An ongoing dialogue on HIV/AIDS, infectious diseases,
December 26th, 2015
A Few Things We Were Talking About On Rounds …
 Remember when people passed out papers of interesting clinical studies and relevant reviews? And how some doctors even had a special stamp they put in the upper right hand corner?
Remember when people passed out papers of interesting clinical studies and relevant reviews? And how some doctors even had a special stamp they put in the upper right hand corner?
OK, full confession — I did that. A lot. See evidence to the right. Haven’t used the thing in well over a decade, surprised I still have it. Amazingly, it still works, though the print is getting somewhat faint.
But why did I do that? Some indirect way of getting credit for the literature search-library run-photocopying? A way of preventing reprint theft? (Never much of a crime.) Just too lazy to write out my (very short) name? I do have terrible handwriting.
Kind of ridiculous, when you think about it for a moment.
I thought of this bygone practice since I just finished some time on service, and mentioned various studies while on rounds. Passed out zero papers, for the record.
But to prove to the excellent fellow with whom I was working that the studies weren’t just made up, here are a few that came up:
- Dalbavancin is the long-acting lipoglycopeptide that is FDA-approved for skin infections , the two doses separated by a week; oritavancin is approved for just single-dose therapy. But this study of skin and soft tissue infections suggests that dalbavancin given as just one dose is just as effective as the two dose regimen. It also doesn’t require the lengthy infusion time of oritavancin — only 30 minutes for dalbavancin, 3 hours for oritavancin.
- Toxoplasmosis treatment is much in the news these days, thanks to the 5000% pyrimethamine price hike — and the always entertaining and recently arrested former CEO of the company that owns the rights to the drug. The price increase has forced many of us to adopt what most other countries (and the transplant docs) have done for years, which is to use trimethoprim-sulfamethoxazole for toxo — an antibiotic that is cheap, readily available, and can be given either IV or PO. But what’s the dose? This small randomized clinical trial used 5 mg/kg of the TMP component q12h, and found it was better tolerated and just as effective as pyrimethamine and sulfadiazine; this dose is also listed in the OI Guidelines, and it comes out to 2-3 DS tablets twice daily. Some recommend twice this dose based on other studies. Regardless, take that, Mr. Shkreli!
- Leuconostoc is not only one of the few gram positive cocci intrinsically resistant to vancomycin, it’s also not reliably sensitive to linezolid. And boy does it sound weird — a bacterium named by Russians? Who named it while working in Vladivostok? Treatment of choice is penicillin, but susceptibility testing is critical since resistance can occur. Macrolides, tetracyclines, carbapenems are also usually active. Here’s a recent case report of successful treatment with tigecycline.
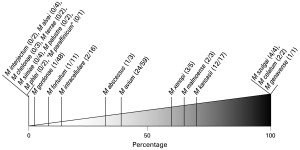 Mycobacterium gordonae is a slow-growing non-tuberculous mycobacteria that can sometimes cause clinically important infection, but is much more likely to be a colonizer or contaminant — figure to the right is proportion of pulmonary isolates that caused real disease among NTMs in the Netherlands. M gordonae is commonly found in tap water, and also is infamous for causing pseudo-outbreaks through its propensity to colonize bronchoscopes, ice machines, cleaning devices, etc.
Mycobacterium gordonae is a slow-growing non-tuberculous mycobacteria that can sometimes cause clinically important infection, but is much more likely to be a colonizer or contaminant — figure to the right is proportion of pulmonary isolates that caused real disease among NTMs in the Netherlands. M gordonae is commonly found in tap water, and also is infamous for causing pseudo-outbreaks through its propensity to colonize bronchoscopes, ice machines, cleaning devices, etc.- Penicillin-sensitive Staph aureus is on the rise! Here are the percentage of MSSA that are also penicillin-sensitive according to WHONET (H/T to Michael Calderwood):
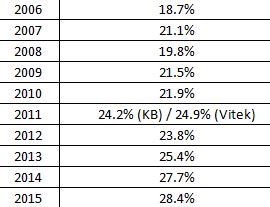 Our hospital has similar rates. No one (I don’t think) has any idea why this is happening — theories welcome. And we continue to be surprised by the latest endocarditis guidelines, which recommend nafcillin or oxacillin for all MSSA regardless of penicillin sensitivity — though many experts (including those who taught me) will choose penicillin if susceptibility is confirmed, since it is more active in vitro, and there is this suggestive study. The key is that the micro lab just needs to do the extra step of confirming absence of inducible beta lactamase — not difficult, and potentially clinically relevant.
Our hospital has similar rates. No one (I don’t think) has any idea why this is happening — theories welcome. And we continue to be surprised by the latest endocarditis guidelines, which recommend nafcillin or oxacillin for all MSSA regardless of penicillin sensitivity — though many experts (including those who taught me) will choose penicillin if susceptibility is confirmed, since it is more active in vitro, and there is this suggestive study. The key is that the micro lab just needs to do the extra step of confirming absence of inducible beta lactamase — not difficult, and potentially clinically relevant. - Nitrofurantoin should not be prescribed to patients with creatinine clearance < 40 due to lower efficacy and increased toxicity — accumulation of toxic nitrofurantoin-derived metabolites can occur. That means it’s not an option for the 90-year-old woman admitted with a UTI and a creatinine of 1.6 (which for the record calculates to an estimated creatinine clearance of around 20). Great recent review of nitrofurantoin here, which is particularly helpful since use of this drug has increased enormously since the change in the UTI guidelines and the rise in fluoroquinolone and TMP-SMX gram negative resistance.
Hey, hope the holidays brought you got some wonderful presents — something better than these items in the video below, which could be less useful than my stamp thing (which at least takes up almost no space in the back of my desk):
[youtube http://www.youtube.com/watch?v=FgFeVlw2Ywg]


I’d go with a much more positive spin. Whenever I marked a paper before giving it to someone, it was to prompt the receiver to get back to me with their thoughts. I.e., to start a discussion. I’d guess that was your motive also, because you are still doing that here: inviting discussions.
The ubiquitous nature of electronic publishing may be reducing scholarly discussion. I no longer send papers to anyone unless they specifically ask: “Do you know of any research on . . . ” In fact, when I recently sent something on leadership theories to a colleague after a lengthy discussion, his reply was: “Why did you send this to me?” Well, alright then . . . nevermind.
I admit to pestering colleagues (both academic and clinical) with interesting, important and/or just plain cool articles. Most of the time, they at least have the courtesy to act appreciative, and one or two seem to get as excited as I am.
Interesting paper from Baystate Medical Center on rise of PCN sensitive Staph aureus. 3-fold increase over a decade.
http://www.ncbi.nlm.nih.gov/m/pubmed/26342027/
Thanks Dr. Sax for mentioning the rise in PSSA. It is a fascinating phenomenon and as one commenter pointed out, there are sporadic reports of the same thing happening in Central MA, Montreal, Los Angeles and even the UK. To complement this, most readers of the blog are probably aware of the several large surveys from various health systems in the US documenting a fall in rates of MRSA nationally. There are numerous hypotheses to explain this but none have been proven definitively. An especially intriguing line of thought is whether the fall in MRSA is somehow related to the rise in PSSA. This is difficult to prove for a number of reasons, but the first step would be to see whether the increasing prevalence of PSSA is a local or general phenomena. Unfortunately, with the advent of newer anti-MRSA antibiotics and a prevailing assumption that the vast majority of S.aureus is resistant to penicillin, many clinical microbiology labs no longer test for this drug. This is a practice truly worth re-considering, particularly if 20% of isolates could potentially be susceptible. Its favorable pharmacokinetic profile and narrow spectrum make it an excellent treatment choice, assuming the absence of an inducible beta lactamase.
While research has (rightfully) focused on studying the biology and epidemiology of MRSA, defining a versatile living organism by resistance to a single antibiotic fails to capture the complex and often orthogonal factors that go into explaining its population behavior and on a practical level would better inform the design of infection control measures. I would very much welcome further research into the population epidemiology of Staph aureus as a whole.
Thanks!
I used to write my name in red ink so I could distinguish my copy of the paper from the duplicates I handed out. If it’s red, I want it back. Now, I hand out many fewer papers, but on a good day, I put web links in my note or e-mail them to colleagues. Sometimes, these are appreciated, sometimes not; I still remember handing a paper to a medical student, who immediately threw it in the trash, right in front of me.
Regarding penicillin-sensitive Staph, I was also taught it was the drug of choice, not surprising because I was taught by the same people who taught Paul. But my microbiologists tell me that testing can be tricky and not so reproducible, which I believe was the rationale for recommending against the use of penicillin in the new guideline.
One strange reason to report penicillin susceptibility is the unfortunate confusion among a few clinicians over the meaning of amp/sulbactam susceptibility in S. aureus. Some of the less astute ones may mistake that for ampicillin susceptibility. If they see “ampicillin …… R” in the report, that error is less likely. Our lab gets around this by reporting amp/sulbactam susceptibility only as a footnote, probably not often read, to the oxacillin result.