An ongoing dialogue on HIV/AIDS, infectious diseases,
September 2nd, 2019
New Antibiotics for CRE, Draft Lyme Guidelines, Cost of Measles Outbreaks, and More — a Labor Day ID Link-o-Rama
 Labor Day! Could summer really be over?
Labor Day! Could summer really be over?
Nah, we still have a few weeks — and as I’ve noted several times, this time of year (September-October) gives us far and away Boston’s best weather season.
On with the links.
- Data from electronic medical records can accurately identify the best candidates for PrEP. The challenge in primary care is finding the tiny proportion of a clinical practice that could benefit from PrEP — and here’s a way to have the medical record do it for you. This is very nice work here, with some controversy (apparently some might find this creepy). And note that this algorithm only worked in men.
- PCV13 may no longer be recommended to all immunocompetent older adults. Instead, “shared clinical decision-making” will likely become the guideline, based on the plummeting rate of invasive disease in those over 65 due to pneumococcal immunization of children. Great coverage here by Dr. Abigail Zuger, right here in our own NEJM Journal Watch. But big question — how best to engage in this process, a patient-driven strategy I suspect we’ll see increasingly in all sorts of guidelines going forward. And will it influence insurance coverage for the vaccine?
- Uptake of the new anti-CRE drugs — for treatment of CRE — is surprisingly slow. The previous standard of care (usually polymixins) is terrible, so what’s up? The probable explanation is a combination of unfamiliarity and (especially) high cost — especially since these are hospitalized patients.
- Here’s another study showing no clinical benefits to HIV regimens with high CNS penetration effectiveness (CPE) scores. Could it be time to abandon this as a desirable metric for HIV treatment? Except in truly unusual circumstances — so called “CNS escape” cases — suppression of HIV replication in the central nervous system tracks quite nicely with activity in peripheral blood.
- IDSA, the American Academy of Neurology, and American College of Rheumatology issued draft guidelines for diagnosis and treatment of Lyme Disease. Public commenting will close September 9 — final publication eagerly awaited!
- Chilling summary how Lyme can become an “identity.” Note that the author of this well-researched, difficult, but very fascinating piece never denies the existence of post-Lyme disease syndrome (which is very real), yet is accused of doing so in the comments. I suggest every ID doctor read both this and this account in The Atlantic, from a sufferer, who is just trying to get better, and doesn’t know what to believe.
- The Truvada lawsuit may be hindering PrEP uptake. People notice the ads soliciting cases from personal-injury legal firms — both patients on HIV treatment (including several of my own, who have asked about it), and individuals considering PrEP. Here’s a sample, on autoaccident.com (of course, where else). Hard to imagine this will be a good thing for anyone.
- People with perinatal HIV transitioning to adult care have high rates of treatment failure. In a time when essentially all people with HIV in care have suppressed viral loads, the fact that 56% of this cohort transitioning to adult care had viremia stands out starkly — and underscores how challenging care for this population can be.
- Even small measles outbreaks cost public departments a lot. Infuriating, because these government funded programs are not exactly swimming in money, or just sitting around waiting for other things to do. This outbreak in a Clark County, WA cost nearly a million dollars; the one in New York is pushing 20 million. If only there were a solution to the problem of measles … oh wait.
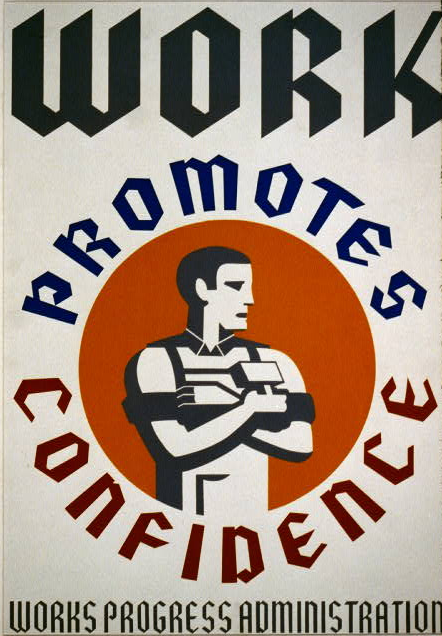
- This New Yorker piece summarizes some of the origins of the anti-science views fueling the anti-vaccine movement. It’s exceptionally well-written — I particularly like this tally: “Suspicion of authority, rejection of expertise, a fracturing of factual consensus, the old question of individual liberty versus the common good, the checkered history of medical experimentation (see: Tuskegee, Henrietta Lacks, Mengele), the cynicism of the pharmaceutical industry, the periodic laxity of its regulators, the overriding power of parental love, the worry and suggestibility it engenders, and the media, both old and new, that feed on it—there are a host of factors and trends that have encouraged the spread of anti-vaccination sentiment.” As for the media, I can’t resist posting this brilliant cartoon:
In the interest of balance… pic.twitter.com/pDLAzTPz5q
— TwistedDoodles (@twisteddoodles) August 22, 2019
(H/T to Keith Law for finding the cartoon.)
- HIV therapy and CRISPR-Cas9 eradicate HIV. In mice. Humanized mice, but still, mice. Have to start somewhere!
- With this recently approved Lyme antibody test, can we eliminate the need for the Western blot as a confirmatory test? The strategy would involve doing two immunoassays instead. Every ID clinician has experienced both the delay in diagnosis by waiting for the Western blot, as well as the rampant confusion over the results — especially with IgM results.
- Complex HIV regimens can be simplified even if there’s extensive background resistance. This certainly is our practice, but caution — you need complete resistance information! Plus, best to do close follow-up after making the switch, if for nothing else to reassure your patients who may be understandably fearful that fewer drugs will lead to treatment failure.
- Should serum β-D- glucan testing be used for the diagnosis of Pneumocystis jiroveci pneumonia? Two papers take opposite sides on this question, including one led by our former fellow (and now ID attending at Maine Medical Center) Dr. Jed Pilkington. (I was co-author.) I won’t divulge what side we took, but here’s the bottom line: The test is great if ordered in the right clinical context — but too often that’s not the case, and the results are frequently impossible to interpret!
- The number of reported cases of emergent dolutegravir resistance when part of an initial triple-therapy regimen is now up to 3. All cases involved very high baseline viral loads and low CD4 cell counts — 1,970,000 and 78 in the first case, 457,000 and 39 in the second, and 1,400,000 and 22 in this third one. Two also received rifamycin drugs. As noted in the title to the second case report, it’s time to conclude that selection of DTG resistance in initial therapy is “rare but possible.”
To finish — slow and steady wins the race (at least sometimes). I’ve watched this video too many times not to share it on this site, as it’s strangely compelling.


Loved the cartoon, Paul! Thanks for that. And thanks for the link to the Lyme article on The Cut/New York mag website. I had read the article in The Atlantic, but not that one.
Brilliant, Sir, as always. You are an unrelenting voice of reason in a culture that deprioritizes evidence and rational thought. Please never stop.