An ongoing dialogue on HIV/AIDS, infectious diseases,
May 8th, 2016
Zika, Baseball, and Waiting for a “New Normal”
 I received an email from someone who’s known me a very long time.
I received an email from someone who’s known me a very long time.
Hint: She’s known me longer than anyone. Literally.
Here’s the email:
Baseball cancelled in Puerto Rico because of Zika. This story has you written all over it. (To use a cliche.)
Mom
I told you she knew me well!
For those not obsessed with this silly game to the same degree as I, here’s the story: Two games between the Pittsburgh Pirates and Miami Marlins were scheduled in San Juan, Puerto Rico on May 30-31 instead of in Miami.
This two-game series, of course, was planned before anyone had any idea that Zika would arrive and become a major health threat in Brazil, then move rapidly through Latin America and the Caribbean — including to Puerto Rico. Several hundred cases of Zika have been reported Puerto Rico (including one death), and some have estimated that 25% of the population will eventually become infected.
The players on the Pirates and Marlins raised significant concerns about traveling there, and two days ago it was announced that the series would be cancelled as a result.
Puerto Rico officials were, predictably, highly critical of the decision.
So what was Major League Baseball supposed to do? I can see both sides of this issue.
In favor of cancellation:
- A player could contract the virus and transmit it to his partner. This is of greatest concern, of course, if the woman is pregnant or trying to conceive.
- There’s still no readily available test to see if infection has occurred. A large proportion of infections are asymptomatic. Are these players supposed to wait 6 months before trying to have children? Or have unprotected sex? Seems like a lot to ask.
- There’s a small (but not zero) chance that a player will get either severe clinical Zika (fever, myalgias, and rash) or, even worse, Guillan-Barre syndrome. Bad enough for anyone — baseball player or not — but imagine if this player were a star like Andrew McCutchen or Giancarlo Stanton. (Brief aside: Stanton hit a home run nearly 500 feet the other day. Wow. Watch here.)
- What do the players get out of it? The whole idea of these trips is to promote the game globally — so it’s good for “the game”. But how about the players? They get paid the same regardless of where the games are played — why should they take this risk?
In favor of playing the games in Puerto Rico as originally scheduled:
- The CDC travel advisory on Zika is limited to women who are pregnant or trying to get pregnant. Not a single professional baseball player falls into this category. Didn’t even have to look that one up.
- The players will be mostly in settings where Zika transmission is highly unlikely. I don’t have their exact itinerary (they don’t typically share this with ID doctors), but it’s safe to assume they would stay at 5-star air conditioned hotels when they’re not playing. A comfortable air conditioned bus (at worst) would take them to and from the game. And though the stadium is old, it’s got to have an air conditioned locker room. Sure, the game itself is outdoors — but only for a few hours.
- They will only be there for three days. For such a short trip, the risk of getting Zika with the above conditions is incredibly small. Maybe almost as small as my chances of hitting a home run nearly 500 feet.
- How different is San Juan from Miami anyway? Virtually all public health officials are predicting Zika transmission in Southern Florida any day now. It might even be happening now — who knows about late May?
- Puerto Rico is the birthplace of several baseball superstars. Plenty of Hall of Famers and near Hall of Famers: Roberto Clemente. Roberto Alomar. (Hey — second time I’m writing about him!) Edgar Martinez. Ivan Rodriguez. Bernie Williams. This is an important pipeline for top baseball talent, we should support it.
- Zika didn’t stop hundreds of baseball scouts and other officials from recently visiting Puerto Rico to see a top prospect. The guy’s name, for the record, is Delvin Perez, a high school shortstop. I’d bet good money he never expected to see his name on this blog.
- They aren’t cancelling the Olympics in Brazil. If thousands of athletes from around the world can go to Rio, why can’t a couple of baseball teams go to Puerto Rico?
- Given what they’re being paid, the players should just do what they are told. The current average MLB salary is over 4 million dollars per year. The aforementioned Stanton has a 13-year, $325 million dollar contract. That will buy you plenty of DEET.
I don’t know whether baseball made the right decision on this one. But I do know that Zika is still so new, and so much is still unknown, that the decision is certainly understandable. With new threats of any sort — infectious or not — our risk assessment instincts are flawed, and typically biased toward fearing the worst.
So let’s give it a few years — Zika isn’t going anywhere, unfortunately. At that point we’ll know a lot more about how it causes disease, and in whom, and maybe even how to prevent it. We’ll certainly have better testing. There will be a “new normal” attitude about a world with Zika, just as there is now with West Nile virus, another mosquito borne virus which didn’t even exist in the Western hemisphere before 1999.
Once that new normal happens, I boldly predict that there will be professional baseball games played in San Juan.
Happy Mother’s Day!
April 30th, 2016
A Ridiculously Long Post: How EHRs Expose Unspoken Hierarchies Within Medicine — Or Maybe Are Just Bad
 I am consulted by a surgeon about a patient with something that might be infectious, might not. A very appropriate referral.
I am consulted by a surgeon about a patient with something that might be infectious, might not. A very appropriate referral.
After seeing the patient and reviewing the history and scans, I decide a CT-guided biopsy is the next step.
The nice radiology fellow tells me “Just place the order in [enter name of EHR here]”. Since this is the first time I’m ordering this test using our new system, the prospect of doing so doesn’t exactly fill me with joy.
Nonetheless, I give it a go. I place the word “biopsy” in the dreaded order search box, hit enter, and cover my eyes, at least metaphorically.
A lengthy list appears, and I select the test closest to the one desired — for some reason it’s called “CT IR MASS ASPIRATION/BIOPSY (NO CATHETER) (Order #152640784)”. The order then requires filling out numerous fields (some of them woefully tiny for anyone past the age of, ahem, failing eye accommodation), clicking several check boxes, and deciphering inscrutable warning messages.
Since the precise diagnosis on this case isn’t yet known, and a precise description of the problem doesn’t come up in the formatted search, I do what everyone does when trying to navigate these complex screens and their finicky criteria.
I fudge it (in other words, make something up). Nevermind that the fudge doesn’t really fit the case — voila, it goes through!
But most importantly, the order for the biopsy includes a free-text box, where I enter the critical micro tests desired, specifically:
- routine and anaerobic culture with gram stain
- fungal culture and smear
- AFB culture and smear
- Nocardia culture and modified acid-fast smear
Note to micro lab: Prioritize pathology and fungal culture/smear if there isn’t enough specimen.
(If that seems overly detailed, trust me — I’ve been doing this ID stuff a long time. You’ve got to give precise directions. Sometimes you might even need to go from being the ID Attending to, as my brilliantly funny colleague Libby Hohmann once put it, the “Transport Attending”. That happens when you both specify the cultures to be done and are the person making sure the specimens arrive at the lab appropriately.)
After completing the order without setting the computer aflame, I feel a little glow of satisfaction — kind of like when you get a tough clue in a crossword puzzle, correctly guess your opponent’s hand in poker, or predict in advance when the runner on first tries to steal second on a 2-1 count.
Or maybe that glow is simply the computer screen reflecting off my face? Because the satisfaction is short-lived — soon after placing the order, I receive this from the radiology fellow:
Dr. Sax, thanks for your biopsy request. In addition to the order, we require you to put in separate orders for each microbiology test before the biopsy. Could you please place these individual orders- i.e. fluid culture, AFB, fungal culture, nocardia, etc and any other micro testing you think would be relevant? These will need to be entered as “Signed and Held” orders.
Brilliant.
Thoughts, emotions, reflections on this unfortunate turn of affairs.
- Why does this make me feel so worried — and frustrated? I envision entering these individual orders as a sure-fire way of heading down a bunch of digital rabbit holes, especially since some of the orders aren’t exactly common. What are the chances that the stain for nocardia would be straightforward? The frustration is amplified of course, by the fact that I already have written exactly what is wanted in the free text box. (That will be the first — but not last — time I mention this.)
- Why do I have to write these extra orders? No doubt for some billing and/or compliance reason, something completely separate from the patient care activity. Even though the desired tests are already clearly entered in the computer (second time mentioned), if they aren’t entered in exactly the right way, in exactly the right place — and by correctly, I mean “according to the rules of this particular EHR to meet whatever criteria are set up by whatever payer” — then they can’t be done because they won’t be paid for. Joy. Note that in our last EHR (we’re on our fourth), this free text order would have been fine.
- Why doesn’t someone more expert with the EHR take what I’ve written and enter the orders? Yes, this is passing the buck, but what we want is clearly spelled out in the free text box. (Third time.) It’s highly likely that someone on this care team has the expertise with this EHR to transcribe what I wrote into compliant EHR-ese. Maybe a “Super User”? Maybe a person whose sole job is to make sure orders are compliant with the above regulations? I hereby authorize him/her to make this happen.
- Why does this feel so burdensome compared to writing orders the old way? We doctors don’t mind writing orders when the process is straightforward — hey, look at my “free text” order for the micro tests cited above. (Fourth time.) Piece of cake. I have written orders like this hundreds of times, or alternatively written this exact list in hundreds of consult notes that are then transcribed into orders by others (interns, residents, PAs, NPs). But the process of writing orders has changed — it’s become tremendously nonintuitive — and even worse, it differs dramatically between platforms. You know how good electronic calendars can take your free text that says, “Dinner next Tuesday 7pm with Consuela at El Conejo Guapo restaurant”, and bingo, the dream date at The Handsome Rabbit is entered correctly? Wouldn’t that be a nice EHR feature? Dream on.
Perhaps the most important question hasn’t even been mentioned yet, and it’s this:
Why does it bother me so much?
I know, I know. In the time I spent writing this absurdly long anecdote, I could just suck it up, enter the orders, and get on with life — a bit frustrated, yes, but ready to move on to the next challenges, such as learning how to spell (and pronounce) “Aedes albopictus” and what PCSK9 actually stands for.
But first, some additional musing on this last question — why it’s so annoying — have yielded 3 key answers:
- Concern that the right tests won’t be done despite all the effort. This is the most important issue, after all — we’re all trying to help our patients. Wouldn’t it be terrible if the critical microbiology tests were omitted based on a cumbersome physician order entry system? Even after I clearly wrote the tests in the initial order? (Fifth time.) Or taken to the extreme level (why not, I’ve written this much ) — what if some critical intervention isn’t done because the order isn’t written correctly in the computer. Imagine those CPR scenes from the TV show ER if, instead of verbal orders, George Clooney had to fire up his laptop, put on his reading glasses, and start typing.
- A fear of the endless time sink. What if some of the tests don’t show up in the initial search? What if there’s an option for separate “nocardia culture”, “nocardia stain,” and “nocardia culture and stain” — do I choose the first, second, or third one, or all three? What if they ask if it’s “lab collect” or “clinic collect”, since it’s neither? How does a “Sign and Hold” order (as specified by the radiology fellow — who emphatically is blameless in this) differ from a regular signed order? I see the edge of that rabbit hole, drawing closer …
- The process elicited an uncomfortable reinforcement of the weird hierarchies in medicine. Any chance that this patient’s surgeon is dealing with the same challenges? I asked him, and he knows the EHR can be difficult, but he told me he barely ever interacts with it — he’s got a veritable army of scribes, PAs, residents, and other support staff who enter the information for him, support staff he can justify financially based on how hospitals are paid these days. Hearing he’s exempt from these frustrations elicited the same feeling I get watching the First Class flyers board the flight early. For the vast array of doctors (and essentially 100% of nurses and PAs, let the record show), no such luck. A giant chunk of EHR-generated clerical work has been handed to us in the form of mouse clicks, drop-down menus, and (too small) text fields. And it just feels lousy.
You might be wondering, after this long screed, what I ended up doing with these orders. Someone has to enter them eventually, right?
Guess.
https://youtu.be/rK1iPNeLTAo
(Picture credit: Anne Sax)
April 24th, 2016
Why Getting Old Isn’t Always So Terrible — and Why People with HIV Can Now Get Life Insurance
 Two patient-related anecdotes, then a news item.
Two patient-related anecdotes, then a news item.
Anecdote #1:
A little email exchange I had with one of my patients recently:
Hi Paul,
Wondering if you got the refill request for my meds from my mail-order pharmacy — their customer service is lousy, and I can’t tell if it’s been approved. I’d like to get this settled before the weekend as I’m going away for a few weeks to celebrate my birthday.
Roger
My response:
Hi Roger,
Yes, I got the message and efaxed them the approval. They should have it to you by the end of the week. And happy birthday!
Paul
So why is this notable? He got his HIV diagnosis in 1989, and was told by more than one person (some of them famous doctors) that he’d be dead in a few years.
After some clinical trials with AZT and other early treatments that didn’t work out so well, for the last 15 years or so he has been totally stable from the HIV perspective, virologically suppressed, with a normal CD4 cell count, and no significant side effects from his treatment.
For the record, it’s his 80th birthday he’s celebrating. Guess those early predictions about his survival were wrong.
And that some older people really can do email.
Anecdote #2:
It’s 1992, my first year as an ID attending — early on in my first “real” job.
(I put it in quotes because what are internship, residency, and fellowship if not “real” jobs? Never really understood that distinction. But you get the point.)
A primary care doctor asks me about one of her patients, an HIV positive woman in her late 30s. The patient has a low CD4 cell count, but is asymptomatic. Since there is no email then, the doctor and I have an actual conversation.
It goes something like this:
PCP: Hi Paul, do you remember Tara, whom you saw once and started on AZT and Bactrim?
Me: Sure, how’s she doing?
PCP: She’s doing OK — CD4 cell count is down to 120, but she’s feeling fine. I’m wondering what to do about her cholesterol, which is over 300! Plus her mother died of a heart attack, and she’s really worried about it. Should I start her on lovastatin?
Me (skeptically): You could … but given the prognosis of someone with a CD4 of 100, and that she’s only in her 30s… is it really going to help her? How about we switch her to ddI? I can see her to discuss this.
PCP: Sounds good. But I’ll start her on lovastatin [You kids might not remember, that was the first statin drug.] It will make both of us feel better.
Me (thinking this but not saying it): There is no way she will live long enough to benefit from cholesterol-lowering therapy.
Fast-forward to today. Tara indeed continues to feel “fine”, at least from the HIV perspective — zero HIV complications, ever. Cardiovascular disease is by far her biggest threat, as she clearly has familial hypercholesterolemia.
Not the first time I’ve been wrong. And certainly not the last, as I thought the touch screen keyboard on the iPhone was a stupid idea that would never catch on.
Now the news item, from this week’s Boston Globe:
Good news — but importantly, the company is not selling life insurance policies to people with HIV for altruistic reasons. It’s no more an act of charity than when viatical companies purchased life insurance policies from people with AIDS in the bad old days (see the ad above from a 1994 magazine).
As illustrated by the above anecdotes — and no doubt thousands of others in practices around the world — survival for patients with HIV who are on treatment is every bit as good as for people with other chronic illnesses, in many cases better.
Here’s why Hancock is making this policy change, and why other insurance companies will likely soon follow:
“It’s based almost entirely on data, such as survival rates for people who have been on certain types of medication,” said Steven Weisbart, senior vice president and chief economist for the Insurance Information Institute, a New York-based trade group … “This is a very competitive business,” he said, “and companies like the Hancock and the Pru are looking for new policyholders who will buy life insurance that’s hopefully been priced appropriately.”
“What a drag it is getting old,” said the Rolling Stones, famously, in this song.
But as our long term survivors will tell us, it sure beats the alternative.
Happy Passover!
[youtube https://www.youtube.com/watch?v=baQfqoZrEvI]
April 15th, 2016
Mystifying Abbreviations on Daily Medical Rounds
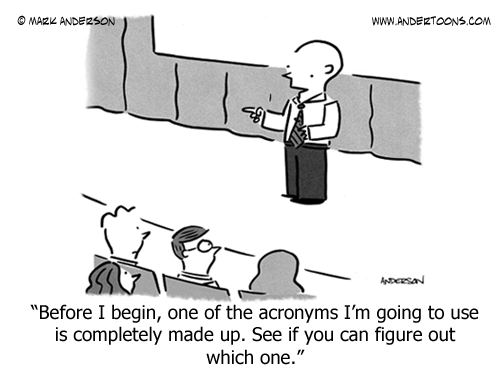 I am currently attending on the inpatient medical service — always a treat, and a great learning experience for me each year. Aside from the refresher on inpatient general medicine — hey, no amount of repetition is too much when it comes to working up hyponatremia — I’m also fascinated by the steady proliferation of abbreviations and acronyms, bits of absurd sounding non-words or letters that sprout like weeds in the conversations and notes of these fine young doctors.
I am currently attending on the inpatient medical service — always a treat, and a great learning experience for me each year. Aside from the refresher on inpatient general medicine — hey, no amount of repetition is too much when it comes to working up hyponatremia — I’m also fascinated by the steady proliferation of abbreviations and acronyms, bits of absurd sounding non-words or letters that sprout like weeds in the conversations and notes of these fine young doctors.
Below a select list of some of the commonly used terms bandied about by our skillful interns and residents. Some are nationally used, others are just local-isms that are highly relevant for our hospital’s patient population.
- MOLST
- BMP — not to be confused with BNP, which also wasn’t in circulation when I was a resident (because it wasn’t available), but is now pretty established
- CIWA
- G and G — originally I thought it was GNG, but it’s not.
- CTPE
- TTP — not the hematologic disorder
- WOB
- DOAC
- HDS
- PNA
- TROPE
- RUCKUS — at least that’s how it’s spoken, as in making a lot of noise (a ruckus), but (hint) not spelled that way.
- APLAS
Note that none of these abbreviations or acronyms was in circulation when I was a house officer, but of course that was some time ago (ahem), so that’s not surprising. What’s remarkable is that many of them weren’t even used much last year, showing the remarkable fluidity of medical language, and ensuring an unending supply of confused medical students and gray-haired doctors.
So how many of them do you know? Please offer some guesses in the comments section. Upfront warning — the degree of difficulty is highly variable, and using the google machine (or even UpToDate) may not help.
April 2nd, 2016
You Too Can Have Fun with Academic Spam
Like most doctors who work at academic medical centers, I get a fair amount of “academic spam” — invitations to bogus meetings that take place in some exotic or at least warm place (China, Dubai, and Orlando are favorites), efforts to sell me monoclonal antibodies or, more recently, CRISPR-altered mice, and of course requests to contribute research papers or review articles to made-up journals.
These efforts must make money because, well, otherwise they wouldn’t exist.
So here’s a wonderful opportunity that recently came my way (some details changed to protect the “innocent”, but assuredly I haven’t changed the writing style or font colors one bit):
Editorial Board Membership: Wilkie Renal DisordersDear Dr. Paul E,Greetings of the day!It is an excited endeavor to start a new open access journal in the field of Medicine. At the onset, we would like to invite you to join us as an Honourable Editorial Board Member of Wilkie Renal Disorders.Wilkie Renal Disorders is an open access, peer reviewed, scholarly journal dedicated to publishing articles in all areas. The aim of the journal is to provide a forum for Nephrologists, researchers, physicians, and other health professionals to find most recent advances in the areas of clinical and experimental renal disorders.Please visit our journal at: http://wilkiepublishinggroup.com/wilkie-renal-disorders/If you are interested, kindly provide your short CV full contact details along with expertise keywords of your ongoing research work.We await your reply with interest.Best regards,Samantha FarnsworthEditorial office- Wilkie Renal Disorders# 54 Turniptown Way,
NEW JERSEY 08831, USA
Tel: +1-201-698-7575
You can imagine how excited I was to receive this invitation. Quickly, I replied as follows:
Dear Samantha:
Greetings of the day back to you! I’d be honoured to accept your invitation to be on the Honourable Editorial Board of “Wilkie Renal Disorders”. Here are my demands, which an impressive journal like yours no doubt will find easy to fulfill:
 That you provide me board certification in nephrology, as I am currently trained only in bloodletting and bicycle repair.
That you provide me board certification in nephrology, as I am currently trained only in bloodletting and bicycle repair.- That you continue to refer to me as “Dr. Paul E.” The “Sax” part was always tricky for people to spell, and took too long to write.
- That during Editorial Board meetings, you allow me to bring my companion pet lizard, a green iguana whose name is Oscar. He’d appreciate a name tag during the meetings so that he feels like part of the team! Attached please find a photo so you’ll recognize him when he comes.
I look forward to a long and productive working relationship!
Regards,
Paul E.
Haven’t heard back yet. Maybe they have a “no iguanas” policy for their renal journal.
But the good news is that the next day the same publishing company invited me to be on the board of their Orthopedics journal, which I hear is much more liberal with companion pets.
March 27th, 2016
One-Week-to-Baseball ID Link-o-Rama
(Important note: Title has nothing to do with this post’s content. I just felt like writing something about baseball.)
As some of us eagerly await the start of the 2016 baseball season — especially Cubs fans — here are some ID/HIV items yearning to shag flies, toss around the horsehide, and play some pepper:
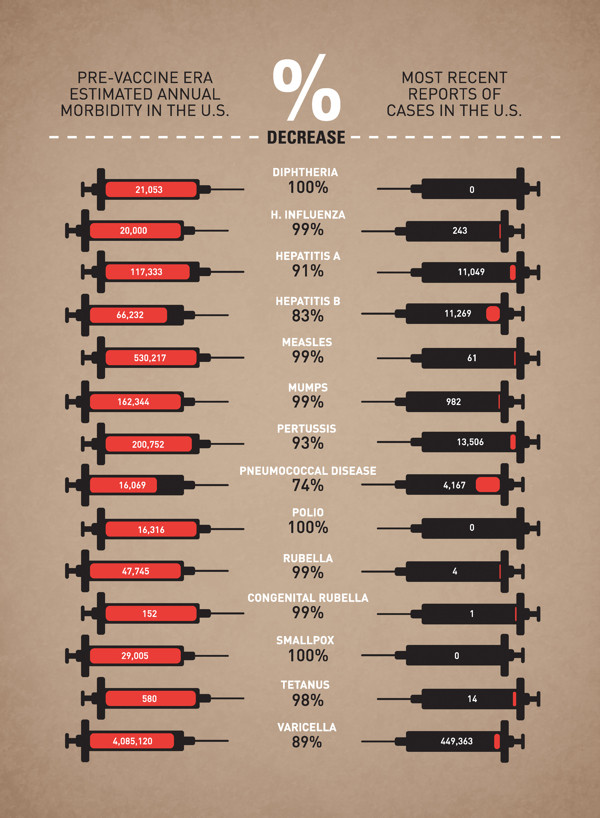
- Famous anti-vaxxer — and notorious scientific fraud — Andrew Wakefield was going to have his film shown at the Tribeca Film Festival, but now it’s been pulled. Robert De Niro might be a great actor, but he whiffed big time on this one. Here’s a humorous editing of the festival’s original biography of the filmmaker (notice I don’t write “scientist” or “doctor”).
- TB cases in the USA are up for the first time in 23 years. Up a little — 157 more cases in 2015 than 2014. It’s the end of a longstanding decline, a remarkable success story (so far). The CDC report accurately describes this as a “leveling” of TB rates — it’s not a “surge” as the headlines in the popular press write — but it also makes the complete elimination of TB in this country increasingly unlikely.
- CRISPR/Cas9 eliminates HIV from T-cells. With the caveat and confession that I’ve never done a single second of basic science research, my gut feeling is that this (or a related strategy) is more likely to be successful at curing HIV than giving chemotherapy-like drugs to “awaken” the latent reservoir. But what do I know? Good review of CRISPR for non-lab scientists here.
- While we’re curing HIV, let’s also try a new HIV vaccine strategy. This one will generate broadly neutralizing antibodies (bNAbs), which are all the rage.
- Lots of flu out there right now. You’d almost think influenza is seasonal, or something crazy like that.
- The outbreak of Elizabethkingia anophelis in Wisconsin continues to baffle public health officials. The bugs are genetically related, but there’s no obvious environmental source (yet), and cases are widely dispersed geographically. Contaminated injectable medications, or an intravascular medical device, both distributed from the same (unsterile) point of origin? Trivia question — what was Elizabethkingia called before it was named after microbiologist Elizabeth O. King?
- CDC has issued an updated guidance on caring for women and men of childbearing age with Zika exposure or disease. Key take home recommendations: After symptomatic disease, women should wait at least 8 weeks before attempting conception, and men at least 6 months. With possible exposure and no symptoms, both should wait at least 8 weeks. As the data linking Zika to birth defects continues to accumulate, these guidelines make a lot of sense.
- In other mosquito-related infection news, this dengue vaccine candidate (TV003) looks very promising. All 21 vaccine recipients were protected against infection after challenge with a weakened form of dengue; by contrast 20 out of 20 placebo recipients developed viremia, 80% a rash. Importantly, TV003 elicits antibodies to all 4 dengue serotypes. At least two large clinical trials are being conducted, one in Brazil, one in Thailand.
- In this observational study, antibiotic exposure in babies was not associated with childhood obesity. It’s just one negative study; nonetheless, it would fascinating to get an interpretation from Marty “Missing Microbes” Blaser, who writes and speaks quite eloquently on this putative link between antibiotic overuse and the obesity epidemic.
- Here’s the study showing that dolutegravir significantly increases metformin exposures. These data led to a dolutegravir label change a few months ago, stating that metformin dosing should not exceed 1000 mg a day in patients taking both drugs. Dolutegravir and raltegravir have so few significant drug interactions, it’s critical to remember the important ones.
- Toxoplasmosis is associated with impulsive behavior and aggression. I gather toxo does the same thing to mice, making them more reckless — and hence more likely to be nabbed by cats (the source of the toxo to begin with). These studies on the neuropsychiatric effects of this parasitic infection in immunocompetent humans periodically appear in the medical literature; recent review here.
- Good targeted review of rapid TB diagnostics, in particular their use in low-prevalence settings. We’ve got a lot to learn from the extensive use of Xpert globally.
- Speaking of, the giant-pouched African rat can diagnose tuberculosis. It’s multi-talented, as it also can find land mines — here’s their web site. Maybe it’s just me, but I find the UTI-detecting dogs much cuter.
In case De Niro wants a movie short to replace the one he’s now cut from the Tribeca Film Festival, he can show this one — it would be better than Dirty Grandpa.
[youtube http://www.youtube.com/watch?v=3aNhzLUL2ys]
March 20th, 2016
“Choosing Wisely” in HIV Medicine — Should We Stop Giving MAC Prophylaxis?
 (Disclosure: The following post represents personal opinion, and is in conflict with treatment guidelines. Proceed at your own risk.)
(Disclosure: The following post represents personal opinion, and is in conflict with treatment guidelines. Proceed at your own risk.)
E-mail recently from one of our outstanding first-year fellows:
Hi Paul,
I’ve heard you recommended against the use of MAC [M. avium complex] prophylaxis in most settings in the modern HAART era. We admitted a 21yo F patient, non-compliant with meds, with a CD4 of 2. She has poor tolerance of pills in general which has been a major obstacle to her care. Would you recommend against the use of MAC ppx in this patient? Even with a CD4 of 2?
Thanks.
It’s a great question, notwithstanding the use of the term “HAART”. (I think she did that just to bug me).
In general, I’m not recommending MAC prophylaxis anymore, and here’s why:
- It’s never been proven necessary in the modern ART era. For the record, this is the most relevant placebo-controlled trial, and it enrolled patients from 1992-1994—eons ago, ART-wise (only available HIV therapies were NRTIs). There’s certainly no controlled clinical trial since 1996, when effective ART became widely available. This observational study from the HIV Outpatient Study (too bad it wasn’t the MACs cohort, ha ha) didn’t find any benefit, and this one from the early ART era was conducted in 1996-1997, a time when virologic suppression rates in clinical cohorts was 20-30%. Please tell me if I’m wrong and there are other more relevant studies.
- Effective HIV therapy reduces MAC risk much more than azithromycin ever did. Disseminated MAC was, along with CMV retinitis, one of those dreaded “final common pathway” OIs that occurred late in HIV disease, almost exclusively in patients with longstanding severe immunosuppression. The incidence of both of these conditions—especially if you limit diagnoses to non-IRIS cases—has dropped dramatically.
- Some of these advanced disease patients may have undiagnosed MAC. It could be clinical or subclinical, and you wouldn’t want to give low-dose “monotherapy” to them anyway. They might develop MAC IRIS, but do we have any evidence that MAC prophylaxis prevents MAC IRIS?
- High-dose, weekly azithromycin has side effects. These are mostly GI side effects, and I’d argue anything that might make it tougher for someone with a CD4 < 50 to take ART is a bad thing.
- Any antibiotic administered chronically selects for resistance, will alter the “microbiome.” Although clinical studies of MAC prophylaxis didn’t find much macrolide resistance in M avium, resistance to macrolides among other bacteria is widespread. And one dose of an antibiotic can alter the microbiome.
- It costs money. Not a lot, but something. And if it’s not doing any good, or even worse, distracting someone from taking ART, it’s bad value.
So could there be anyone in whom I’d still recommend MAC prophylaxis? I suppose—but without much enthusiasm, and only if all the following criteria were met:
- Newly diagnosed with HIV, or newly ready to take ART.
- CD4 < 50.
- No clinical symptoms or signs consistent with MAC.
- Expresses strong commitment to taking ART now that he/she has this serious diagnosis (AIDS).
In these cases, one could argue that it’s possible that giving it would provide some benefit during this very vulnerable period. If the patient takes ART, furthermore, the CD4 will soon be above the threshold allowing discontinuation of primary MAC prophylaxis,
But I’d have a very low threshold for stopping it (any GI toxicity in particular) even before the CD4 cell count is > 100, and would make it abundantly clear that this patient’s true lifeline to health is HIV therapy.
So what about a controlled clinical trial? It’s never going to happen—the incidence of MAC is too low these days, so the sample size would need to be untenably large. Additionally, finding and enrolling patients who meet the CD4 entry criteria would be an enormous challenge. These are not the easiest patients to get into clinical trials.
So what say you, ID/HIV specialists—should we still be prescribing MAC prophylaxis?
March 15th, 2016
Dogs Again Are Brilliant Diagnosticians
The reputation of dogs in the ID world got a big boost when Dutch researchers published this remarkable study of Cliff — a beagle who was trained to “diagnose” C diff using his superior olfactory abilities.
(A couple of entertaining videos here, if you can’t get enough of this stuff. I can’t.)
Now, in the pages of Open Forum Infectious Diseases (IDSA’s open access journal, of which I’m editor), we’ve published another landmark study demonstrating the extraordinary sniffing powers of our best friends:
From the paper:
In this double-blinded case-control validation study, we obtained fresh urine samples daily in a consecutive case series over 16 weeks. Dogs were trained to distinguish urine samples that were culture-positive for bacteriuria from those of culture-negative controls, using reward-based clicker/treat methods …Dogs detected urine samples positive for 100,000 cfu/mL E. coli (N=250 trials; sensitivity 99.6%, specificity 91.5%).
Impressive! Not only that, but the pooches did equally well with other bacteria — Klebsiella, enterococcus, Staph aureus. An anecdote in the Discussion section of the paper highlighted the real-world performance of Abe (he’s a dog) when a sick person visited the training center — I encourage you to read the full paper (which is on OFID’s early access page) for the details. Not only that, but there’s an action shot of the experimental methods.
So how do the dogs do so well at this task? To start, it is estimated that a dog’s nose is over 100,000 times more sensitive than ours. Plus, there’s this astute comment from my Twitter feed:
Indeed, this diagnostic task is right in the “sweet spot”, as it were, of a dog’s abilities. As the paper notes, “Sniffing urine is innate behavior in dogs.”
Practice makes perfect. Woof!
[youtube http://www.youtube.com/watch?v=L4o68eyT26w]
March 9th, 2016
Approval of TAF/FTC/RPV, Another Single Pill HIV Treatment Option
 The approval last week of TAF/FTC/RPV — that’s coformulated tenofovir alafenamide, emtricitabine, and rilpivirine — brings us another one-pill, once-daily option for HIV treatment.
The approval last week of TAF/FTC/RPV — that’s coformulated tenofovir alafenamide, emtricitabine, and rilpivirine — brings us another one-pill, once-daily option for HIV treatment.
It’s essentially the same as the existing TDF/FTC/RPV, with similar pros/cons, but with three notable differences coming with the substitution of TAF for TDF.
Specifically:
- Likely reduced renal and bone toxicity. Since approval was based on bioequivalnce, this hasn’t (yet) been proven in clinical trials — switch-studies are ongoing, comparing TAF/FTC/RPV to both TDF/FTC/RPV, and TDF/FTC/EFV. Note that this might end up being a more relevant consideration with TDF/FTC/RPV than TDF/FTC/EFV, since the former is taken with food and hence leads to higher tenofovir levels.
- A smaller tablet size. TDF/FTC/RPV was already the smallest coformulated pill for complete HIV treatment, and with 25 mg of TAF replacing 300 mg of TDF, the new pill is quite a bit smaller. For some patients, this matters a lot.
- A weird new brand name. It’s called Odefsey, which sounds kind of like the famous Stanley Kubrick film, without the “2001: A Space …”
We can assume (for now) that carried over from TDF/FTC/RPV is the generally well-tolerated profile (low risk of rash, GI side effects, metabolic abnormalities). As with TDF/FTC/RPV, TAF/FTC/RPV should be taken with food and without concomitant PPIs to maximize RPV absorption. It is not intended for treatment-naive patients who have HIV RNA > 100,000 copies/mL.
So this is a nice advance, especially for those patients at risk for renal and/or bone disease. Little reason not to switch existing TDF/FTC/RPV-treated patients to this new formulation, at least once payers add it to their formularies. (As with ECF-TAF, the listed price of TAF/FTC/RPV is the same as TDF/FTC/RPV.)
Note that arguably a bigger TAF-related approval — the TAF/FTC pill, already nicknamed “TAF-ada” — is expected next month.
[youtube http://www.youtube.com/watch?v=KliLsBSo-J4]
February 28th, 2016
Really Rapid Review — CROI 2016, Boston
The Conference on Retroviruses and Opportunistic Infections (CROI) returned to Boston last week, bringing together over 4000 HIV researchers and clinicians from all over the world.
And note I put “researchers” first — this is certainly the only conference I attend where we are asked to list published papers as part of the registration process! You can almost imagine the program committee reviewing the papers we enter, calculating impact factor and counting first- and last-author contributions.
(I don’t think they really do this. At least I hope not.)
Challenging registration process notwithstanding, the conference organizers are to be credited with releasing the dates of CROI way in advance, greatly facilitating academic and vacation calendars. As the graphic shows, it will be in Seattle next February, back in Boston the following year.
Here is a carefully curated (I’m joking) list of highlights, a Really Rapid Review™ roughly divided into epidemiology/prevention, treatment, complications, cure — and coffee.
- In the United States, the CDC projects that the lifetime risk of acquiring HIV among men who have sex with men (MSM) is 1 in 2 for blacks, 1 in 4 Hispanics, and 1 in 11 for whites. Lots of press for these alarming data. I’m an optimist, so I’m betting the under on these estimates given our advances in HIV prevention (PrEP in particular), and the fact that we now treat everyone with HIV.
- In the iPrEx study, higher TDF/FTC levels on PrEP were associated with declines in renal function. These data, and the expected approval of TAF/FTC next month, of course raise the question about the use of TAF/FTC in PrEP. Since you asked …
- Tissue and blood levels of tenofovir after TAF administration are much lower than with TDF. Understandably, this raises a concern about use of TAF/FTC for PrEP. BUT …
- In an animal model, TAF/FTC protected 6 macaques from acquiring SIV. These are encouraging data, and suggest we don’t really know the optimal biological correlates of protection with this drug combination. Bottom line: Whether TAF/FTC will work for PrEP in humans remains unknown — and is a big clinical research challenge.
- In this meticulously detailed case report, a person taking PrEP with TDF/FTC acquired a multi-drug resistant strain — 5 TAMS, Y181C, even integrase resistance! This rare event isn’t enough to change policy or practice, but it’s a reminder that no prevention intervention will be 100% effective 100% of the time.
- Maraviroc seems like an ideal prevention drug given its mechanism of action and expected concentrations in relevant “compartments”. However, in this study of MSM, all 5 patients who acquired infection were receiving maraviroc-based PrEP.
- In separate studies (here and here), a dapivirine-impregnated vaginal ring significantly reduced the risk of HIV infection among African women (paper of one of the studies published here) — but the effect was modest. As in other studies, adherence played a key role, and younger women were not protected at all.
- In MSM at low risk for acquiring HIV, injectable cabotegravir was well tolerated (and preferred to oral therapy), but the q12 week injection schedule did not reliably achieve desired trough concentrations. One cabotegravir subject acquired HIV; trough concentrations were low. A q8 week schedule for PrEP seems likely.
- In this Kaiser cohort study, the “survival gap” between those with and without HIV is closing (13 years overall, 8 years if ART is started with CD4 > 500) — and much of the gap is now attributable to modifiable health risk factors, such as smoking.
- On the other side of the HIV treatment spectrum, this ambitious study evaluated the optimal strategy for retaining in care hospitalized HIV patients with addiction — including intensive patient navigation efforts and cash payments for certain desired outcomes (follow-up visits, picking up the antivirals, virologic suppression). The result? Payment “for performance” with the navigation worked — but only during the 6 months of the intervention. By month 12, the outcome of viral suppression was not significantly different in those with incentives from those who received “treatment as usual.”
- In this British Columbia cohort — where they have meticulous records of treatments and test results — HIV drug resistance to NRTIs, NNRTIs, and PIs has significantly declined since 2009, while integrase resistance has increased. The good news: Integrase resistance is still really, really rare.
- In this randomized clinical trial, stable patients taking TDF/FTC who switched to TAF/FTC maintained virologic suppression and experienced improved renal and bone outcomes. As noted above, approval of TAF/FTC is expected soon — and there are a lot of patients receiving this drug combination.
- Injectable cabotegravir and rilpivirine given every 4 or 8 weeks maintained virologic suppression as well as oral therapy. Importantly, no resistance was detected in the one patient who experienced virologic failure. Larger studies planned.
- In a reprise of the EARNEST and SECOND LINE study results, patients failing first-line dual NRTI plus NNRTI-based therapy did comparably well with LPV/r plus either RAL or NRTIs — despite having extensive NRTI “resistance”. Note the quotation marks around resistance, that was intentional since obviously there’s plenty of residual activity.
- Related to NRTI resistance — in this cohort of nearly 2000 patients with treatment failure on TDF, FTC or 3TC, and an NNRTI, the rate of tenofovir resistance ranged from 20% (Europe) to 60% (Africa). Use of 3TC (vs FTC) and NVP (vs EFV) were predictors of tenofovir resistance. Note that TAF is in vitro active vs K65R-containing viruses.
- In this clinical cohort in Amsterdam, there was an unexpectedly high rate of discontinuation of dolutegravir (16%), mostly for sleep, GI, and neuropsychiatric complaints.
- By contrast, this cohort study found no increased risk of virologic failure switching from RAL to DTG. This analysis should be repeated looking at switches from boosted PIs to DTG.
- Viral decay in the two-drug pilot trial of DTG + 3TC (PADDLE) was comparable to the three drug arms from the SINGLE and SPRING-2 studies. Another single-arm study of DTG and 3TC is ongoing (ACTG 5353).
- At 48 weeks in this phase 2 study, the NNRTI doravirine was similar to efavirenz, both arms with just under 80% virologic suppression. Despite these relatively low response rates, there was no drug resistance detected in either study arm; CNS side effects were lower with doravirine. Phase 3 studies of DOR ongoing — and yes, the drug will need to be abbreviated “DOR” since “DRV” is taken.
- This long-acting NRTI MK-8591 — and I mean really long acting, with a half-life of 150 hours with oral administration — induced nearly a 2 log decline in HIV RNA at day 7 after a single 10 mg dose. PrEP candidate? Part of an implantable device? Some other “paradigm shifting” treatment?
- In a European cohort, fractures were 3x more common in HIV positive patients than in the non-infected population. Among antivirals, only tenofovir independently increased the risk of fracture. Osteonecrosis was 100X more common; no specific drug exposure could be implicated.
- Most of the bone loss after starting ART occurs early, but in this study, a single dose of zoledronic acid completely blunted this adverse effect. If this bone loss phenomenon is due to immune reconstitution, one could imagine this intervention one day becoming standard of care.
- In the NEAT study comparing DRV/r plus either RAL or TDF/FTC, RAL increased trunk fat more than TDF/FTC. The study used DEXA, so could not determine if this was subcutaneous or visceral fat, or both.
- Compared to placebo, the quadrivalent HPV vaccine in “older” (age 27!) HIV-positive adults did not reduce new HPV infection or improve the course of anal dysplasia (HSIL). Study stopped early for futility.
- In a highly TB-endemic region, patients with a low clinical suspicion of having TB did not benefit from empiric TB treatment. In hindsight, this was kind of a self-fulfilling prophesy.
- There are many “real world” HCV treatment cohorts out there, and thus far most demonstrate outstanding cure rates in clinical practice, comparable to clinical trial results. Here’s another one (from Germany) which shows a 98% SVR12 among those treated for 8 weeks with LDV/SOF.
- In a study of 26 patients with recently acquired HCV (negative HCV antibody within past 6 months), 6 weeks of LDV/SOF cured 20, with 4 virologic failures — 3 relapses, 1 reinfection. The relapses all had HCV RNA > 9 million copies/mL, adding to data that HCV RNA is a critical determinant of optimal treatment duration.
- The ION-4 study of LDV/SOF for HIV/HCV co-infected patients, only 10/335 experienced virologic relapses. Nine (one didn’t participate) were successfully cured with a subsequent 24-week course of LDV/SOF + RBV.
- Treatment of 9 SIV infected macaques with two different TLR7 agonists induced viral blips and in some reduced the SIV reservoir. Most attention-grabbing: two of the monkeys are now off ART for 3-4 months, with no viral rebound. Stay tuned!
- In virologically suppressed patients, romidepsin (a “latency reversing agent”) and an immunologic boost with Vacc-4x adjuvanted with GM-CSF led to a modest decline in HIV DNA (one marker of the viral reservoir). Viral rebound after stopping therapy, however, appeared unaffected.
- This patient with acute leukemia received a stem cell transplant from a CCR5 negative donor, and has no detectable using sensitive assays — sounds like the n=1 case of HIV cure. Importantly, he remains on ART. Weird that this case is also from Germany! Fingers crossed.
- This cohort analysis demonstrated improved survival among French coffee drinkers with HIV/HCV coinfection. I’ll add this to my list of studies demonstrating the health benefits of coffee — a lifelong quest.
- The plenaries/review lectures this year were excellent — including in particular Bruce Walker on cellular immunity, Jerry Friedland on the intersections of HIV, TB, and poverty, Joe Eron on HIV treatment, Grace McComsey on fat, Paddy Mallon on bone, John Brooks on the HIV outbreak in Indiana, and Eric Rubin on Cheetos — I mean TB. (You had to be there.) All are available on the CROI web site here.
A bit of Boston- and venue-specific news. First, the weather was downright balmy, with temperatures one day pushing 60 degrees and thunderstorms (!) one evening. Last year’s record snow? No problem — it melted long ago.
And I happened to chat with someone who works at the Hynes Convention center, who assured me that the WiFi would be better in 2018.
So what did I miss?