An ongoing dialogue on HIV/AIDS, infectious diseases,
February 14th, 2025
This Year Influenza Came Back to Remind Us It’s Not Messing Around
If it seems like pretty much everyone you know either has the flu or is recovering from it, it’s because we’re in the middle of the worst flu season in over a decade.
Take a look at this figure, from our state’s surveillance data, updated yesterday:
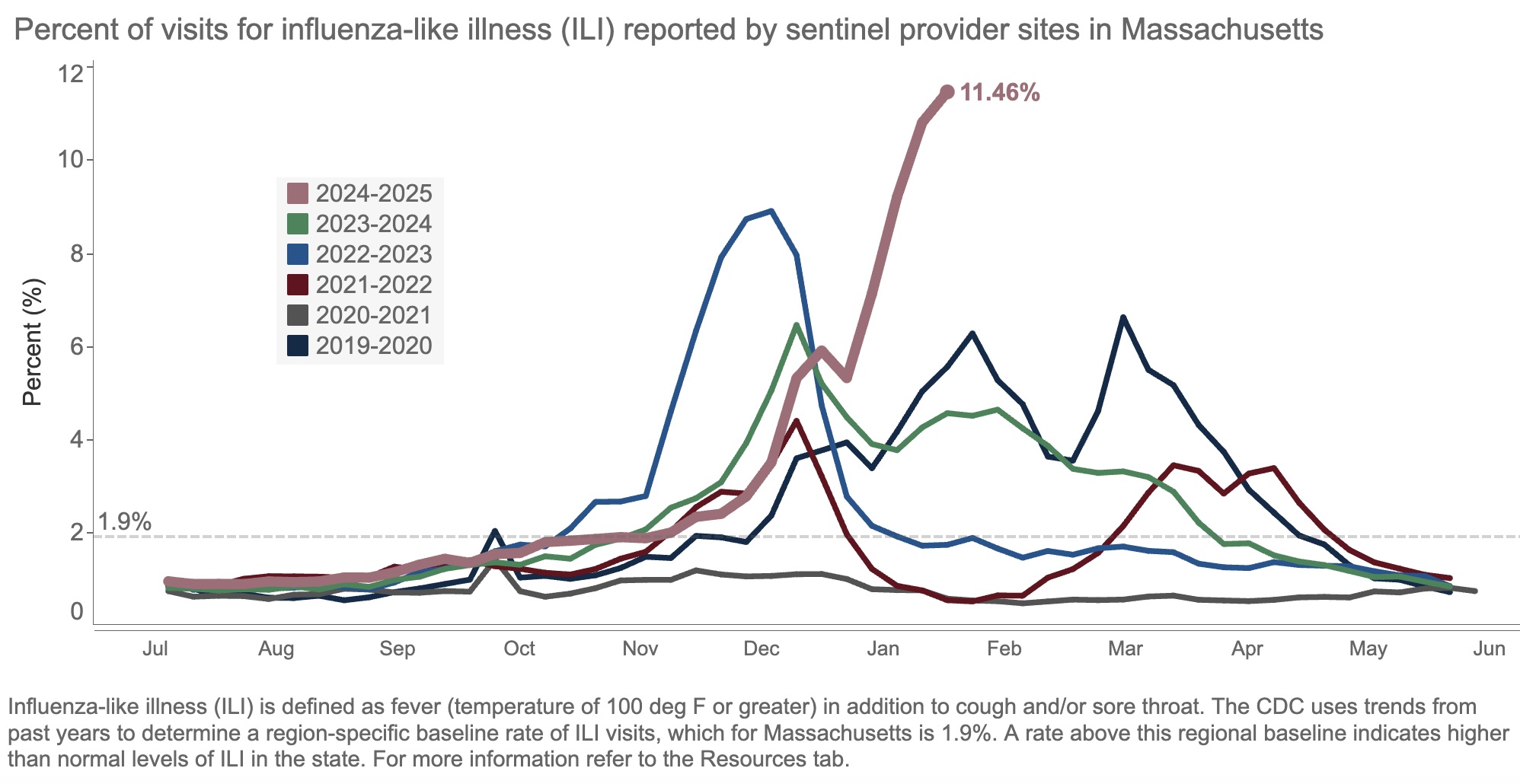
The result of all this “influenza-like illness”? Patients are deluging outpatient clinicians with messages about fevers, sore throats, coughs, and related symptoms. Hospital beds and ICUs fill up with chronically ill people whose condition has worsened due to the flu. Emergency rooms, already overstrained, park sick people in hallways awaiting evaluation and treatment.
Yes, it’s bad out there, folks. This week, we heard that our hospital has four times as many people hospitalized with the flu than as those hospitalized with COVID-19, the first time this has happened since the pandemic.
One of the most common questions we ID doctors get when the flu season is bad, or late, or just strange, is, “Why this year?” The honest answer is this humble three-word sentence:
We don’t know.
Some have blamed the cold weather this winter without much in the way of a significant thaw. Maybe, but other cold winters haven’t necessarily had this much flu. Plus there’s plenty in southern states.
Others cite the low rate of influenza vaccination, in reaction to overzealous (in some views) COVID-19 vaccine recommendations. Perhaps, but this has never been a popular vaccine.
A third theory is the fact that masking and other infection prevention activities in the community have ended. I doubt it’s this because masking was pretty much over last year and even the year before.
Some have asked me if this year’s strain of flu is somehow different, and the answer is that surveillance molecular data do not so far suggest this is the case. This is in contrast to the 2009 H1N1 influenza pandemic, where during April (!) flu cases surged because of the emergence of a novel H1N1 variant to which younger people had little immunity.
Related, one cause of this year’s high number of cases emphatically isn’t a flood of cases of “highly pathogenic” avian influenza, H5N1. Despite active surveillance at the state level, we still are not seeing this illness from this strain to a significant degree — fortunately!
Note that I put the words “highly pathogenic” in quotes. H5N1 is of course of great concern because we have no natural immunity to it. If it emerges as a human-to-human pathogen, we’re looking at an explosion of cases, analogous to or worse than 2009. That’s bad enough.
But another major worry is that it might be intrinsically more virulent, more likely to cause severe disease per case. But the cases of H5N1 reported thus far in the United States from animal sources have had a wide spectrum of severity. At one extreme there has been a death, and at least one ICU admission; at the other end of the spectrum, many have had mild illness (conjunctivitis seems particularly common), and a recent serologic study in 150 bovine veterinary practitioners found 3 positive cases — all asymptomatic.
So I’d propose we remove the two-word phrase “highly pathogenic” as a common modifier of H5N1 until we really know whether it deserves this scary label — not just in birds and cats, but also in humans.
And please, let’s press on with the following:
- Active influenza surveillance, with transparent reporting of data. This recent government action to reduce the CDC workforce will not make this easier. To quote one of my former colleagues who works there right now, “It’s a very sad time for public health.” 100% agree.
- Re-invigorated research to improve the flu vaccine. That universal flu vaccine can’t come soon enough.
- Further drug development to improve flu treatment. Can I interest anyone in interferon lambda again, which was effective in COVID but never developed? It’s a potential treatment for respiratory viruses that may be agnostic to etiology.
Here’s hoping.
The views and opinions expressed in this blog do not represent those of NEJM Journal Watch, NEJM Group, or the Massachusetts Medical Society.


We’ve got to watch H5N1 closely. Absolutely critical.
During the 1918 influenza pandemic we had Woodrow Wilson, confining young men—the most vulnerable—in crowded army barracks and transport ships to fight in Europe. With AIDS we had Reagan, who barely mentioned it except to talk of quarantine. With COVID we had Trump, recommending bleach and ultraviolet light. History may be about to repeat itself. Maybe that’s what it will take.
Dr. Sax, your thoughts on baloxivir?
Is it possible that this year’s vaccine just isn’t as effective, perhaps due to some genetic drift since the vaccine was first formulated?
I think it is important to note that the terminology “Highly pathogenic avian influenza” is carried over from veterinary medicine where it separates the current strains, which cause severe disease and can be lethal to birds, from “Low pathogenicity avian influenza”, which is non-lethal to birds. It was not meant to denote how it affects humans.
You are absolutely correct! Thanks for pointing this out, I learned something after posting this that it applied to birds, not humans.
-Paul