An ongoing dialogue on HIV/AIDS, infectious diseases,
March 21st, 2015
ID Learning Unit: Coagulase-Negative Staph, and the “Anti-Zebra” Residents’ Report
 At the risk of betraying a deep streak of nerdiness, I confess to being a huge fan of Residents’ Report. This infatuation goes back to my medical student days, when the occasional chance to watch the Chief Medical Resident — who seemed the smartest doctor on the planet — lead a discussion of an interesting case inspired all kinds of aspirations.
At the risk of betraying a deep streak of nerdiness, I confess to being a huge fan of Residents’ Report. This infatuation goes back to my medical student days, when the occasional chance to watch the Chief Medical Resident — who seemed the smartest doctor on the planet — lead a discussion of an interesting case inspired all kinds of aspirations.
Alas, I was never chosen to be Chief Resident, but have been lucky enough to sit in on my fair share of Residents’ Reports over the years, including one this past week. And so glad I did, as current Chief Resident Mary Montgomery tried a new twist on the genre: Instead of presenting a fascinating rare case — a “zebra” — or a challenging ongoing diagnostic dilemma, she chose a couple of extremely non-zebroid (that’s a word) cases that involved coagulase-negative staph (CoNS), a bug that frankly most of us think is pretty ho-hum.
But you know what? It was a great report, educational and entertaining, and here’s what we learned about this commonly encountered (but frequently challenging) entity:
- In the microbiology lab, a coagulase test is done on suspected staph isolates, looking for tell-tale clumping of plasma. Clumps = coagulase-positive (Staph aureus); no clumps = coagulase-negative. Watch!
- There are over 30 species of CoNS, with Staph epidermidis the most common — but you rarely see micro reports listing Staph epidermidis, since identifying the particular CoNS species is rarely helpful.
- Staph saprophyticus is a CoNS species that is the second most common cause of uncomplicated UTIs in young women. Fortunately, it’s sensitive to most antibiotics used to treat UTIs.
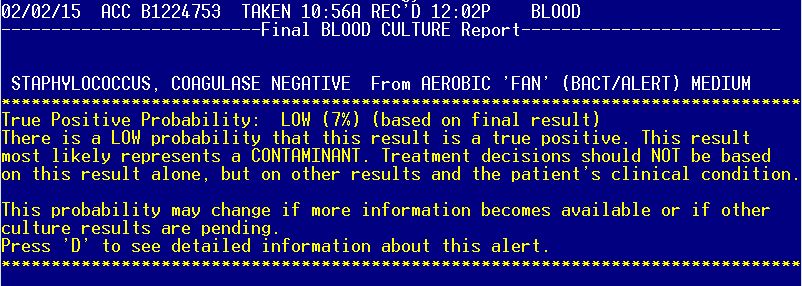
- CoNS are the most common isolates from blood cultures, and also the most common contaminants. Distinguishing true- from false-positive blood cultures can be tricky, in particular with CoNS, and this home-grown study provides some guidance — indeed, it’s incorporated into our ancient electronic medical record. (See above image — soon to be retired, alas, in a move of EPIC proportions.) Question: Has this study been updated by anyone?
- Clinically important infections with CoNS frequently involve prosthetic joints, mechanical heart valves, indwelling vascular catheters, ventricular shunts, vascular grafts, pacemaker or defibrillator leads, orthopedic hardware — in short, artificial ingredients!
- Treatment of choice for CoNS infection acquired in the hospital is vancomycin, since more than 80% are resistant to beta lactam antibiotics.
- CoNS are good at sticking to things, and have a virulence factor called arginine catabolic mobile element (ACME), which they unfortunately sometimes decide to transfer to MRSA. I hate when they do that.
- Production of biofilms — slime, think of the stuff that makes rocks slippery in a stream — makes CoNS difficult to clear from prosthetic material. Here’s a whole book about biofilms, great for leisure reading.
- Among antibiotics, rifampin seems to be the best at penetrating biofilms, hence its use as adjunctive therapy for many infections involving prosthetic material.
- Around 8% of native valve endocarditis is due to CoNS, and these patients have a high likelihood of requiring surgery. In my anecdotal experience they have an extremely indolent course, but not when the CoNS is Staph lugdunensis.
- Speaking of, Staph lugdunensis is a particularly aggressive form of CoNS, a wolf in sheep’s clothing that acts much more like Staph aureus than its wimpy coagulase negative brethren. It’s usually sensitive to beta lactams, too.
Of course I could go on and on about this last bug — we ID doctors adore Staph lugdunensis, which is both fun to say and is one of those factoids that separates us from the mere mortals out there who can’t be bothered to remember this arcane stuff.
Here’s a tip for you non-ID doctors: You can really impress your ID specialist friends by bringing up Staph lugdunensis when discussing a case, or even just in casual conversation:
Non-ID doctor: Hey, have you watched the new House of Cards season yet?
ID doctor: No, am waiting until I have time to binge-watch it.
Non-ID doctor: Makes sense. By the way, Staph lugdunensis.
ID doctor: Impressive!
Yes, I know. Time to get a life.


Thanks Paul. This reminded me of the period of time when coag neg Staph was reported as “Staphylococcus NOS” and the majority of house staff and fellows thought it meant Not Of Significance. Seriously.
Love these articles — good clinical pearls, great humor!
Thanks for making me laugh out loud, Paul. I hate House of Cards. Not a single character has any redeeming qualities, and thus I have no one to root for. I think my next dog’s name will be Staph lugdunensis. Tell your dog, Louie.
As usual, great writing and learning with lots of humor. Thanks!
These NEJM posts are so great. Just consulted on a patient who has S lugdunensis in blood now with recurrent positive cultures and endocarditis. I’m treating all S lugdunensis like MRSA right now!
Great discussion. Good point about artificial ingredients. I teach the residents that in “organic” patients, no arificial anything, CoNS is almost always a contaminant. Except of course, Staph lug.
Great piece !!!!! And yes, common things first.
Lugdunensis somehow linked to lovely Lyon (formerly Lugdunum) in France?