An ongoing dialogue on HIV/AIDS, infectious diseases,
February 4th, 2022
Prior COVID-19 Is No Guarantee of Immunity
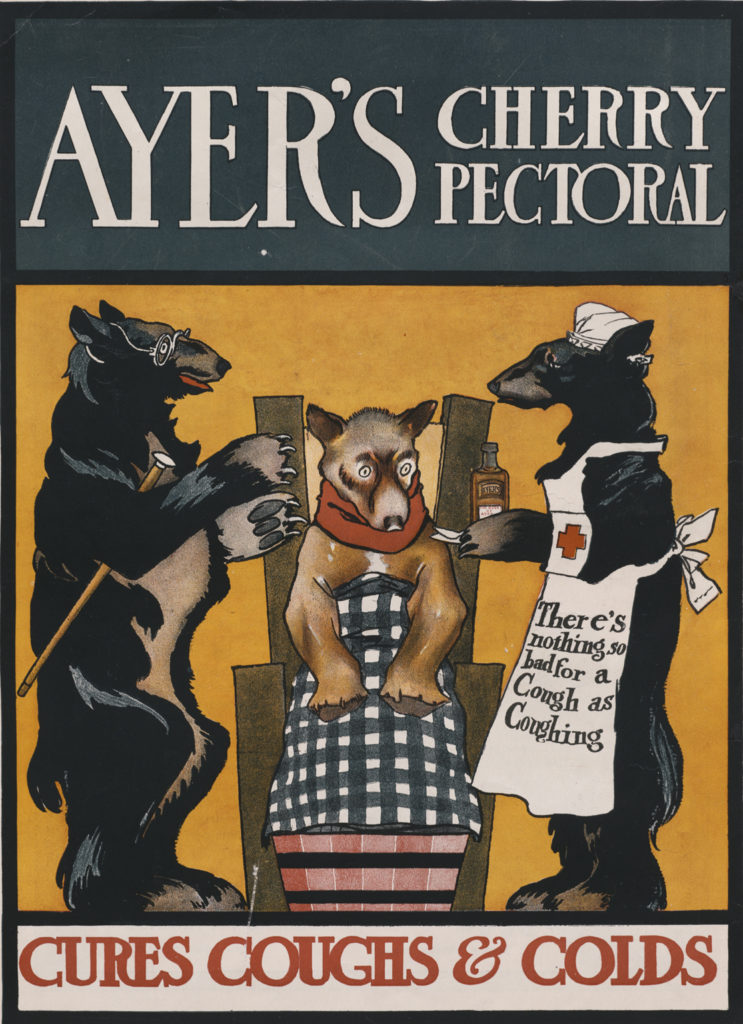
19th century apothecary advertisement, Lowell MA. Product has fewer drug interactions than ritonavir-boosted nirmatrelvir.
I’m no immunologist — a fact made vividly obvious to me several years ago when asked to teach a weekly medical student section that included cases and problem sets. The challenge was that the course combined immunology and microbiology.
I was on much firmer ground with the microbiology than the immunology, the latter often a wonderfully complex and mysterious system.
So why, then, am I about to wade into perilous waters and write about something very much immunology-related, a subject I’ve already confessed to being an amateur at? Because to us ID specialists, the immune system plays a critical role in how our bodies respond, clear, and protect us from various infections. We may not be true experts, but it’s highly relevant to what we do.
Additionally, I’m watching a debate unfold among ID colleagues, public health officials, epidemiologists, the lay public, politicians, and yes, even advanced degree-holding immunologists. It’s a debate about a critical issue facing the globe as we march on to the third year of the pandemic.
Namely, does infection with SARS-CoV-2 confer protective immunity?
Views range from “yes, certainly” to “maybe, sometimes” to “it depends” to “absolutely not.”
Everyone can cite their favorite study to back up their opinions — whether it’s an epidemiologic analysis of reinfection rates, or the cases of reinfection after prior COVID-19 that are less (or more!) severe than the first, or an in vitro study demonstrating robust (but then waning!) antibody responses, or how cells from people with prior infection continue to mobilize protective cytokines, or contrarily how prior infection inhibits these helpful cellular responses.
Many of the people lining up on opposite sides of this debate are smart, have impressive credentials, and aren’t shy about expressing their opinions — hence sparks do fly.
This doesn’t help resolve the issue, because of course they cite mostly the scientific studies and opinion pieces that support their views.
So for the price of subscribing to this blog, here’s my non-immunologist’s take, and warning — it’s a messy one with no precise answer:
Prior infection confers some degree of protective immunity. It varies from person to person, depends on the severity of the disease, with “just right” being more protective than mild or severe illness. (Cue classic Goldilocks analogy.) It’s not durable, is not guaranteed, and certainly isn’t going to lead to herd immunity on its own anytime soon.
Nope, no herd immunity by April 2022, just like it didn’t happen by April 2021.
Incomplete immunity conferred by prior episodes of COVID-19 is one critical reason that studies of populations continue to show that the unvaccinated have a markedly higher rate of hospitalization and death than the vaccinated — even though prior infection is becoming more common.
Two years into the pandemic, with major population surges, this remains an undeniable fact everywhere it’s studied — even though a higher and higher proportion of the unvaccinated have already had the disease. If prior infection were strongly protective, the gap between vaccinated and unvaccinated in risk of hospitalization would decrease over time. It hasn’t.
Omicron only exacerbated this reinfection issue, with many of us seeing or hearing about patients with repeat infections, sometimes quite quickly after a first infection:
https://twitter.com/TheBlondeRN/status/1489608641858654219?s=20&t=bairQyDjErYe4NJziFpC9Q
Indeed, if we asked a group of primary care clinicians, emergency room folks, and other front-line providers to raise their hands if they had cared for or heard of people with more than one episode of COVID-19 — usually less severe, but sometimes more — 100% would have their hands up.
Incomplete protection from prior infection isn’t what any of us want to hear. But as we’ve learned again and again, wanting something from this virus doesn’t make it happen. The other night, someone in my family asked me whether now, as Omicron nabbed so many of us who previously escaped, can we at last move past this pandemic and get back to normal?
It’s such a good question!
I just wish I had a more reassuring answer.
In the meantime, let’s get everyone vaccinated, even those with prior infection. It’s a much more reliable way of getting protected, especially from severe disease.


Expectations from vaccines were based on incomplete understanding of vaccines, and accounts of polio, smallpox, but we routinely discounted annual flu vaccines.
I am not taking sides either but find it very fascinating and curious that we have incomplete protection after natural infection or with a vaccine. When you combine infection and vaccine, we may have better protection. I am interested in a final explanation one day as to why. We have presumed over the years that natural infection to a disease often means immune protection
Paul, Thanks again for addressing issues that we face every day in the office. Please keep up the good work, it helps us all.
Does reinfection occur because of the poor immunogenic nature of the coronavirus, a waning immunity over time or immune escape by novel variants? I’m betting on the last option. The concept that this virus has evolved to represent a much different pathogen than the Wuhan strain may be grossly underestimated. If so, the dilemma of reinfection is far from surprising.
Yet, the threat of reinfection fails to capture the more critical issue of relative morbidity with reinfection. It may be wishful thinking, but I suspect the risk of severe illness with reinfection will prove to be much lower.
Paul
Good points and completely consistent with what I’ve been saying. We will continue to have difficulty educating the public when most of their information, even if factual, is based on soundbites. This, I think, is part of what makes the debate so raucous.
Whether vaccinated with single, double or triple dose, I have seen enough people to get infections and reinfections to make me wonder are we doing right by vaccinating? Whether vaccinated or earlier infected, reinfection is common.
Most of these are now getting milder form of disease (proved by RTPRCR).
I wonder whether the change in clinical profile has anything to do with our immune system at all? Is it not happening because the virus is now getting better adapted to human body and following the principle of “Live and Let Live” as propounded by “The Selfish Gene” theory of Richard Dawkins?
There indeed are few guarantees in medicine -but prior infection does seem to be just as effective as immunization in preventing hospitalizations, which is probably our most important goal – this is data from 1/28/2022 MMWR:
https://www.cdc.gov/mmwr/volumes/71/wr/mm7104e1.htm#T1_down.
take a look at the figure – the previously infected cohort is the same or lower than vaccinated and vaccinated/prior infection
I don’t think this is a settled point and there are a number of problems with this data.
In the MMWR study above, the lowest risk of hospitalization was in people who were vaccinated AND had a prior COVID infection (ie hybrid immunity). The MMWR study also takes data from the Alpha and Delta variant time frame, so results are likely not applicable to the Omicron variant. More importantly, this study didn’t account for the booster doses. This is extremely important when comparing the groups because we now know that vaccine immunity tends to wane over time. Last point about the MMWR data: studies of reinfected groups of people have to be interpreted with caution because they are subject to survivorship bias (always an issue with “natural immunity” or reinfection studies).
Here’s an example where immunity from prior infection was NOT equal to or greater than vaccine-induced immunity. In this study of hospitalized patients, unvaccinated people who had previous COVID infections were 5x more likely to have a positive COVID test (indicating reinfection) compared to vaccinated people: https://www.cdc.gov/mmwr/volumes/70/wr/mm7044e1.htm
Todd Bagwell’s citation of the MMWR report showing equal protection against hospitalization in the unvaccinated with reinfection vs. those vaccinated with breakthrough is a key point. I’m fascinated that we would believe/expect that 3 brief exposures to spike protein generated through vaccination would produce as or more robust immune protection than the prolonged, continuous exposure of days of viral infection, with not just the spike protein to elicit an immune response, but the rest of the virus as well.
As others have pointed out, the antigenic drift in SARS-CoV-2 may stymie either approach, and perhaps – just perhaps – the combination of prior illness and vaccination will prove superior with future variants for preventing hospitalization and death. At present, I don’t think we have the data to prove that, and the fact that both sides of the ongoing debate are so fervent (sometimes to the point of dogmatism) suggests to me that the truth may lie in the middle. Humility, so well demonstrated by Paul Sax, is a character trait sadly lacking in our ongoing debates.
The consequences of endemic Covid regardless of patient history vis-a-vis infection or vaccination needs to be explained to the public. Some of we senior citizens with auto-immune bleeding issues who cannot risk IM injections without large doses of IVIG, already know the score or have died. The same situation exists for the severely immune-compromised, except they can tolerate IM anti-virals. Someone in the Healthcare field needs to prick the balloon of the invincibility of medicine and prepare us for the future that has dropped on our collective doorstep.
John the elder
Thank you.
So Vaccination vs Infection immunity … seems newly borns have better imunnity form vaccinated mothers than from infected mothers …
Shook LL et al. Durability of anti-spike antibodies in infants after maternal COVID-19 vaccination or natural infection. JAMA 2022 Feb 7; (https://doi.org/10.1001/jama.2022.1206)