An ongoing dialogue on HIV/AIDS, infectious diseases,
November 21st, 2022
Five ID Things to Be Grateful For, 2022 Edition
Household magazine, 1952.
In what’s something of a holiday tradition on this site, I hereby present 5 ID things we can be grateful for as we prepare for the best holiday of the year. Why the best?
Family and friends. A nice big meal, with something for everyone. (My family of four has two vegetarians — they have plenty to eat.) No pressure about gifts.
And, most importantly, a chance to express gratitude, something we all should do more often.
I say you can’t beat it, and since this is still my column/blog/whatever (checks over his shoulder), that will be the final decision.
Onto the 5 things, starting with the very most obvious:
1. Trending toward endemicity. No, the pandemic isn’t “over” — especially for people who are immunocompromised, or very medically fragile. And Long Covid remains a persistent challenge and mystery.
But boy has COVID-19 changed.
I speak annually each fall in a Harvard postgraduate course for hospitalists. This is the third year I’ve spoken about management of COVID-19 in hospitalized patients.
The first 2 years, my case-based talk included patients with oxygen-requiring pneumonitis, with discussions about remdesivir, dexamethasone, tocilizumab, baracitinib, and other promising immune-based therapies. Pulmonologists spoke of ventilation strategies and ECMO.
This year? My case for discussion was someone admitted to the hospital with congestive heart failure, “incidentally” found on testing to have COVID-19 — maybe it tipped them over, maybe not. Most of the talk was about outpatient therapies (yes, it’s a hospitalist course — it was a reach), and managing that tricky nirmatrelvir rebound syndrome.
“We might have you pivot back to HIV,” said the course director, inviting me back for next year’s course. That would be just fine!
So while there’s still plenty of COVID-19 out there — and influenza and RSV have come charging back — we appear to be past the stage where our ICUs fill up with COVID-19 pneumonia, forcing our hospitals to restrict their basic functions. Draconian family visitor policies are gone. Some hospitals have even stopped testing all their asymptomatic inpatients.
Fingers crossed it stays this way. After all, it was last year at this time that Omicron hit. I’ve learned, with this virus, not to take anything for granted.
2. Monkeypox is under control. Back in July, one of my colleagues was spending nearly all of her time managing referrals for confirmed and suspected cases of this new (at least to us) sexually transmitted infection.
(And yes, it’s mostly sexually transmitted. I know there are debates about this nomenclature, but that’s for another time.)
It was tough, and her actions were heroic — full PPE for each case. Tecovirimat applications to the CDC. Struggling with Jynneos vaccine shortages. And, worst of all, some cases so severe they required hospitalization.
As the case numbers increased, we had to wonder — when was the steep increase in case numbers going to peak? Anecdotal cases with no apparent exposure, outside of the primary risk group (men who have sex with men), raised the possibility that this scary thing would explode even further.
But thanks to a spectacular collaborative effort by CDC, local public health officials, the gay community, and the roll-out of the Jynneos vaccine, the incidence of this viral infection dropped wonderfully.
Got to love this curve:
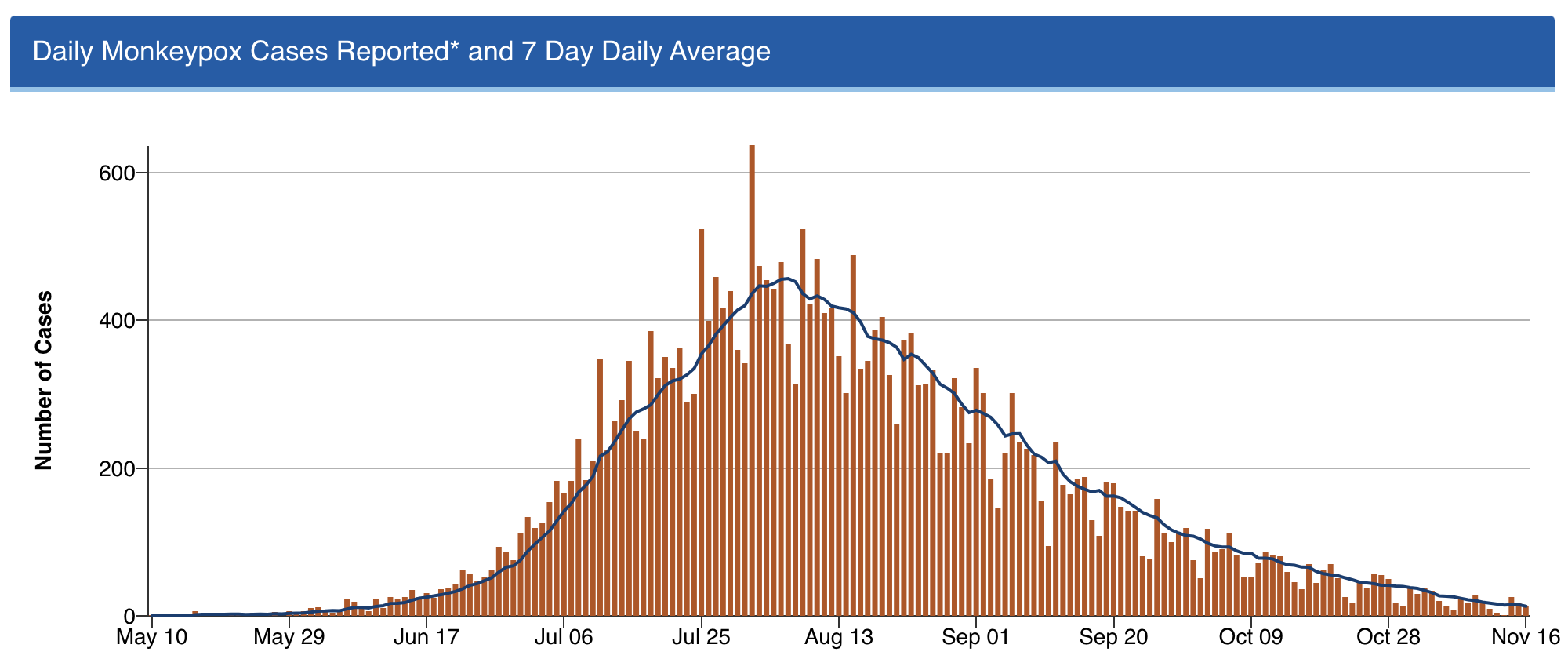
Shout out to Dr. Demetre Daskalakis (among others) — but I’ll give him extra credit as he’s a graduate of our ID program. He was quite the special ID fellow, and is quite the special ID doc!
3. Professional meetings are back — but now with a remote option, too. I spoke recently with someone who attended IDWeek this fall in Washington DC, asking her what she thought about the experience.
“It was wonderful,” she said. “I had a great time.”
She smiled as she said this — almost guiltily, I thought.
It’s an opinion I’ve heard repeatedly from those who went. There was something so strange, yet so exhilarating, about attending. Seeing old friends and colleagues for the first time in years. Marveling at the survival of our specialty, brutal though our experience has been. Sharing what it took to get through it.
But not everyone is ready to go back to these meetings — I understand that. The cost, the carbon footprint, the time away from work and from family — all negatives. And let’s be ID nerds about it, there’s no doubt that interacting with others at professional meetings is a risk factor for transmission of viral respiratory tract infections. Always has been, always will be.
Fortunately, the big meetings seem to understand all this, and now offer the chance to attend remotely. For IDWeek, 7431 attended in person, 2160 virtually.
I would call that progress.
4. Dolutegravir — and by extension, bictegravir — hold up stronger than ever. For those readers who don’t do HIV treatment, here’s little secret — it’s never been easier. Dolutegravir- and bictegravir-based treatment, consisting of these drugs plus tenofovir/emtricitabine (or lamivudine), is so sensationally effective that all but the tiniest fraction of people who take this combination achieve virologic suppression.
(I lump dolutegravir and bictegravir together since they’re quite similar — enough so that there’s even a colossal legal agreement about it.)
It’s worth acknowledging up front that these treatments aren’t perfect. We still have that frustrating weight gain issue, and a signal of possible excess cardiovascular risk. A fraction of people get headaches and insomnia from the drugs, and can’t take them. But by and large these treatments just work — and work better than anything we’ve ever had in the 35 years we’ve had antiretroviral therapy.
Treatment-naive and treatment-experienced. Resistance to the NRTIs or no resistance. Viremic or suppressed. Young and old. Advanced HIV disease or asymptomatic.
Sure, there are exceptions. If you push any drug too hard, with suboptimal adherence, or super high viral loads and severe immunosuppression, or drug interactions, you can select for resistance. In the NADIA trial of people failing second-line therapy, dolutegravir plus 2 NRTIs was noninferior to darunavir/ritonavir plus 2 NRTIs, but 9/235 in the dolutegravir strategy developed resistance, versus zero in the darunavir arm. The world is now conducting a massive conversion of most HIV treatment to “TLD” (tenofovir-lamivudine-dolutegravir), and it will be critical to follow this roll-out to explore the incidence of this resistance, the risk factors, and the optimal management.
But so far, in clinical practice, resistance to these second-generation integrase inhibitors is a rare enough thing that most experienced HIV clinicians have at most a handful of such cases in their practice. And we essentially never see it when people with virologic suppression switch.
Oh, and by the way — that concern about dolutegravir exposure during conception and neural tube defects? Gone! Thanks to the primary investigators, who accumulated a ton of more data since the first report in 2018, the incidence is now comparable to that with other ART strategies. Dolutegravir is now a recommended treatment for all pregnancy categories.
That last fact alone is worth some serious gratitude.
5. #IDTwitter — still a wonderful and entertaining place to learn.
Yep, chaos at the top notwithstanding, it still is.
But that’s the topic for my next post … provided the site is still running when I write it!
Hey, if you ignore the #EndOfTwitter stuff, the content on here remains pretty great https://t.co/O73xiLS6ZI
— Paul Sax (@PaulSaxMD) November 18, 2022
Happy Thanksgiving, Everyone! What are you grateful for this year?


Came for the gratitude, stayed for the confused dachshund puppy! Thanks for sharing!
Among many items for which to be thankful, I thank you for your blog. I cannot begin to tell you how I enjoy and look forward to whatever you write. Though simply a retired rural Iowa family doctor, I want to learn, and your concise wisdom is a marvel. And whether baseball or canines, your wit and observations always bring a smile.
Delightful Paul. Thanks as always.
That puppy is me every time I started a new rotation in medical school.
About dolutegravir based treatment being rolled out to the world, I feel a downside is the need to double the dose if on rifampin for TB treatment, which is the number one OI out here where I am.
Ditto about being grateful for you and your blog, Paul! More broadly, so grateful for ID specialists willing to take the time to speak to media and cogently share their expertise with the public — but especially grateful that you combine gorgeous clarity and paramount expertise with a delightfully positive and generous personality (stop blushing) and if it’s partly graphomania that drives you, so glad you suffer from it…