An ongoing dialogue on HIV/AIDS, infectious diseases,
January 6th, 2019
Rabies After Trip to India, Aortic Dissections with Quinolones, a Vaccine for Candida, Koala Bites, and More: A Welcome-to-2019 ID Link-o-Rama
From the Library of Congress, government shutdown notwithstanding.
As 2018 tips over into 2019, here are a bunch of ID- and HIV-related studies that, for one reason or another, haven’t made their way to this site yet — but still yearn for your attention:
- Cases of infective endocarditis have increased since release of the 2007 dental prophylaxis guidelines. Recall that those guidelines only recommended prophylaxis for patients at the highest risk of IE. The results of this population-based study suggest (but do not prove) that perhaps some moderate-risk patients should also receive antibiotic prophylaxis.
- A woman in Virginia died of rabies after being bitten by a puppy during a trip to India. Though rare, these horrific cases underscore the value of pre-travel counseling and immunizations for certain trips. And dogs (especially puppies) are cute and wonderful, but stay away from strays in countries that still have canine rabies!
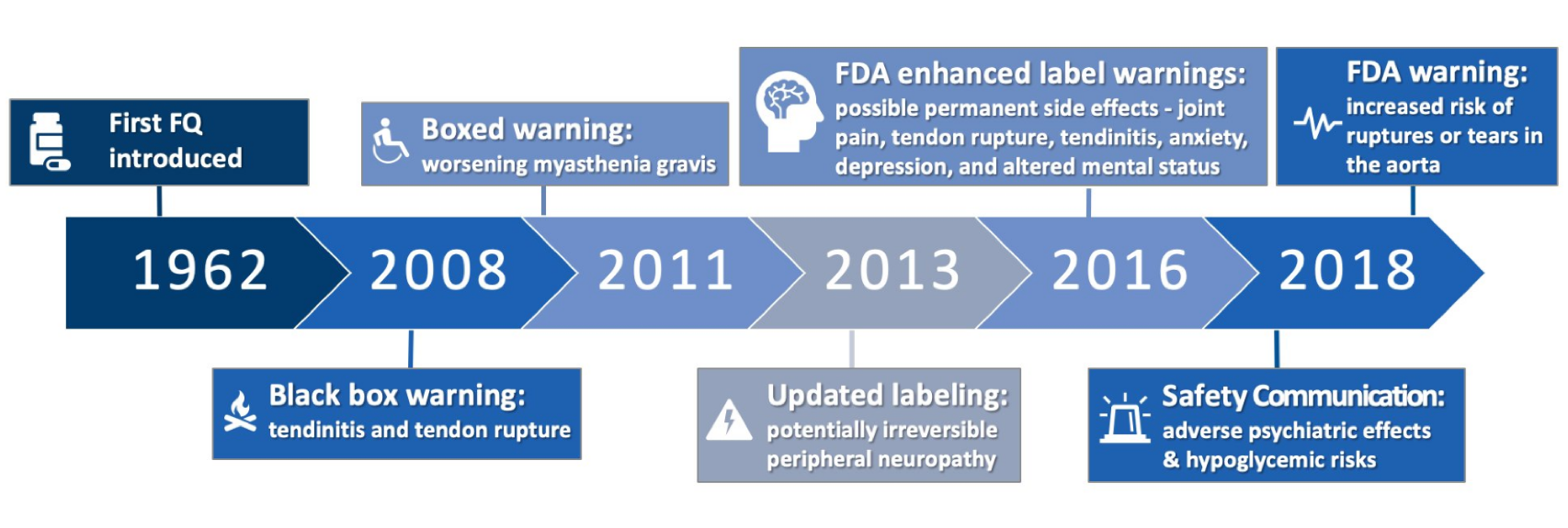
- Per FDA, fluoroquinolone use is linked to aortic dissections. As the parade of adverse events for this drug class marches on, it’s worth remembering that they remain extremely useful antimicrobials, especially in patients with complex infections. For those interested in the history of these alerts, here’s a great graphic, courtesy Travis Jones, PharmD:
- Dolutegravir monotherapy lands with a thud. In the linked study, nearly 10% failed by week 48 (some of whom developed resistance), prompting cessation of the study. A second study done in patients treated during early infection suggests the monotherapy strategy may work in patients with a low viral reservoir, but 1) we don’t measure reservoir in clinical practice, and 2) what’s the point?
- Starting antiretroviral therapy right away works great — even in the most difficult-to-treat populations. In a group of 216 patients with high rates of mental illness, substance use disorder, and homelessness, an astounding 95.8% achieved an HIV viral load <200 at least once after receiving immediate ART. I can’t imagine this occurring without integrase inhibitor-based therapy.
- A 39-year-old man nearly died of influenza last year, and now he’s publicizing the importance of the flu vaccine. I have tremendous admiration for people who endure such extreme hardship and then try to make something good out of the experience.
- A vaccine is under investigation for recurrent vulvovaginal candidiasis. This phase 2 study demonstrated safety and immunogenicity and hinted that it would be effective as well. For the record, there are currently zero vaccines for fungal infections.
- Here is a superb summary of the severe infrastructure problems fueling the national hepatitis A outbreaks. This disease is strongly linked to breakdowns in sanitation and hygiene, and not surprisingly have targeted the homeless and drug user populations.
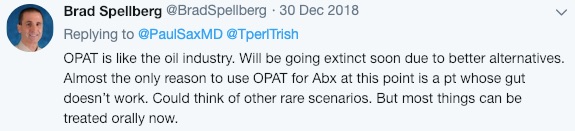
- Complications are very high with outpatient parenteral antimicrobial therapy (OPAT) for severe Staph aureus infections. Roughly 33% experienced an adverse event, and 64% were readmitted at 90 days. Clearly a very tenuous patient population! And will Dr. Spellberg be right in his bold prediction?
- In North Carolina, infective endocarditis related to drug use has increased more than 12-fold over the past 10 years. As I’ve noted numerous times before, this dramatic rise in drug-use-related endovascular infections is one of the most profound changes in ID since starting practice in the early 1990s.
- Add wound botulism to the list of infectious complications of injection drug use. These cases in California involved black tar heroin, which is made mostly in Mexico. During transport inside car tires and other unsanitary locations, it may be exposed to soil containing Clostridium botulinum spores.
- Using both pneumocystis PCR and blood beta glucan improved the diagnosis of Pneumocystis pneumonia in cancer patients. These two tests complement each other — PCR is highly specific, but it may be too sensitive; a high value on beta glucan can help distinguish between colonization and true infection.
- Beta glucan is frequently elevated after abdominal surgery. Another study underscoring the basic problem with this test — if it’s ordered in the wrong context, there are innumerable false positives.
- Fusobacterium necrophorum is often implicated in recurrent peritonsillar abscess. This anaerobic gram-negative infection is more famously known for causing septic jugular vein thrombosis (Lemierre’s syndrome), but it clearly has a role in other suppurative complications. Question: Would a throat swab diagnostic test for F. necrophorum help identify the non-strep pharyngitis cases that would benefit from antibiotics?
- Cefiderocol versus imipenem for (what else?) complicated UTI — and cefiderocol comes out the winner. The winner, that is, based on microbiologic response. As a reminder, cefiderocol is a “siderophore” antibiotic (you can read here what this means), with activity against multi-drug resistant Pseudomonas, Stenotrophomonas, and Acinetobacter spp. Looking forward to seeing the studies in more difficult to treat patient populations, such as hospital-acquired pneumonia.
- Here’s a simple framework to guide antibiotic prescribing: 1) Is infection one that needs an antibiotic? 2) Have cultures or other studies been sent? 3) What empiric treatment should be started? 4) How should results alter therapy? 5) What duration is required? ID clinicians have internalized these thoughts, but no harm making them explicit.
- A woman acquired HIV that was highly resistant to all available integrase inhibitors. Transmission of integrase inhibitor resistant virus is very rare; these viruses have typically still retained susceptibility to dolutegravir and bictegravir. Not this one — the baseline isolate had three major integrase mutations, E138A, G140S, and Q148H. The critical information from the case report was the identification of the source patient, for whom the authors obtained detailed resistance information.
- For ID specialists, management of Staph aureus bacteremia is all over the map. Treatment of choice, management of persistent bacteremia, duration of therapy — plenty of variation! Example: For MSSA endocarditis, 32% chose cefazolin, 29% favored nafcillin, while 32% considered the two the same. Practice variation can represent differences in quality, but here I think they reflect lack of a clear, evidenced-based choice.
- For infected burn wounds, bacteriophages did worse than standard of care in reducing Pseudomonas aeruginosa bacterial burden. This approach to treating resistant infections is highly promising, but still in its infancy.
- Three patients suffered wound infections from Lonepinella koalarum after koala bear bites. No, I’ve never heard of that bug either — which, given the source, will never become a global threat — but the molecular investigation into these cases is quite the tour de force.
Have you written 2018 on a form or check yet?
Of course you have. Happy New Year!
And just 18 million views for this video (and counting):


Very nice updated reviews
Before your prescribe antibiotics think ABCD
Antibiotic- choice for what
Bugs you want covered
Creatinine Clearance & appropriate dose
Duration
Thank you for the review. I always look forward to Link-o-Rama!
The death of the woman from Virginia from rabies was very tragic. Just to point out that the rabies vaccine is widely available in the private healthcare system in India, and is also available free of charge in government hospitals in many states ( the government hospital where I rotated as a medical student prescribed it routinely in the emergency department). Medical education in India addresses rabies prevention and providers prescribe the vaccine routinely. I hope ID docs in travel clinics in the US will use this unfortunate case to inform their patients on the need to seek immediate medical care following a dog bite and the widespread availability of the vaccine in India.