An ongoing dialogue on HIV/AIDS, infectious diseases,
October 15th, 2018
Outpatient Antibiotic Prescribing Boosts Patient Satisfaction Scores, Rewarding Bad Medical Practice
A recent study confirms what every busy clinician already knows.
Many patients seeking care for respiratory infections expect to receive an antibiotic. When they get one, they’re happier than if they don’t.
Among 8437 patients seeking care for a respiratory tract infection in a direct-to-consumer telemedicine service, 66% received an antibiotic. The rate of prescriptions prescribed by physicians ranged from 19% to 90%, showing that these were not exactly evidence-based decisions. Satisfaction ratings strongly correlated with adjusted antibiotic prescribing rates (Pearson correlation, 0.41; P < .001).
It’s even worse if you look at the figure — none of the MDs in the lowest half of prescribers exceeded the 75th percentile for patient satisfaction.
More details:
Few physicians achieved even the 50th percentile of satisfaction while maintaining low rates of antibiotic prescribing. To reach the top quartile, a physician had to prescribe antibiotics at least half the time; almost all physicians above the 90th percentile had a rate of antibiotic prescribing greater than 75%.
This isn’t the first time we’ve seen data like these. In this earlier study comparing immediate versus deferred versus no antibiotic (along with a patient education intervention), patients with the immediate antibiotic prescription were significantly more likely to be very satisfied with their care — even though clinical outcomes were, not surprisingly, the same.
Jeffrey Linder — who studies appropriate outpatient antibiotic prescribing — would no doubt remind me that not every study demonstrates this effect of antibiotic prescribing and increased patient satisfaction. While this is true, his group just presented data that many antibiotic prescriptions aren’t written in the context of a patient visit, and often for diagnoses not even related to infection.
I asked a physician who works with one of the companies charged with assessing patient satisfaction what he thought about these recent survey data. He made the excellent point that it was physician communication — time spent talking with patients — that most powerfully drove patient satisfaction.
While no doubt this is true, let’s imagine you control for this talk-time. And that clinicians in urgent care centers and telemedicine systems are graded on volume (productivity) and patient satisfaction scores. Some would undoubtedly consider the counseling and education piece too time consuming. Remember, it was urgent care centers that had the highest rate of inappropriate antibiotic prescribing in a study published earlier this year.
What’s the fastest way for urgent care and telemedicine clinicians to achieve higher scores in patient satisfaction and “see” more patients/hour? In our action-driven society, it’s doing “something” (antibiotics, pain relievers, sleep aids, MRIs, you name it) rather than “nothing” (observation). It takes energy and time to explain why the latter is often the right choice.
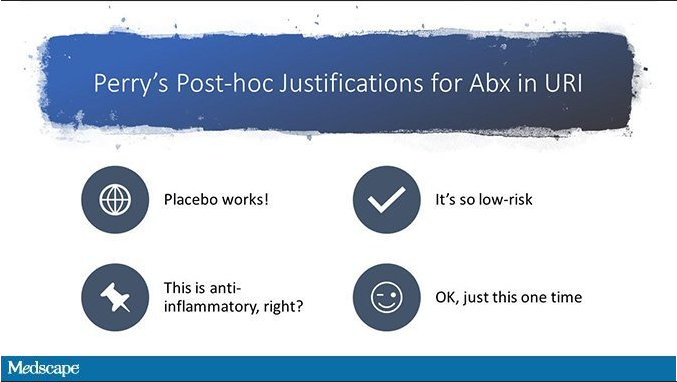
If you doubt my ID-doctor biased perspective, here’s another interesting view on this study from F. Perry Wilson on Medscape:
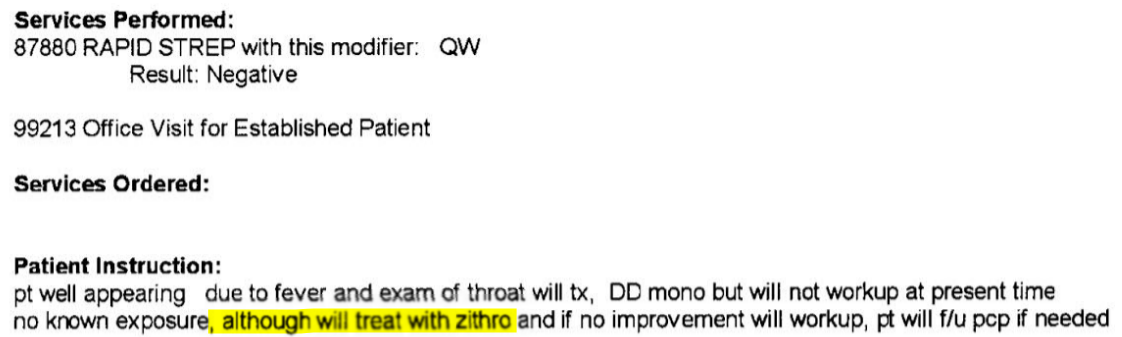
All of this leads to an all-too-familiar patient encounter, typified by this note from a local walk-in center:
Finally, could anything comment more appropriately on this relationship between antibiotics and patient satisfaction than this New Yorker cartoon?
So what are we going to do about it?


As someone specializing in C diff and FMT this makes me TOTALLY INSANE!!
Perhaps I should generate some brochures with horrible descriptions and pictures of patients with recurrent C. diff infection that doctors could hand out. Somehow I doubt that would plump up ‘patient satisfaction scores.’ I don’t tell my accountant how to do my complicated taxes; why do people tell us how to practice medicine!?
I JUST gave a lecture to nursing students yesterday about C. diff. and antibiotics. Hopefully, I drove my point home with all the scary images I used. (And data, of course, data!)
I do think this needs to be treated like the public health issue it is, complete with a media campaign. Something like, “This is your colon before you took that unnecessary antibiotic for your cold”, with a photo of nice, pink, healthy mucosa. And, “This is your colon after you took that unnecessary antibiotic”, with a photo of weird-looking, bright yellow pseudomembranes. We’d need a campaign directed at prescribers, too. (Could we get rid of Press Ganey scores, while we’re at it? I know, I know.)
P.S. Paul, you’ll be happy to know that thanks to one of your blog posts, I taught my students the new nomenclature for C. diff. Now if only the CDC would get Clostridium difficile changed on their website. 😉
This seems to be a strong argument for ethical prescription of placebo. “A lot of people find that this helps them feel better.” Ted Kaptchuk at BIDMC here in Boston has a number of studies of the value of prescribing placebo in a non-deceptive way. This seems like the obvious place to do it. In any case, we can guess that very few of the satisfied customers receiving antibiotic prescriptions have anything actually approaching informed consent: “I am going to write you a prescription for a medication which will not benefit you, but will expose you, and everyone else, to a significant risk of harm.”
The horse has been out of the barn for a while. It’s going to take a while to get it back in there.
Lots of forces at work here. Meanwhile I am deeply grateful my group doesn’t use patient satisfaction scores.
Following up on the public health/education approach, maybe require that a hand out be given to the patient by the prescriber (not the pharmacist) every time an antibiotic is prescribed for respiratory infections, complete with color pictures of the Cdiff colons versus normal colon, luridly presented statistics about harm, and with lots of links to CDC and ID websites about inappropriate antibiotic prescribing that people can tweet on to their friends. This is a simmering public health emergency and intervention at the Federal level is needed to break the positive feedback loop of patient demand driving antibiotic prescribing, validating patient demand.
And no discussion of antibiotic stewardship is complete without talking about the disgrace of allowing antibiotics in animal feed. Anyone have friends in the agriculture department?
And, this is one of the biggest issues but patient satisfaction scores are also affected by a variety of other factors such as physicians agreeing to order the tests that the patients would like or ordering other meds that the patients heard/read about somewhere etc..whether evidence supports their requests or not. And, in general, when sometimes physicians are busy and do not have the time (or inclination, because face it – it more often than not results in an dissatisfied patient and and foul mood for the rest of the day and if there are more patients like that then stress levels build up) to argue with patients against their requests, they may give in and they may actually be getting better patient satisfaction scores (even if it means they have actually caused more harm to the patient by ordering unnecessary tests/treatments).
We have a long way to go to figure out how to do no harm to patient, practice only evidence based medicine but at the same time keep the satisfaction scores high…
Change the payment structure.
If I suggest (3) 200 mg Advil, Level 2 visit.
If I Rx Ibuprofen 600 mg, Level 4 payment.
“Every system is precisely designed to achieve exactly the results it gets.” -Berwick
As an internist working full-time in urgent care, I can tell you this is true. However, if one spends 20 seconds explaining the no-Abx rationale to the patients, then most appreciate it and feel satisfied, some even appreciate that more. Then there are a few who will be unsatisfied if no Abx prescribed, but as the doc you have final say. As long as we remember that there’s a reason Abx aren’t over the counter – we are the gatekeepers and it’s our obligation and responsibility to make sure we guard those gates well, we can reduce resistance in the community.
A continued variation of the “Do something” mentality of modern practice. The patient wants an antibiotic, opioid pain medication, another ultrasound to “see the baby”? Do you want good patient satisfaction scores? Better keep the consumer happy by giving them what they want, but only if it is covered by insurance and does not cost them anything
Change the technique for patient satisfaction surveys. The ‘Survey Monkey’ garbage in/garbage out style is certain to over reward over prescribers (not just abx, but benzos and opioids). It might be more costly for Big Insurance, but phone interviews would be more valuable
Prescribing opioids inappropriately also boosted patient satisfaction scores.
I found that the usual arguments failed to convince patients: CDC recommendations, drug resistance, risk of diarrhea and C. diff, lack of efficacy against viral infections, etc. Only ONE argument seemed to have any effect at all: the prolonged disruption in the microbiome after a single course of antibiotics…and (there’s some handwaving now, but for a good cause) the link between microbiome disruption and obesity. Now that I’m no longer seeing patients, I’ll pass this one on to the rest of you. You’re welcome to use it if you’re comfortable with the handwaving
Eliminating antibiotic treatment of viral upper respiratory tract infections and bronchitis, improving influenza diagnosis and treatment, and reinforcing prescription guidelines for pharyngitis and sinusitis could improve outpatient antibiotic stewardship.
The antibiotic usage paradox – where we as patients assume these treatments will cure all ills, and through our repeated requests for them, cause the number of ills actually cured to shrink – is a topic for discussion every time the cold and flu season rolls around. Hopefully strengthened public health policy will empower frontline healthcare professionals to protect antibiotics, employ alternative treatment options, and to educate the public so that in the long term we are better protected against antimicrobial resistance.
Nowadays there are too many online stores but all are not reliable, they are selling cheap meds only but result is not concern for them, i am only visiting reputed online store like mygenericpharmacy.