An ongoing dialogue on HIV/AIDS, infectious diseases,
May 2nd, 2010
Learning from Clinical Trials with Limited “Generalizability”
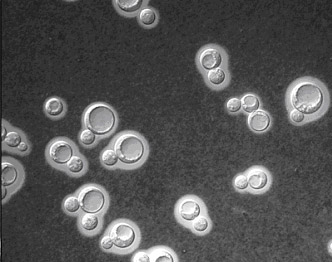 In the ongoing debate about when to start antiretroviral therapy in our sickest patients — those with acute opportunistic infections — comes this study from Zimbabwe of early vs. deferred ART in patients with cryptococcal meningitis:
In the ongoing debate about when to start antiretroviral therapy in our sickest patients — those with acute opportunistic infections — comes this study from Zimbabwe of early vs. deferred ART in patients with cryptococcal meningitis:
The median durations of survival were 28 days and 637 days in the early and delayed ART groups, respectively (P
=
.031, by log‐rank test). The risk of mortality was almost 3 times as great in the early ART group versus the delayed ART group (adjusted hazard ratio, 2.85; 95% confidence interval, 1.1–7.23). The study was terminated early by the data safety monitoring committee.
In sum, early ART made a terrible situation even worse: 3-year survival for the early ART group was only 22%, vs 46% in the deferred therapy group.
The challenges of applying this study to clinical practice here are numerous, including use of non-amphotericin therapy for cryptococcal CNS disease, lack of protocol-directed management of suspected raised intracranial pressure or immune reconstitution inflammatory syndrome (IRIS), and the highly unstable social and political situation in the country at that time.
Still — sometimes a study’s findings are so overwhelming that that there is something to be learned, issues of limited generalizabilty notwithstanding.
I suspect here it’s that ART should be deferred for at least a couple of weeks in patients with crytpotoccal meningitis, giving the amphotericin/5FC time to bring down the organism burden. Importantly, this slight delay would still be consistent with the “early” ART strategy of A5164, where the median time to start therapy was 12 days after OI treatment.
At least that’s what I’ll be doing until the results of this study are available.
Categories: HIV, Infectious Diseases, Patient Care
Tags: antiretroviral therapy, ART, cryptococcal meningitis, HIV
You can follow any responses to this entry through the RSS 2.0 feed. Both comments and pings are currently closed.
Comments are closed.

Paul E. Sax, MD
Contributing Editor
NEJM Journal Watch
Infectious Diseases
Biography | Disclosures | Summaries
Learn more about HIV and ID Observations.
Search this Blog
Follow HIV and ID Observations Posts via Email
Archives
-
-
From the Blog — Most Recent Articles
- ID Things to Be Grateful for — 2025 Edition November 24, 2025
- When AI Gets the Medical Advice Wrong — and Right November 18, 2025
- Hot Takes from IDWeek: CDC, COVID, and Two Doses of Dalbavancin November 13, 2025
- Favorite ID Fellow Consults: Johns Hopkins Edition November 7, 2025
- Two Covid Vaccine Studies — One Actionable, the Other Not So Much October 28, 2025
 NEJM Journal Watch — Recent Infectious Disease Articles
NEJM Journal Watch — Recent Infectious Disease Articles-
Tag Cloud
- Abacavir AIDS antibiotics antiretroviral therapy ART atazanavir baseball Brush with Greatness CDC C diff COVID-19 CROI darunavir dolutegravir elvitegravir etravirine FDA HCV hepatitis C HIV HIV cure HIV testing ID fellowship ID Learning Unit Infectious Diseases influenza Link-o-Rama lyme disease medical education MRSA PEP PrEP prevention primary care raltegravir Really Rapid Review resistance Retrovirus Conference rilpivirine sofosbuvir TDF/FTC tenofovir Thanksgiving vaccines zoster
