An ongoing dialogue on HIV/AIDS, infectious diseases,
July 19th, 2020
Reaching Out to ID Doctors in COVID-19 Hot Spots — You Must Be Truly Exhausted
 For us ID doctors in most of the northeastern United States (and Chicago and Detroit and some other northern cities), March and April hit us like a giant wave of never-ending calls, pages, emails, and crises.
For us ID doctors in most of the northeastern United States (and Chicago and Detroit and some other northern cities), March and April hit us like a giant wave of never-ending calls, pages, emails, and crises.
With COVID-19 case numbers increasing every day, the challenges crashed down on us in an endless torrent of hospital needs and responsibilities.
The emotional toll of seeing so many critically ill patients for whom we didn’t have any proven therapies was only part of it. We were also the group to whom everyone turned for help — everyone had questions.
We know you must be swamped right now, but … started many a query.
No surprise. This is an Infectious Disease, after all. “It’s what you signed up for,” as one of my friends, a lawyer, put it succinctly with a shrug.
But it’s also something none of us had ever seen in any of our lifetimes. No one is old enough to remember the 1918 influenza pandemic. No one really knows what to do, or how to do it.
Which is why the work of handling COVID-19 can be endless.
Want an example? Someone tallied what one of my extraordinary colleagues — she ran our “biothreats” response team — gave to the COVID-19 effort, which started for her in early March:
Needless to say, it came as an enormous relief when case numbers started to drop. For Boston, this started in early May.
Here’s what Dr. Stephen Smith, writing in late June, said about his experience in northern New Jersey (reprinted with permission):
In my private ID practice in northern NJ, 18 miles west of New York City, we have treated over 200 hospitalized COVID-19 patients, many in the ICU. We peaked in early April. Then in early May, it was as if someone turned off the spigot. Since then, we have been consulted on only 20 patients who tested positive for SARS-CoV-2, but only a minority was admitted with COVID-19 symptoms. We have not intubated a patient with COVID since early May.
We are hesitant to use the “A” word (attenuation). Like the reverse of saying Lord Voldemort’s name, we are worried that if we say the “A” word, it won’t happen.
To what do we owe this lessening of the COVID-19 burden, especially now that cases are increasing in most of the rest of the country?
While herd immunity might play some role — I remain hopeful, despite discouraging reports on low seropositivity in hot spots — much more likely is that we’ve been adherent on a societal level with implementation of various low-tech strategies.
Social distancing. Banning communal indoor activities. Closing bars and restaurants. Asking religious institutions to worship over Zoom, or outside. Wearing masks in public, especially indoors.
These things, you know, actually work.
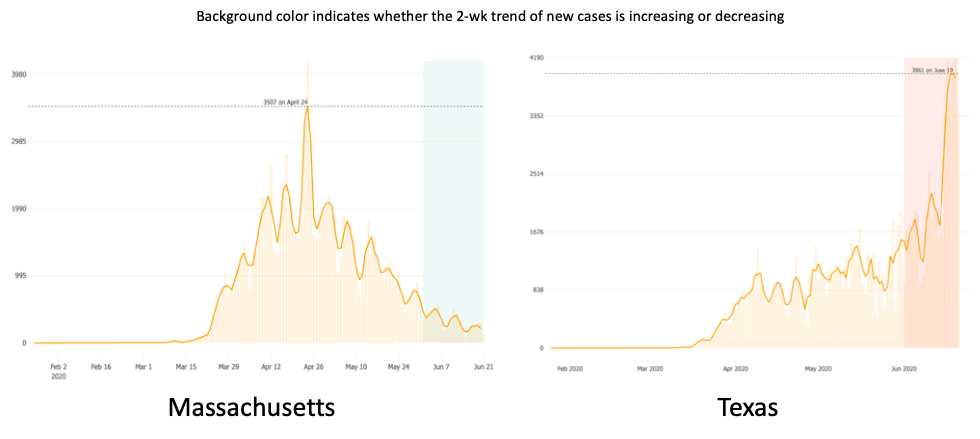
While we ID doctors in the northeast bask in this much-needed reprieve, our ID colleagues in much of the rest of the country — initially relatively spared — now have to deal with rising case numbers.
And they must be truly exhausted. Really.
Because it’s not as if they weren’t gearing up for this in the winter. When CROI (the most important national HIV meeting) converted to a “virtual” meeting in early March, many ID doctors from the south and west had already cancelled their plans to come to Boston — COVID-19 already loomed very large nationally to all us ID specialists, and preparation for it was underway everywhere.
Plus, note I wrote that they were relatively spared — they’ve also been seeing some cases right from the start, if not as many we initially did.
So to all ID docs out there in Arizona, Florida, Texas, California, Alabama, South Carolina, Tennessee, Georgia, Louisiana, and all the other states experiencing a COVID-19 surge, I’m thinking of you.
And so hoping that your community will get it together, and turn off that spigot soon.
Because when it happens, it brings a relief the likes of which you won’t believe.



Hi Dr. Sax,
Thanks for these words. I am an ID in Los Angeles and we’ve had surge and surge of COVID patients since late mid-April with no end in sight. We are all truly exhausted and fear for what a bad flu season plus COVID will mean.
I am so frustrated. We were spared the worst of it in Atlanta thanks for the rapid actions of local elected officials like Keisha Lance Bottoms who ordered everyone to stay at home long before our Governor did. Now those same local authorities are not only not allowed to act but in the case of Atlanta they are being sued for doing the right thing- rolling back “re-opening” and raising masks. We sent a letter to the Governor with the signatures of over 1400 health care workers asking him to require masks and empower local authorities. But he has decided to be malignantly obstinate instead. And the elephant in the room is the completely poor federal response. I’m truly at a loss.
Paul: thanks for your message. Yes, as Jesse Cauk states, down south we are exhausted, frustrated and frankly mad. This should have not been the case but the lack of leadership and of a science based response has come out to hurt people and, unfortunately, as usual, the disadvantaged and marginalized the most.
Just want to give a shout-out to all the nurses, respiratory therapists, CNAs and other staff who are working so hard, too. For some reason, I haven’t seen the media cover the job that RTs do every day for our patients.
The most distressing thing is that this didn’t have to happen this way. I know, I’m preaching to the choir here.
Organizing care for infectious patients should not be a service area. This should be the area of national health protection. This area should be free of charge for all citizens, funded from the Federal budget and have a strict management structure throughout the country. Then the epidemic will go down, and many lives will be saved.
Hello doctor,
Great post. Im a ID doctor in Panama at a third level hospital.
Im part of the covid19 unit in my hospital… Great job.. But we are having some lack of equipment and meds.
A shout out to all the ID doctors out there, keep the good work.
Thank you for thinking of us.really. It is nice to have support from colleagues who actually know what this is like.
Even though we initially had fewer cases (and I have great respect and sympathy for what our east coast colleagues when through), we have still been sprinting full force since march preparing for covid: implementing infection control measures in our clinics and hospitals, updating changing PPE guidance, guiding anxious staff back to work, reaching out to patients, fighting to get sufficient testing access (a huge issue in March which we solved temporarily and is back again), keeping up with CDC and professional society guidance, participating in town halls and task force meetings, and worrying night and day about how to protect our staff, patients and communities (we are in the hard hit southern region of San Diego county).
We are completely exhausted and now we are facing our peak of cases depleted of energy and optimism. And those who are parents are now facing school closures (against expert recommendations) and wondering how to care for our families and while meeting relentless covid demands with no end in sight.
Thanks Paul for thinking about us in South Carolina. Waiting for the beach and bar season to be over and hurricane season to hit. It may still get worse
Thank you for these kinds words, Paul. Out here on the West Coast we saw the beginnings of the surge before the rest of the country and thankfully, our Governor was one of the brave to rapidly adopt the shut downs of non-critical businesses, implement social distancing guidance, masking and all of the public health tools available to us. Because of this our early surge did not reach the proportions seen on the East Coast at least in most places, however, that has all changed now with the refusal of many of our politicians and citizens to follow even the simplest guidance. We have all been working, Zooming, and doing everything else flat out now since mid-March with no respite and little help. Piled onto all of the activities you and others mention has been the effort to launch major randomized clinical trials of new drugs and vaccines in the midst of salary reductions, furloughs, hiring freezes, and public and institutional obstructions. We’re doing it all so far but no one knows how long we’ll be able to continue. I do fear for the well being of our staff, our faculty, our fellows and obviously the patients we all serve.
If we were invaded by a foreign power we would have a draft and muster an army and this is the responsibility of the federal government. But here we are invaded by a an invisible army and the government seems clueless or worse to help the people on the front line. My deepest empathy to the entire medical profession since what you are doing is simply heroic.
Those of us working in areas not considered “hot spots” are also working incredibly hard and having difficulty keeping up. The reality is that the vast majority of the country does not have sufficient Infectious Disease specialists. My partners and I have been working continuously on clinical service in addition to the hours spent on preparedness, answering personal calls from healthcare workers, teaching students/residents and fellows and participating in meetings.
The reality is that we need a better payment system for ID so that more physicians will choose this specialty. I know of no other specialty that is expected to be available constantly and is not reimbursed for those activities.