arm. No effect was observed on nasopharyngeal viral load, raising the question — are we measuring the right surrogate? While giving remdesivir for 3 days to an outpatient to someone with active COVID-19 would be no picnic, these results are in many ways the strongest efficacy data we have for the drug — and underscore that if giving remdesivir to hospitalized patients, it should be started early (inclusion criteria required symptoms for a week or less). The same likely applies to any antiviral agent.
Am sure there are plenty of studies that I missed, but these in particular caught my eye. And for now at least, in-person meetings have started to return, with many (all) also having a remote option — so-called hybrid meetings. Denver will host a hybrid CROI in February 2022, and we just had a hybrid EACS in London, where my friend Joel Gallant attended.
Here’s his front-line experience:
I’m attending the hybrid EACS in London in person, my first face-to-face conference since the pandemic began. It’s strange to be sitting in a large, largely empty conference room watching a bunch of speakers give pre-recorded virtual talks on a big screen. In many cases there’s no one on stage at all. It’s as though the Zoom meeting has been turned into a spectator sport. But at least it’s easier to get a table for lunch than at most conferences.
Don’t you love pandemic silver linings?
Hey, in case you have some leftover pumpkins after Halloween, here’s something you can do with them.


Any ideas about the new Fluvoxamine study? The real deal or another horse paste? Your blog is very useful and entertaining. Please keep it up.
Dr. Sax,
In regards to the IAS presentation on patients with a history of K65R from prior virologic failure and currently suppressed on ART switched successfully to BIC/FTC/TAF- how do we know the F/TAF are actually contributing to any efficacy?
Since patients were suppressed prior to switch to the BIC/F/TAF regimen, can it be that it was the BIC that was doing all the work?
What is the data on continuing the other two drugs? Is their data from other clinical trials that show continuing drugs to which there are resistance mutations still prevents emergence of resistance to the other drugs?
Thanks
Dr Sax,
Just a note on weight gain/loss. Efavirenz is usually taken on an empty stomach at bedtime. So, could this, at least in some cases, explain less weight gain than compared to drugs with no food restrictions?