June 10th, 2020
Resident Wellness Doesn’t Need to Be Expensive or Elaborate
Daniel Orlovich, MD, PharmD
“We’re not like Stanford” she said to me as we sat next to each other during our breakout session. My cheeks reddened. Somehow, suddenly, I felt as if I became the embodiment of my entire institution. And my furrowed brow revealed my surprise.
Her tone softened. “What I mean is, resident wellness is easier when the program has money. Your program has money. We, though, don’t have the funds for it.”
I looked toward the corner of the room as I thought about this statement. It was interesting. So I decided to examine this a little bit more thoroughly.
Does resident wellness require a large financial commitment?
A Study
A large academic general surgery program created a program that delivered a care package to residents, at work or at home (J Surg Edu 2020; 77:13). This package included essential medications, vitamins, nutrition, and hydration. Residents themselves could request a package or colleagues could send one to them.
All (100%) of the residents felt that this package addressed an unmet need in residency and also felt that the supplies helped them recover faster. The majority of packages, 83%, were requested by colleagues, rather than self-requested. The recipients’ narrative comments focused in on feeling valued and supported, and having a feeling of belongingness.
And here is the most important part – each package cost $7.
The Take-Home Points
First, this study suggests that interventions for resident wellness need not be expensive or elaborate. It is time we reevaluated the kneejerk association of wellness with fancy retreats and expensive counseling sessions. A phone call, a text message, a handwritten note, or even a heartfelt verbal acknowledgment of hard work goes a long way.
Second, this study reiterates what is already well-known and established in the literature — residents won’t ask for help. It is time we design interventions that go to the residents. Or, allow co-residents and family members to take an active role on behalf of the resident. Most residents I’ve been around want to work hard. They don’t ask to be excused — they ask to be supported.
Third, the intervention is targeted. It provides what is needed and at the right time. No more ‘one-size-fits-all’ approaches that residents themselves didn’t vote on or ask for. On the surface, the care packages might seem reductionist and simplistic. The authors themselves acknowledge that burnout is multifaceted and this study only addressed one aspect of burnout. But the point here is that what the care package communicates is incredibly powerful:
Residency is hard and the system is complex but you are valued. We care about you in a meaningful way that is useful to you. We want to support you in your journey to be a better physician.
Conclusion
So to be clear, resident wellness doesn’t necessarily require a large financial investment. It can be a simple, targeted, low-cost intervention that goes to residents and meets an unmet need as determined by the residents.
What low-cost interventions have you seen? Continue the conversation @SolvngResBrnout
June 3rd, 2020
Will the Real Doctor Please Stand Up?
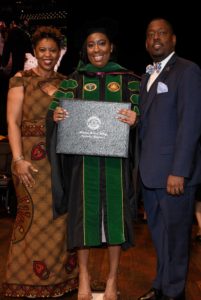
Allison Latimore, MD

Dr. Latimore is the Education Chief Resident at the MedStar Washington Hospital Family Residency Program in Washington, DC
I stood in the hospital elevator yawning and rubbing my eyes, waiting to get off on my floor. A woman looked over at me and said, “Congratulations.” I began to look over my body. Did I look pregnant in these scrubs? Did I have on my real engagement ring instead of my silicone ring? After a few seconds of wondering why she could possibly want to congratulate me, I asked, “On what?” She looked at my physician badge and said, “Your job.” I was stunned. Here I am. Frustrated with working long hours. Unable to realize my position of privilege in that moment. There have been moments in residency that I’ve had people of color tell me how proud of me they are. I’ve had little girls tell me that they want to be like me when they grow up. But the reality is, I struggle to believe that I even belong in this career.
You Are the Doctor?
I am a short black woman, in her 20s. When I walk into an exam room with a white coat on, so many patients tell their relatives on the phone, “Hold on. The nurse is here.” My personal favorite is being called a baby doctor, because at least I still look young. I’ve stood on a hospital floor reading an EKG with a stethoscope around my neck, and have been asked, “Are you the secretary?” The person who asked was the night secretary reporting for her shift.
It’s hard for me to go along with some of the simplest things in medicine. For example, some of my colleagues don’t wear white coats for a myriad of good reasons. When I’m in the hospital, I feel it is necessary to wear a white coat, because a badge that says, “Physician” or “MD” is not enough to remind people that I am indeed a doctor. There are people who feel that referring to yourself as Dr. to others in the medical field or to patients is pompous or reserved for attendings, but I feel I need to, just so people understand my role in their care. I’ve had a patient ask me if I was legally a doctor before just observing an in-office procedure. There have been times when I’ve been disrespected by colleagues or others in the medical field, and I can’t help but wonder why they felt it was okay to speak to me in that way. Is it because I’m young, black, a woman, all of the above, or am I being overly sensitive because of the aforementioned reasons?
Pay it Forward
For every uncomfortable situation, there have been positives. I have had the opportunity to mentor at my alma mater and to share my story, my setbacks, and my successes with students to encourage them to pursue this career.
As of March 2019, ≈300,000 out of the ≈1 million doctors in the U.S. are women. I feel that it is imperative to tell the truth about this path, because I didn’t come from a lineage of physicians. I was a 5-year-old with a dream to become a doctor, whose parents never stopped believing in her when she stumbled. I was fortunate to make connections with people who helped me figure out my path, and I feel a responsibility to do the same for others. Even with 3 degrees, a closet with multiple white coats, and a stack of ID badges for different hospitals and offices, I sometimes still don’t feel like I should be here. Some days, I don’t feel qualified to be writing this blog. But for whatever reason, I am here. So how do I get over the feeling? I know that anyone can feel like an imposter in this profession. If you did, how did you get over it? Does it just take time? I’m still looking for answers!
May 27th, 2020
Virtual Residency Recruitment in the Time of COVID
Prarthna Bhardwaj, MD
COVID-19 has undeniably altered life as we know it. As if getting into residency wasn’t hard enough already, COVID has made it a notch harder. Graduate Medical Education across the nation is preferably adopting video interviews for a virtual residency recruitment. This noncontact change was further endorsed by the Association of American Medical Colleges (AAMC).

What are some of the implications of this? It is pertinent to look at this from two different perspectives — the applicants’ and the programs’.
Financially — More Viable
One of the greatest advantages of virtual recruitment is the time and money an applicant saves on travel and accommodation during interview season. On average, depending on number of interviews, applicants spend between $1000 and $5000. Not having this expense is a nice breather for medical students who already have heavy loans on their backs!
It goes without saying that programs will be saving a ton of money as well. A large portion of money that is usually spent goes towards social events, including pre-interview dinners and lunches and breakfasts on interview days. This is especially important for programs that already had lower funding and budgets for recruitment. One hopes that residency programs will offer virtual pre-interview social interactions with residents.
More Interviews?
There is a chance that programs might choose to interview more applicants, given that applicant behaviors will be more difficult to gauge, to maximize their chances of filling their slots. Virtual recruitment might also allow for multiple interviewers to be available, thus allowing programs to interview larger numbers of applicants. This could mean more interviews for each applicant.
Culture of the program and the ‘fit’
The flip side of a virtual recruitment, for both applicants and interviewers, is that it might be difficult to get the ‘vibe’ of the program and know if the fit is good. ‘Fit’ has anecdotally been rated consistently high among students who are choosing a residency program. Applicants might find it difficult to learn how happy the residents in the program are, unless the program offers virtual socializing opportunities.
For applicants, it will be incredibly hard to show personality in just 20 to 30 minutes on video chat — opportunities to socialize will be much more limited. This means that you will have to shine during your interview – you better have your elevator pitch ready!
Video Fatigue
Having resorted to Zoom for virtual educational conferences this spring, I can say for certain that there is something exhausting about staying glued to a computer screen and remaining engaged. After about 40 minutes, I want to stretch. Worse still, I am looking down at my phone if the content is not stimulating and interactive enough.
Video fatigue could be an even bigger problem for interviewers who are interviewing several applicants consecutively. To avoid it, one should ideally be taking breaks between each interview and should do no more than 2 hours of interviews consecutively.
How do FMGs fit into the picture?
Personally, I believe that Foreign Medical Graduates (FMGs) are at a slight disadvantage, compared with their American counterparts, during virtual recruitment. A few things for FMGs to consider: Can you even travel to the U.S. right now? Some countries are restricting all travel. Is your home country in a time zone that would make interviewing difficult? (For example, a 11am interview with a U.S. East Coast program would be a 9:30pm interview for an applicant in India.) Programs and applicants will need to be mindful of time differences. How is the Internet connection in your country? Not every country has uninterrupted and great Internet to ensure smooth functioning of the interview itself. .
Tips for Applicants During Virtual Recruitment
Regardless of advantages or disadvantages, the mantra to a successful recruitment season during COVID is to embrace the unknown. Here are my top 5 tips to prepare for a virtual recruitment:
-
The set-up
Ensure you are in a well-lit room with a neutral background. Several video interfaces like Zoom allow you to choose a virtual background or even blur the background. It is also vital to choose a quiet space where you will not be disturbed. Try to avoid distractions. While some interviewers might be charmed by children crying in the background, not all will appreciate it.
Ensure you have good internet access and a reliable desktop or laptop, of course. Nothing is worse than choppy internet video. While programs might be understanding of technical difficulties, they are more likely to remember the encounter for the wrong reasons.
-
Dress the part
This is a virtual interview, so dress the part, just as you would for an in-person interview. A lot of people love to wear pajamas on the bottom and their formal attire on the top. We all know what happened to Will Reeve on Good Morning America. Trust me, you do not want to be that person during your job interview. Make sure you are well-groomed.
-
Body language is everything
- Avoid the temptation to look at yourself on the screen. Instead, look directly into the camera to allow for direct eye contact.
- Use a stationery chair — swivel chairs are distracting.
- Have a balanced power pose! If you have not heard about power posing, watch this TED Talk by Amy Cuddy.
-
Keep your virtual identity professional
In today’s digital world, your email address or username is often your first impression. Don’t give the interviewer a reason to question your professionalism before they even meet you by providing a once-hilarious high school email address you still might be using. Keep your email and usernames simple.
-
Prepare ahead of time
Ask a friend, your advisor, or a mentor to do a test run with you to make sure someone other than yourself can assess your performance. In addition, saving time in travel should allow you to research a program more thoroughly. So have good questions ready for the interviewer!
Tips for Programs During Virtual Recruitment
Here are my top 5 tips for programs:
-
Make your program stand out
One of the biggest challenges for a program showcasing the culture of the program. Pre-interview dinners served this purpose traditionally, so programs are going to have to think harder about how to stand out virtually. Some ideas are ‘Virtual Happy Hour’ or ‘Virtual Teatime’ with the residents or perhaps even a dedicated themed chat channel. You can make a short video of ‘a day in the life of an intern’ to provide more realistic appeal. Involve your residents — ask for ideas to make your program stand out!
-
Put your candidates at ease
Reach out to applicants and give them a rundown on the details of their interviews, just as you would if they were coming to talk to people onsite. These are times of high stress and uncertainty for everyone. Some useful things to share are:
- Tips on how to access the videoconferencing technology and whether applicants need to download any software.
- Your team’s expectations for the interviews.
- A timeline that details when interviews will start and end along with name and title of each person applicants will meet.
Finally, as an added precaution, give them a backup phone number to reach you, in case there is a glitch. Ask them to share the same with you.
-
Go with the flow
Expect to have internet and connection issues. In addition, applicants often live with spouses, children, and pets. If life interrupts the interview or a dog is barking in the background, candidates should not be penalized. Use a little extra compassion and thoughtfulness during these challenging times. Be flexible and forgiving as an interviewer.
-
Your Digital Presence
Put simply, Digital Presence is the space that your brand owns online. Some ideas for that are:
- Create an Instagram or Twitter account for your program if you do not already have one. Celebrate your residents and ensure you post at least once a week. Applicants are often more tech savvy that you are. Talk to them in their own language.
- If you do not have a great website, now is a great time to update it! With applicants having limited social interactions with your residents, they are more likely to resort to your website, Doximity, SDN, Reddit – you name it! Consider having resident testimonials and resident bios on your website.
-
Be prepared
Carefully read the applicants’ resumes and personal statements beforehand. As an applicant, I appreciated interviewers who have made the time to discuss the finer nuances of my personal statement. This also adds a nice personal touch to the interview, which is especially important now.
And the Virtual Recruitment Season Starts … Now!
In conclusion, we are learning new ways of leading our daily lives in this era. Being flexible yet professional is key to combating the stress of virtual interviews. I cannot wait to see how the virtual recruitment season will turn out for applicants and programs alike.
Feel free to shoot me a tweet @prarthnavb for more comments and thoughts.
April 30th, 2020
Why Is Burnout Still Occurring, Even with Work-Hour Restrictions?
Daniel Orlovich, MD, PharmD
“Daniel, this guy is one… sick… puppy,” he stated emphatically, drawing out the last three words.
I put my phone down and turned my chair away from the computer. He had my attention. Not because I haven’t taken care of any sick patients before, but because this statement was coming from him.
I’m sure your hospital has someone like him (or her), too. A physician who stays up to date on the current literature yet has enough experience to know the previous guidelines and recommendations. One who really has ‘seen it all’ and remembers when the old wing of the hospital was new. A colleague who others curbside to glean insight, which he gladly shares. And of course, the highest compliment of all — someone who is trusted to take care of other physicians’ family members.
His tanned face leaned in as he told me about this patient who was getting ready to go to surgery. Looking down at his beige and hunter green hiking boots, it dawns on me — I’m in a moment. This type of patient, this type of case, this type of responsibility with someone of his caliber could only make me a better physician.
But then something happened. The case got pushed back. A few hours later, it was pushed back again. Pretty soon it was morning. The patient didn’t go to surgery that night.
“What could have happened?” I thought to myself, as I stopped by Starbucks. I was looking to indulge in a little more caffeine to make up for the lost learning opportunity. Just then my phone vibrated: “CASE TO GO LATER THIS AFTERNOON,” the page read. And, the case finally did go that afternoon. And also long into the night.
The Connection with Resident Burnout
What does this story have to do with resident burnout? When it was all said and done, I was at the hospital much longer than the ACGME recommended limit. And, despite this, I felt less burned out, rather than more burned out.
Resident burnout is more than hours worked. In the situation above, I clearly went beyond the arbitrary hour limit. That artificial number, in the midst of a complex, large, and imperfect system, was crossed. But to focus solely on a number fails to take into account other important drivers of resident burnout.
To be clear, hours worked is an important factor. And this piece is not about the “hours worked” debate. It’s easy to point out when something is excessive. It is harder to define when something is right. Of course, hours worked is an easy metric to track, but it provides an incomplete assessment.
Solely focusing on hours worked drives a wedge between those who trained before and those who trained after work-hour restrictions. I completely understand that some of those who trained before the limits have trouble understanding how hours have gone down, but resident burnout currently is at epidemic levels. There is no doubt that the training system has improved, yet we are still mired in a suboptimal environment.
Four Domains of Burnout
To obtain a more complete understanding, I conceptualize the drivers of resident burnout into four categories – physical, mental, emotional, and moral. By framing the conversation strictly around hours worked, only the physical domain is addressed and the others are neglected.
The other domains:
Mental: E.g., How does my mind keep up with the pace of the day?
- The average patient’s length of stay decreased from 14 days to 4.8 days from 1983 to 2009.
Emotional: E.g., Is the system tolerating harassment?
- Sexual harassment was the most common form of abusive behavior in training programs with about 36% of residents reporting it, according to a systematic review (Acad Med 2014; 89:817).
Moral: E.g., Am I here to connect and serve another human being or to document and bill?
- Research specifically focused on Internal Medicine residents suggests the ratio of documenting to direct patient care might be as high as 5:1 (Ann Intern Med 2017; 166:579).
So why did I feel better after taking care of a complex patient, despite being at the hospital past the recommended hour limit? Using the framework provides the answers. Mentally, I knew that I had built on my foundation of knowledge. Over the past 4 years, I have been incrementally and appropriately given more challenging cases. I was prepared for this case. Emotionally, I felt incredibly supported. My attending even shared a cookie from the attending-only lounge with me. It sounds trivial, but that gesture personified the solidarity we had throughout the night. He made sure I had enough time to grab a drink of water. He knew I was up for many hours and asked me if I was still able to provide good care. And he supervised me closely — with various checkpoints throughout the case — to see if my words matched up with what was needed. I knew I could say at any time that I wasn’t fit to continue — and there would be no retribution. Morally, I felt the patient was receiving high-quality care. The communication amongst teams, coordination with other services, and plan were thoughtful, deliberate, and done in accordance with best practices. I felt respected as a person when the program paid for my Uber ride home as my adrenaline faded away.
Perhaps we spend too much time focusing on the hours worked. It is a part of the picture but not the entire picture. I cannot tell you the perfect amount of hours worked. By overly focusing on that question, we fail to take into account other pertinent influences. We can all agree that past a certain point, the educational value of more hours is suboptimal. But again, where is that point? And how does it apply to my specialty compared with yours? And how do we define the value of hours as a newly minted intern versus a nearly graduating soon-to-be attending?
It is time to consider interventions that address the other domains that drive burnout — physical, emotional, and moral. These interventions must address the pressing and timely concerns of modern training. In addition, they should be effective and high-yielding without requiring a complete retooling of the system nor a large financial commitment. The next logical step of addressing resident burnout is to consider these other domains and incorporate practical and targeted solutions.
April 24th, 2020
Pass or Fail — USMLE Step 1
Allison Latimore, MD

Dr. Latimore is the Education Chief Resident at the MedStar Washington Hospital Family Residency Program in Washington, DC
We All Take Tests
In January 2020, it was announced by the US Medical Licensing Examination that USMLE Step 1 scoring would change from a 3-digit score to pass or fail. I’m sure some budding and current medical students are jumping for joy. Some residents and attendings probably are brooding jealously, thinking of all the stress, depression, and anxiety that they developed or exacerbated as a result of Step 1 testing. I’ve heard people say, “if you are a doctor without anxiety, something is wrong.”
A large part of the anxiety that medical students and doctors face stems from the constant testing. We take the MCAT, NBMEs, USMLE Steps 1-3, subject boards, in-training exams, and, finally, boards for our specialty. All of those exams are necessary to become a board-certified physician. Personally, I felt that every time I turned around, I was inputting my credit card information to pay for a new test. As inconvenient as it is, being tested constantly as a physician is necessary. People want to know that the person treating them is intelligent and up to date on the latest research. However, have we proven that all these standardized tests correlate to how “good” a doctor someone is or their potential to become a good doctor?
Good Doctor or Good Medical Student?
According to a study published in the Advances in Medication Education and Practice Journal in April 2019, “USMLE Step 1 and Step 2 CK scores moderately correlate with the number of honors grades per student in core clinical clerkships. This relationship is maintained even after correcting for gender, institution, and test-taking ability. These results indicate that USMLE scores have a positive linear association with clinical performance as a medical student” (Adv Med Educ Pract 2019 Apr 26; 10:209).
Why the change from a 3-digit score to pass/fail, if this test correlates with how well people perform in medical school? The USMLE released the following statement from Humayun Chaudhry, DO, MACP, President and CEO of the FSMB, in regard to the policy change: “These new policies strengthen the integrity of the USMLE and address concerns about Step 1 scores impacting student well-being and medical education. Although the primary purpose of the exam is to assess the knowledge and skills essential to safe patient care, it is important that we improve the transition from undergraduate to graduate medical education.”
Peter Katsufrakis, MD, MBA, President and CEO of NBME, stated, “The USMLE program governance carefully considered input from multiple sources in coming to these decisions. Recognizing the complexity of the environment and the desire for improvement, continuation of the status quo was not the best way forward. Both program governance and staff believe these changes represent improvements to the USMLE program and create the environment for improved student experiences in their education and their transition to residency.”
Transition to Residency
I must confess, my initial response to this change was jealously that this didn’t happen while I was crying incessantly over Step 1. Then, I began to read some of my colleagues’ thoughts on social media. I read people recount their suicidal thoughts after Step 1. I also read about people who had no issues with Step 1 at all and who couldn’t relate to these feelings. What surprised me were the people who disagreed with the change completely. At first, I could not understand why anyone would disagree. But when I think of minority students, students aiming for very competitive residencies, and international medical graduates, I realize that 3-digit score is the key to their destiny. Some feel that the one way to separate themselves from the others in the stacks of residency applications lies in a 3-digit score — which is not wrong. People who don’t have a big-name school behind them might count on their step 1 score to get them into the door. What sets your application apart from anyone else with a pass?
Long-Term Effects
It’s possible that this change will push medical schools to change their curriculums and schedules. Will students need to take Step 2 CK early enough to have an impressive 3-digit score to match into their desired specialty? Will this make medicine even more of a “who you know” field? Away rotations already are expensive for students. Will everyone need to complete more away rotations to increase their likelihood of matching? I’d love to hear your thoughts. Do you think changing Step 1 scoring to pass/fail will be conducive to the medical school experience or detrimental?
March 5th, 2020
Should We Avoid Exposing Residents to Coronavirus?
Eric Bressman, MD
Dr. Bressman is a Chief Resident in Internal Medicine at Icahn School of Medicine at Mount Sinai in New York, NY
The arrival of the novel coronavirus to the U.S., and the inevitability of its eventual spread, raises an interesting question: Should we avoid exposing residents to the virus?
 Before we try to answer this question, we should start with some important qualifiers. While a good deal about this novel virus remains unknown, the majority of cases appear to be low risk, particularly for the demographic of the average resident. Furthermore, if this outbreak does reach pandemic levels, exposure to healthcare workers of all levels ultimately will be unavoidable. Finally, even with the best of protocols in place, it will be impossible to triage out every potentially infected patient at the point of first contact.
Before we try to answer this question, we should start with some important qualifiers. While a good deal about this novel virus remains unknown, the majority of cases appear to be low risk, particularly for the demographic of the average resident. Furthermore, if this outbreak does reach pandemic levels, exposure to healthcare workers of all levels ultimately will be unavoidable. Finally, even with the best of protocols in place, it will be impossible to triage out every potentially infected patient at the point of first contact.
With all this in mind, COVID-19 may not be the best case study, but it’s an interesting opportunity, nonetheless, to pose a broader question regarding the role of trainees during epidemics and pandemics.
History
Let’s start with a brief historical overview of this question. Physicians have always been at the frontlines of deadly outbreaks, and as a result, were regularly infected by the same diseases as their patients. The first century of U.S. history can be recounted in a sequence of epidemics, from yellow fever to cholera to typhoid fever. In an era of unregulated medical and graduate medical education, and limited understanding of the spread of these diseases, there was scarcely any thought given to the protection of students and trainees during these outbreaks.
The first century of U.S. history can be recounted in a sequence of epidemics, from yellow fever to cholera to typhoid fever. In an era of unregulated medical and graduate medical education, and limited understanding of the spread of these diseases, there was scarcely any thought given to the protection of students and trainees during these outbreaks.
Graduate medical education evolved over the course of the twentieth century from a mix of apprenticeships and a limited number of more structured programs, to a landscape of predominantly hospital-based internships, and eventually specialty-focused residencies with a unified accrediting body. Important questions that persist to this day were considered during this time, including the place of the resident on the spectrum from student to employee.
The AIDS epidemic was likely the first major infectious disease outbreak during which the unique experiences of students(Health Educ Res 1999; 14:1) and residents (Ann Intern Med 1991; 114:23) were explored, although the emphasis tended to be on the duty to treat in spite of the fears and perceived risk. In the intervening decades, however, the vulnerability of the trainee has been reconsidered, and this has shifted the conversation. By the time of the 2014 Ebola epidemic — although different in scale and mode of transmission from HIV — much wider efforts were undertaken to protect trainees from potential exposure, prompting a healthy debate (Acad Emerg Med 2015; 22:88).
Pros
We can entertain a couple arguments in favor of trying to protect residents from a potential pandemic exposure:
- The infection control argument: Because residents are mid-level providers, any patient a resident sees will also be seen by a supervising attending. To limit total number of exposures and mitigate the potential for disease spread, the fewest number of providers possible should see any at-risk patient.
- The student versus employee debate: During the Ebola epidemic — which was vastly different from the current pandemic — nearly all medical schools forbade students from providing care for rule-out Ebola cases (Acad Emerg Med 2015; 22:88). There may not be one unifying theory about why these policies were developed, but the reasons probably include insufficient training, liability, and a less than clear moral imperative. Conversely, faculty are compelled to care for all patients, at times even in the face of personal risk, by virtue of their training, their contracts, and their professional codes of conduct (Am J Bioeth 2008; 8:4). The question, as always, is where residents fall on this spectrum; this has been argued both ways over time, often according to what is most convenient for the employer.
Cons
At the same time, some real downsides might occur in trying to shield residents from potential exposures:
- Missed training opportunity: This is especially true when it comes to outbreaks that require rigorous infection control practices, as was the case with Ebola. If rule-out protocols exclude trainees, health systems will be less likely to invest resources in training them. This may, in fact, put residents at higher risk, both now and in the future.
- Modeling professionalism: Residency is about attaining not just the knowledge and skills, but also the attitudes, necessary for life as a physician. At times, this encompasses embracing some risk in the service of our patients. Whatever the status of residents — student, employee, or student-employee — there might be value in imparting this message.
Conclusion
The role of the resident during a pandemic raises interesting questions; although they generally operate at the front lines, the instinct is there to protect them when personal risk is involved. COVID-19 might not be the best case study for a number of reasons, but it is more than just a thought experiment. Health systems are developing protocols at this very moment, and the role of trainees will be an essential consideration. In some instances, the protective instinct of a particular attending might be to handle the rule-out cases personally. But most importantly, the next pandemic might pose even greater risk, and it will be all the more essential to find the right balance between expectation, education, and limitation.
February 26th, 2020
Medicare for All: The Healthcare Our Nation Needs
Frances Ue, MD, MPH
Over a month into the new year and feels like the world around us is in grave peril. There are many reasons to lose hope: the climate crisis with Australia’s wildfires, the evolving COVID-19 epidemic, the acquittal of the President’s impeachment charges, and the list goes on. Combined with long hours, sick patients, and seemingly never-ending grey skies in Boston, it can feel challenging to find goodness in the world.
In search of inspiration, I often turn to my colleagues at Cambridge Health Alliance. One such colleague is Dr. Adam Gaffney, a critical care doctor, public health researcher, activist, and president of Physicians for a National Health Program (PNHP). I had the pleasure of interviewing him for this blog.
(Interview transcript edited for length)
Me: Tell us about yourself. How did you become involved in activist work?
 Adam: Well I’ve been pretty progressive politically for my whole adult life but, during residency, I began to be more active in PNHP. It was a time when concern for inequality was rising, the aftermath of the great recession, occupy Wall Street, really a growing sense in the country that more and more people were being left behind and also clear that health care was a big part of that. I was fortunate enough to be able to join an organization that was on the front lines of speaking about the need for universal healthcare reform, and I’ve been involved in that organization ever since.
Adam: Well I’ve been pretty progressive politically for my whole adult life but, during residency, I began to be more active in PNHP. It was a time when concern for inequality was rising, the aftermath of the great recession, occupy Wall Street, really a growing sense in the country that more and more people were being left behind and also clear that health care was a big part of that. I was fortunate enough to be able to join an organization that was on the front lines of speaking about the need for universal healthcare reform, and I’ve been involved in that organization ever since.
Me: In terms of feeling passionate about Medicare for All and PNHP, can you tell us a little bit about how you discovered this as your passion?
Adam: The idea that healthcare should be a right, and should be a social good, and not a commodity, is an idea that I’ve believed in for as long as I’ve seriously thought about politics and how society should be structured. I think over the course of my medical training, I realized that this was an area where, fairly or unfairly, as a physician, I could have a much larger impact. I also had personal experiences in the course of medical training, that reinforced to me how essential it was to have a system that provided healthcare to everyone by their needs, not by their economic means.
Me: What are the key arguments for Medicare for All and how would it work practically?
Adam: Medicare for All would be a different way of paying for healthcare in this country. Right now, we pay for healthcare in a few different ways. A lot of healthcare is still paid through the government, more than half and that’s because we pay into taxes for things like Medicare for the elderly and Medicaid for low-income people. We also spend a lot of money on public employee healthcare benefits, and there is also the Veteran Affairs (VA), Department of Defense, and other federal, state, and local healthcare programs. Although we spend a lot of money on healthcare through the government, we also spend a lot through the private sector. Private insurance, co-pays, deductibles, out-of-pocket payments, also constitute a large amount of healthcare spending in the United States.
We have this fragmented, multi-payer, partially privatized way of paying for healthcare and the price is that we’ve left:
- 30 million people uninsured
- 44 million people (probably more) underinsured, meaning they have insurance but it doesn’t actually cover the costs of their care
- we’ve generated a profound amount of waste in the form of healthcare bureaucracy.
- We spend more than 800 billion dollars a year on healthcare administration like billing, which is about one third of total healthcare spending
Medicare for All would simplify the way we pay for healthcare rather than putting our money into these various different pools. All the money would flow through a single-payer (the federal government) and hospitals, doctors, drug companies, and everyone else, would be paid for by that single payer. Everyone will be covered with full universal coverage similar to other high-income nations. And because of that, everyone will have an equal level of access to the system. Finally, the way the bills are written and the way the PNHP proposal is structured, it would also eliminate out-of-pocket payments, like co-pays and deductibles. That sounds probably the most radical for many people but the truth is, that is how it works in Canada and the United Kingdom for the most part — you go to the doctor, you get hospitalized, you don’t have to pay out-of-pocket. It can be done, and it can be done affordably.
Me: How were you able to create momentum to create change as a leader and community organizer?

“As Physicians, We Prescribe Medicare for All”: An open-letter — signed by more than 2000 physicians — was published as a full-page ad in the New York Times on January 21, 2020.
Adam: There have been physicians and many others who have been working on this cause for decades. PNHP, for instance, was formed in the late 1980s, and members of the organization have been pushing this agenda ever since. It’s really been in the last 5 years however, that Medicare for All has swung into the mainstream discussion. And there are different reasons for that. I think that on the one hand, we had the Affordable Care Act, which helped a lot of people, but it became clear that it didn’t do enough. On the other hand, we’ve had a rise in popular, progressive politicians like Bernie Sanders in the Democratic primaries. And I think certainly, we’ve had a rise in unhappiness with the amount of inequality in our society.
I think the other reason why we’ve had some success is that it’s becoming increasingly clear that this system is not working well for physicians. And what do I mean by that? Well, physicians are having to spend more and more of their week glued to their computers, doing bureaucratic and clerical billing tasks; things that are really taking them away from the patient’s bedside. At the same time, they and hospitals, are having to hire literal armies of billers and clerical staff to do all these interactions with insurance companies (to get the payments made, to fight for the prior authorizations). It’s really not just draining emotionally and psychologically for doctors, it’s obviously taking a huge amount of resources.
We’ve had success with PNHP helping educate the medical profession about why Medicare for All reform would be very good for our patients, but also pretty good for us, too. And we’ve seen that there has been a change in the medical profession. In January, the American College of Physicians, second largest medical specialty society in the United States, came out in support of universal healthcare and explicitly endorsed Medicare for All. We also published a full-page advertisement in the New York Times, with an open letter, with the signatures of more than 2000 physicians ‘prescribing’ Medicare for All for the nation with some of the most prominent doctors in America, like Dr. Bernard Lown, the developer of the defibrillator, and Dr. Paul Farmer, founder of Partners in Health.
We’ve helped to give voice to a large number of physicians, by some polls, the majority of physicians, who do in fact support single-payer.
Me: Let’s transition from Medicare for All. How did you get involved in research and how have you used research for advocacy?
Adam: I came to Boston 8 years ago for my Pulmonary and Critical care fellowship at Massachusetts General, Brigham and Women’s, and Beth Israel hospitals. And as part of a fellowship, there is a research component. As someone interested in society and inequalities, but also in a pulmonary program, my initial research interests were actually more in respiratory epidemiology; inequalities in lung function. At that point, I also was very interested in health policy and health politics and began to realize that it may be difficult to have these very different sorts of passions. I ended up transitioning into focusing on health services research and I came to Cambridge Health Alliance, in part, because that was the kind of research I wanted to do. We have a group of people here who have long been doing this sort of research and also have long been involved in PNHP.
Since then, I’ve had an opportunity to do some studies that have examined both the ways in which the US healthcare system is not working, which are quite honestly not difficult to find and also to study how a healthcare reform might function. In three studies we did last year, we looked at, after a country moves towards universal coverage, how does it affect the society-wide utilization of healthcare services? How does that impact how many hospitalizations, how many doctor visits are used by society? And we were interested in that because that’s a big question in terms of the cost of reform.
This past January in Health Affairs, we looked at how having VA health coverage affects people going without needed medicines because of cost as opposed to other kinds of coverage. Under the VA system, copays are either very low or zero for medicines, depending on what category you fall into. And for people with other insurances, co-pays and deductibles for medicines can be hundreds or even thousands of dollars a year. So not surprisingly, we found that people with VA coverage didn’t go without needed medications because their costs are much less than those with other kinds of insurance. And it was particularly beneficial for people with low incomes and in racial and ethnic minorities.
Those are a few examples of the kind of work we’re doing which I think is really critical to achieving change. You need high-quality research, you need the numbers, you need the figures, you need to really understand the issues in order to be able to speak up both honestly and intelligently about the problems.
Me: How did you identify mentors and sponsors to help you along your way?

PNHP conference 2019 with David Bor, Danny McCormick, Adam Gaffney, Steffie Woolhandler, Janine Petito, Natalie Shure, Andy Hyatt, and David Himmelstein (L-R).
Adam: I think I was very fortunate to meet people who had shared beliefs and shared commitments. Some of my mentors, like Drs. David Himmelstein, Steffie Woolhandler, and Danny McCormick are people who I met in the course of my work through PNHP, but it turns out that they also did all these other sorts of things that I became involved with as well. I think finding people with a shared vision and shared commitments is a great way to find mentors. And they also should be people you enjoy spending time with as well, which really makes it all much easier.
Me: What’s next in your career?
Adam: The reality is, despite this being in many ways an optimistic moment in those who advocate for Medicare for All, this is going to be a long road. There is an enormous amount of work that still needs to be done for us to have universal healthcare (how will it run, how will it work?) So I think my life and my career is going to revolve around continuing to work on national health insurance and developing the knowledge base and tools, and the research that we need to make it happen. I, and many others, plan on committing ourselves to this as a lifelong pursuit.
Me: With all this experience, what advice would you give trainees who are also hoping to incorporate advocacy work into their careers?
Adam: I think it certainly can be done, but to be honest, it’s not easy as a physician because you’re pulled in many different directions. You have home and work responsibilities. Being a physician is a more than full-time job. The advice I typically give is, throughout your medical career, from medical school onwards, there’s going to be times you have opportunities to engage, there’s going to be other times when say, in the middle of your intern year, you may not be able to. And that’s okay. What you really need to do is not be harsh on yourself when you’re not able to take part in the kinds of things you want to. Just remember, you’ll have an opportunity to get back into it down the road. I think being involved in advocacy does require some sacrifices; you can’t do everything. You have to make some choices about what matters the most to you. But I think that if it’s something you’re really passionate about, you should be able to find a niche, find a position that allows you to do advocacy work. The more that it intersects with your practice or with the people you’re working with, or with your research, the more relevant it will be.
Clinical training is extremely challenging intellectually, but also, personally, and emotionally.
There are issues that we are passionate about and finding the one that speaks to you can actually help you overcome the challenges of training and of being a physician.
Thank you, Adam Gaffney, for kickstarting a series of articles profiling physician leaders, activists, and change-makers; people making a difference in the world of medicine and beyond. Learn more about PNHP and Dr. Adam Gaffney.
I welcome any suggestions for future guests! Leave a comment below or send me a tweet, Frances Ue.
February 18th, 2020
How Can Attendings Affect Resident Burnout?
Daniel Orlovich, MD, PharmD
A Sad Short Story
Harvard medical school. Stanford general surgery training. Northwestern vascular surgery fellowship. Suicide.
This devastating path, taken by a 33-year-old trainee in 2010, is not unique.
- An estimated one physician commits suicide every single day in the U.S. alone (JAMA 2014; 312:1725).
- A number of these lives are taken on the hospital premises, places where physicians feel deep emotional and psychological connections.
- Residents are part of a field which has the highest suicide rate of any profession (CMAJ 2018; 190:E752).
- Suicide remains the second-leading cause of resident death and the number one cause of male resident death in the U.S. (Acad Med 2017; 92:976).
- In 2019, suicide is considered an occupational hazard of medical training.
- Compared with other college graduates, we trainees are 1.6 times more likely to suffer from burnout and twice as likely to feel depersonalized.
- We score lower in quality of life indexes on all sections — mental, physical, and emotional (Acad Med 2014; 89:443).

Photo by Vidal Balielo Jr. from Pexels
Valiant attempts, ranging from reduced working hours to dedicated wellness programs, have been made to alleviate this reality. Such coordinated efforts to prevent both burnout and death frequently focus on individual coping mechanisms. While this strategy has merit, attempts to mitigate unnecessary stressors from our healthcare environment are equally important.
During the past few decades, we have witnessed major changes in training and practice across the U.S. medical system. While being a physician remains an incredible privilege and offers a truly meaningful connection, changes have occurred in the work environment. Notable changes include the electronic medical record, malpractice litigation, and the volume of patient turnover. For example, the average length of patient stay decreased from 14 days to 4.8 days from 1983 to 2009 (J Health Soc Behav 2012; 53:344). Advances in the field have allowed patients to be discharged on postoperative day 1, as opposed to 1 week later. The treatment modalities, imaging, and necessary paperwork have increased. Today, “care” includes extra core elements that go beyond patient contact, including charting, social work, and coordination. Rather than focusing on “hours worked,” it is illuminating to consider what trainees are actually doing and the pace at which it is being done. Interns might spend less than 10% of their time providing direct patient care (Acad Med 2016; 91:827). Once they’ve graduated, today’s medical trainees enter a field that has failed to keep pace with inflation: Compensation has fallen 7.1% from 1995 to 2004, whereas debt burden has risen 270% since 1986.
What Can an Attending Do?
One positive aspect that has not changed is the guidance and impact that an attending can have on a trainee. Traditionally, trainee burnout is framed between two groups: trainees and the system. Based on my experience, I believe that one of the most effective forces to directly benefit trainees, and to help keep burnout at bay, is a third element: the attending-trainee interaction.
Attendings wield significant influence and power, correcting us when we need guidance and praising us for a job well done. As trainees, we look up to them, we learn from them, we want to mold our careers based on their input. With one genuinely constructive comment or action, they can invigorate our day. But one flippant or misplaced remark or action can be disheartening. While large, coordinated efforts such as reducing hours or implementing retreats is a step in the right direction, I believe that simple, low key actions throughout the day serve as the cornerstone in combating trainee burnout. In addition, attendings may glean immense satisfaction from teaching and mentoring, while trainees gain fulfillment from learning. Thus, the entire medical ecosystem benefits.
Try This
From our trainee experience (myself and Dr. Dua, cited below), we propose five actions that might not only mitigate trainee burnout but also benefit the attending by providing a better trainee-attending relationship. These cost no money and minimal time.
- Use a trainee’s name during interactions. It may seem insignificant, but it makes us feel human, provides an instant connection, and allows us to more easily absorb the educational moment.
- Provide a quick debriefing at the end of rounds or a surgery, with both positive and constructive criticism. Guidance is one of the most important things attendings provide and what we, as trainees, seek above all. At times, when the environment is purely service (time constraints or patient severity), a few spent minutes highlighting fundamental learning points and communicating what was done well and what needs improvement is impactful and makes the trainee feel that educational goals were met.
- Acknowledging that some situations are less than ideal, although they cannot be instantaneously remedied, allows the trainee to be heard. Trainees, especially junior residents, spend a good time amount of time coordinating care with phone calls and paperwork. It can be inefficient, extremely time consuming, and anxiety provoking, primarily because it is sometimes at the expense of a high impact and more practical learning opportunity. Major system overhauls would be required to change the current situation, but the work still needs to be done. Acknowledgement of this situation by attendings provides a sense of solidarity, given that attendings also serve our patients in less than ideal system circumstances.
- Say “thank you” to acknowledge trainee input. While there is educational value in dictating a note, setting up a room, or writing a new consult note, a few words of appreciation can add worthiness and make trainees feel like contributing members of the team. No one wants to be praised for every little action. This is not a “participation trophy.” Rather, these tiny words shed light and make the path forward easier to see.
- Ask a trainee how things are going — not just professionally, but also personally. We all know that some of us spend more time with certain attendings than we spend with our own family. This presents an opportunity to form a genuine connection. Asking how or what a trainee is doing once again humanizes this unique relationship and reinforces the attending’s role as a mentor.
Let’s consider the idea that there exists an often underutilized, overlooked, and influential resource in the fight against burnout. Attendings serve as a vital part of trainee education. As young doctors, we are affected by how we are treated by the people who have the most influence. In our experience, five simple remedies can offer consequential change: using our name, providing immediate educational feedback, acknowledging and displaying solidarity in less than ideal circumstances, expressing thanks, and asking personal questions. The attending-trainee relationship is a special sacred one. We encourage attendings to help us fight burnout through support, encouragement, guidance and camaraderie.
Special thanks to Dr. Anahita Dua who contributed to the concept, writing, and editing of this article.