An ongoing dialogue on HIV/AIDS, infectious diseases,
May 4th, 2022
More on Relapses after Paxlovid Treatment for COVID-19
Unless you’ve been hiding under a rock, you’ve heard that some people treated for COVID-19 with nirmatrelvir/ritonavir (Paxlovid) experience a relapse in illness shortly after stopping treatment.
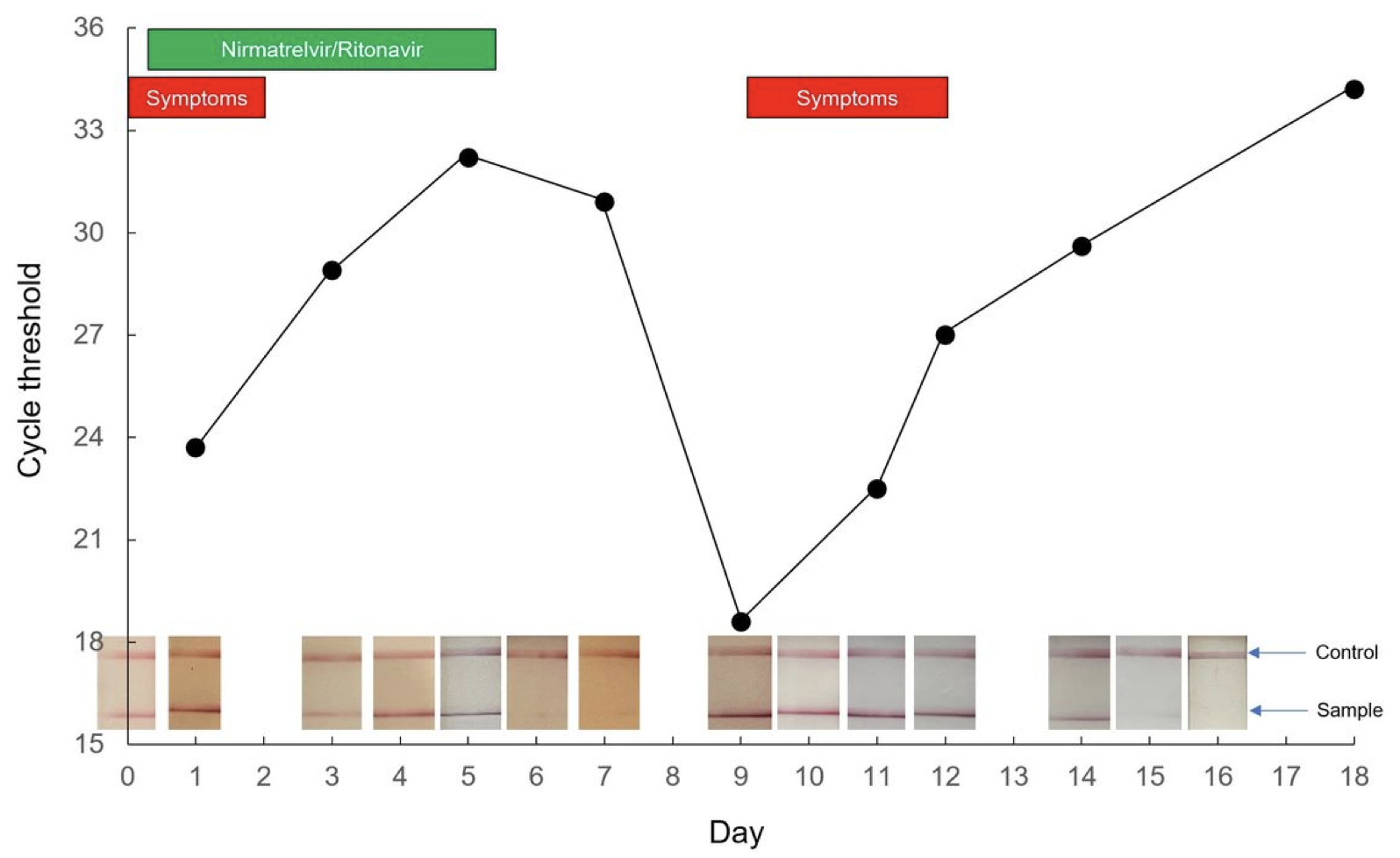
It’s both a recurrence of symptoms and a positive antigen test — sometimes after the test became negative. One case report published as a pre-print shows that a relapse can have a very low cycle threshold, meaning a high viral load:
Relapses vary in severity, from very mild and brief to worse than the initial illness. Check out the comments in my previous post for a sampling.
Some posit that the immune system doesn’t get a chance to mount a full response since the drug quickly reduces exposure to viral antigens. Others note that certain individuals experience prolonged viral replication, symptoms, and antigen test positivity, and perhaps it’s this group that’s destined to rebound after the 5 days of Paxlovid use. The drug knocks down replication for a while, but not long enough, so it rebounds.
Maybe it’s both — these aren’t mutually exclusive hypotheses. Regardless, as noted in my prior post, there’s still plenty we don’t know. But given the rapidly increasing use of Paxlovid nationally, I thought it worth this brief update about two important things we’ve learned since then, plus my opinion on a commonly asked question about contagiousness.
First, Pfizer offered additional details from their EPIC-HR study, citing that late viral rebounds occurred in roughly the same proportion of treated and untreated participants in their trial — around 2%:
UPDATE: Pfizer gave me the figures regarding the proportion of people who had Covid rebound in the Paxlovid clinical trial: About 2% of participants who got the drug experienced rebound, compared with ~1.5% of those who received the placebo rebounding within the same time frame.
— Benjamin Ryan (@benryanwriter) April 28, 2022
Whether the rate of relapse is higher than this 2% in clinical practice is unknown. Certainly, it seems that way — it even happened to a famous virologist! — but without knowing the denominator of total treated patients, we can only speculate.
And remember, clinicians have noted biphasic illness patterns since the start of the pandemic, and continue to do so. We’ve attributed that second period of worsening mostly to a robust (and sometimes hyperactive) immune response, but potentially there could be a component of concomitant heightened viral replication.
Second, in communications with clinicians, the FDA and Pfizer have made it clear that the people who relapse are in fact eligible for re-treatment under the Emergency Use Authorization (EUA). In other words, the within-5-day symptom clock starts over with the relapse. This would be justified clinically for our highest-risk patients (severely immunocompromised, medically fragile, or with severe recurrent symptoms), and favored over other outpatient treatments (all of which have logistical or efficacy issues) until we know more. So far, viral resistance has not been identified.
So where does that leave us with regard to infection control issues? In my opinion, we should assume that people who experience a symptomatic relapse with a positive antigen test could transmit the virus to others. Until data prove otherwise — meaning studies show these late relapsers have defective virions that are not replication-competent — this should be the recommended approach for work, school, and socializing. Symptoms plus positive antigen test equals potentially contagious.
In the meantime, I completely agree with this editorialist that we should be doing more to monitor how Paxlovid is doing since the EUA launched. I’m hoping large healthcare systems can quickly assemble observational studies evaluating how often this relapse phenomenon occurs out there in what is often called “the real world” — which means, in this context, “not in a clinical trial”. Prospective studies collecting virologic and immunologic data would also provide great value, especially given the theoretical concern that treatment blunts a favorable immune response.
So let’s keep learning.
You know, baby steps.


How long after finishing treatment does the relapse happen in those it’s happened to?
Thank you very much for the timely updates and sharing your expertise.
Your statement regarding repeating a course of Paxlovid for people who relapse appears to be in opposition to this FDA update from today which states:
However, there is no evidence of benefit at this time for a longer course of treatment (e.g., 10 days rather than the 5 days recommended in the Provider Fact Sheet for Paxlovid) or repeating a treatment course of Paxlovid in patients with recurrent COVID-19 symptoms following completion of a treatment course.
https://www.fda.gov/drugs/news-events-human-drugs/fda-updates-paxlovid-health-care-providers
Can you kindly clarify if the FDA allows for a second 5-day course of Paxlovid for relapse?
Thanks for your comment, I am aware of that FDA statement, and that there are no data on re-treatment. However, they have also communicated (when directly asked) that the wording of the EUA does not preclude a second treatment course. Hence in the population I described above — “severely immunocompromised, medically fragile, or with severe recurrent symptoms” — I believe it makes more sense clinically to re-treat rather than to choose the alternatives (which are more cumbersome or less effective), or to do nothing.
– Paul
The trials I saw not only excluded all vaccinated patients but also excluded most immunocompromised patients on active cancer therapy, and I think transplant, DMARDs etc. It makes sense to me that immunocompromised patients would be more likely to have longer infection and rebound. I’m curious as have seen vaccinated patients now rebound too (with paxlovid as well as biphasic symptoms). We need better data but no one is watching mild patients 10 days post infection to know if they’re symptomatic or still/again RAT +ve
I had rebound Covid. My symptoms started 4 days after testing negative from the first round. I had not heard of rebound Covid so didn’t test until I got very sick on day 7. Doctors at the Covid assessment centre were perplexed when I went in on day 8 and after calling colleagues said I could not do a second round of Paxlovid.
Thanks Dr Sax for sharing.
I had a patient with this and called Pfizer to see if they saw this in their study. The nurse manager we spoke to said they’d never heard of this. I posted his case o. Twitter @natedefelice on 1/30/22, and no response from Pfizer as well.
Disappointing they knew about this early and weren’t up front about it.
FYI my Twitter post with the history:
#IDtwitter #MedTwitter #PAXLOVID #OmicronVariant
75 yo m dm Vax3. 2wk ago covid. Day 3 took paxlovid. Symptoms resolved quickly. Had rapid ag & #lucira test – D7.
D14, had congestion and fatigue. rapid ag and positive!
#relapse ? Paxlovid=blunt immune response?
Thoughts?
Is there a place where we should be reporting relapses?
I am fully vaccinated (3x Pfizer in mid Jan 22), got first symptoms ~4/22, Paxlovid started 4/25 (day 3, with immediate results) and tested antigen negative 5/2. Symptoms similar to those in the beginning of the infection returned yesterday 5/4 and I’ve tested positive today, 5/5.
Dr Sax, thank you for your insights. Does the growing understanding of the definite risk for rebound change your opinion on prescribing Paxlovid for low risk individuals (as you discussed in an earlier blog post)?
I took Paxlovid within a few days of testing positive for Covid on a home test. I am vaccinated and boosted. Following the 5-day course, I tested negative on home tests for a couple of days; however, I was soon testing positive again and continue to have Covid a week later. I don’t know if Paxlovid has been a benefit to me or not. It was not a magic bullet.
Another note: both my wife and I, who took Paxlovid together, had a strong bitter grapefuit-like taste in our mouths while on Paxlovid. This taste went away almost immediately after we finished the treatment.
You state that the FDA has “made it clear” that a patient who relapses may be re-treated under the EUA. Do you have a citation for that?
If you contact someone from the agency and specifically ask, they will say that the wording of the EUA does not preclude a re-treatment. There are no data on this strategy, which is why in my opinion it should be limited to the population I describe above — “severely immunocompromised, medically fragile, or with severe recurrent symptoms”.
The alternatives are intravenous, or less effective, or doing nothing.
-Paul
Why would we consider retreating with a drug that could potentially be causing or adding to relapse potential in cases where there is relapse, especially considering the fact that patients taking this drug are already at risk for severe illness? Why aren’t there tighter controls on this drug which is only available under an EUA?
Until they know more, I would like to think it would make sense to go back into another 5 days of self-isolation and then mask up again when done once tested negative on an antigen test.
If worsening symptoms call the doctor and go to the hospital if need be.
COVID-19 is still so new, it’s not going away and yes, we may be in wave- lull pattern for at least another year. But, baby steps with this virus yes, we are going to be doing this for years and they are going to take years to perfect on it.
This is the biological and scientific end as well as the research end. And realistically we could be waiting around for everyone and their cousin to graduate from high school or complete CCD or whatever figuratively speaking which means,
Probably forever, which most if not all of our generation may not realistically be around for, and that’s in regards to awaiting COVID-19’s scientific conclusion and new perfected therapies. So, we have an extended isolation policy if rebound, just as one would do for the cold or flu. Thus, if we want to get to an answer, there needs to be a small double blinded clinical trial with paxlovid and placebo with rebound COVID-19 patients to see what occurs during second round of treatment course.
The goal remember here was to deal with the severe consequences and get the healthcare system back to being more manageable to treat other issues besides COVID-19.
With science and viruses one never knows what phenomenon is really going to occur in the real world until after release, use and studies and scientific reviews.
Imagine if we had to lockdown until all of that was completed to 100% perfection!
Hence, mitigation measures such as vaccination and vaccination mandates and masking mandates in public indoor environments. Those of you who have families imagine the mask and vaccination mandates as opposed to lockdowns for years upon years and you may not realistically be around to see them end, let alone your children/grandchildren complete their milestones, (communions, confirmations, graduations, becoming Eagle Scouts, etc) under perpetual quarantine as these events would not be in person. Instead, they would be virtual or not happen at all.
Although the drug includes ritonavir, could there be a secondary metabolic pathway leading to more rapid drug inactivation that would explain this?
My husband and I are both experiencing rebounds right now. We are fully vaccinated with me having one additional booster and my husband having two additional boosters. Original symptoms started and tested positive 5/2 and we started Paxlovid 5/3.
Tested negative and felt better by 5/8 and we both went back to work on the 7th day from symptoms. Yesterday 5/12 I noticed a very stuffy and runny nose starting. I thought it was maybe allergies. It got worse. When I got home I tested and the test was instantly positive with a dark line. I asked my husband and he said he had a little stuffy nose but we tested him too. He came up instantly positive as well. I have no idea what to do. Called the doctor and they said since it has been over ten days since original symptoms that we were no longer contagious and could work. We are both teachers. This is all so confusing and I wish there was somewhere to report this to that could give me advice.
Hi,
My course is similar to above , but for the record,
F,61, RN, Fully vaccinated and boosted x 2, Covid + Day 1 May 3, Ist dose Paxlovid Day 1 May 3, I was very sick, not hospitalized, Congestion, muscle aches, sneezing, runny nose, cough, headache, fatigue like I never experienced before, misery. Day 10 rapid home Antigen test Negative, symptoms much improved, very mild intermittent cough, enrolled in RECOVER trial, Day 11 , May 13, symptoms return, sneezing, runny nose, cough, malaise Rapid Antigen positive.
Similar to others experience, my symptoms were in remission Day 3 of taking Paxlovid but on Day 12 symptoms of congestion, coughing, runny nose and positive test. No clear communications about what to do now, Day15, except that if symptoms clear I can be out with mask on. Mixed messages about whether another 5 days on Paxlovid was warranted so I decided not to. I have also been told you can continue to test positive for some time. We need clearer communication and recommendations from CDC and Pfizer!
If one relapses on Paxlovid is there a contraindication to get monoclonal antibody?
My wife and I tested positive for the COVID antigen test during the initial 24-48 hours of symptoms. Both were strongly positive. We started on Paxlovid the next day. We immediately felt better but I became symptomatic with what I thought were allergies about five days after stopping Paxlovid. My wife continues to be asymptomatic and tested negative when I tested positive again. Feels like a bad cold. No SOB or other worrisome symptoms at this time. I guess I will just let it ride since my only risk factor is that I am 72 years old. Any suggestions?
I am taking Paxlovid now and am not vaccinated. My question is has anyone had the rebound cases and ended up in the hospital or were they just mild and eventually went away? I think it’s worth taking the Paxlovid as long as the rebound is not going to land you int he hospital.
I am immunocompromised with small lymphocytic lymphoma but have not been treated yet since my diagnosis over five years ago. It’s a monitoring known as Watch and Wait. Tested positive for COVID on May 7 and started a course of Paxlovid the same day. Felt better quickly and tested negative on May 12.
I resumed normal physical activity and began to have the same COVID symptoms on May 16 and tested positive again on May 17. On both occurrences the symptoms have been the same at least so far. Primarily it’s been like having a bad cold with runny nose, cough, headache and fatigue but no fever nor breathing issues. My oncology team has recommended that I do a second round of Paxlovid and I will do that.
I see that the advice on a second course of Paxlovid for a COVID rebound is conflicted but I’m willing to see if this time my recovery will be more durable.
I am vaccinated and boosted x2. Age 54. Tested positive for covid on 5/13 with cold symptoms and low fever, and began paxlovid that day. Finished paxlovid yesterday on 5/17, but I am still testing positive today (rapid test), 5/18. I am currently symptom free except for very very mild runny nose occasionally. I am terrified that my symptoms will worsen now that I have stopped paxlovid but am still positive.
Paxlovid received EUA based on one study of UNVACCINATED people. Doctors extrapolating data to justify giving Paxlovid to vaccinated patients, even ones with no high risk factors. Vaccination alone roughly 90% effective at preventing serious disease, so why prescribe Paxlovid for breakthrough cases and take risk of rebound which we seem to know little about, Dr. Sax ?
I am a physician who is fully vaccinated and boosted. Tested positive for covid. Took Paxclovid and felt better within 24-48 hrs. Went out of isolation. 8 days later woke up with same sore throat stuffy nose HA , tested positive again so assumed this was the rebound. Isolated again and on day 5 after rebound tested neg with rapid antigen. Went out if isolation. 4 days later had same symptoms and tested positive again with rapid antigen! The 2nd relapse was worse than the original infection and first relapse!! 3 positive rapid antigens in 3 weeks associated with same symptoms each time!!
I have much the same story as above with a twist as I believe I caught Covid from my husband during his own Paxlovid rebound. Husband was away from home and tested positive on 4/28, started Paxlovid 4/29, stayed away from home and isolated, recovered quickly and returned home symptomless on 5/6. Assuming he was no longer contagious he did not isolate at home but on 5/7 and 5/8 he felt some very mild sypmtoms. I started having symptoms 5/9 and tested positive 5/10 the same day I started Paxlovid. Symptoms were gone within 2 days and I had negative tests on 5/16 and 5/17. 5/18 my nose got very stuffy and mild body aches returned, becoming severe the next day with severe runny nose and sneezing and headache. Antigen test results have been positive again since 5/19. Today 5/21 still have extreme sinus congestion and post nasal drip plus brain fog. I started masking everywhere and taking more precautions but I have not fully isolated. I hope I have not infected others!
I have the classic case of rebound CoVid after Paxlovid. Started the Paxlovid on day 2 of symptoms, by day 5 felt much better and tested negative. By Day 10 symptoms returned — 100.7 fever, severe cough, congestion.
In addition to the possibility permitted by carefully reading the Paxlovid EUA of another five day regime of Paxlovid, is there any information about taking the Merck drug, Molnupiravir, to fight rebound CoVid after Paxlovid?
Is another possible choice for rebound Covid after Paxlovid the Merck drug, molnupiravir?
As many above. 68yr female dbl vaccinated and 1 booster. Treated with paxlovid in first 48 hrs of symptoms. Immediate help and return to normal by day 4 with negative covid test on day 6. A few days feeling normal then again symptoms I thought were allergies into they got worse and tested strongly positive again. Today 5th day of rebound COVID turned the corner to feeling on the mend. I think we are going to find that many more people are experiencing this than the trial data showed!
My husband got the rebound infection on day 10, after testing negative on day 5. Symptoms were worse than the first time. Scratchy throat, sinus congestion. It is currently day 17 since Initial positive test, still testing positive however. Symptoms are improving slowly. My husband is double vaccinated and double vax’d. he is 65. What is clear to me is that NO one of the medical experts actually knows anything really. We’re following your advice but it seems like guesses at this point.