An ongoing dialogue on HIV/AIDS, infectious diseases,
July 1st, 2021
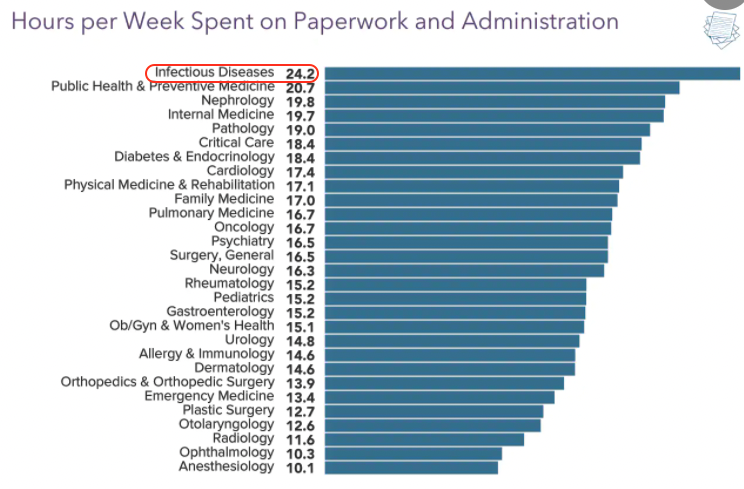
Five Reasons Why ID Doctors Are the Paperwork Champs
As they often do, the inquisitive folks over at Medscape polled doctors around the country on various topics.
This one hit home:
We're #1! https://t.co/4peKM1frWx pic.twitter.com/wwCrcXBrVI
— Paul Sax (@PaulSaxMD) June 17, 2021
Say what you will about Medscape’s methodology, or representativeness, or need for statistical analysis.
But we’re clearly #1 in the Paperwork and Administration category — and it’s not particularly close.
It’s also the very definition of a Pyrrhic victory — who wants this prize? — so let’s examine why this might be.
1. We take the best histories. We should celebrate this skill, as it is clearly our most important clinical procedure. After all, what other procedures do we generally do? That’s right, none.
But detailed histories take time — time to collect, and even more time to document.
Witness:
https://youtu.be/zHep6D_xxOo
These detailed histories, mind you, serve an important medical function and improve patient care — so often the critical missing piece of information arises in the process of collecting these data. I can much more strongly defend these histories than the common practice of cutting and pasting gobs of laboratory and other data into the note, the purpose of which is inversely proportional to its length.
Let the record show, however, that we were not put on this planet to provide the ideal source for a hospital discharge summary. Just imagine if we could collect royalties on every discharge summary that included a big chunk of an ID consult note — wow, we’d be golden.
2. We evaluate and manage complex patients — as a rule. Every doctor thinks their patients are the most complicated.
But since most straightforward ID problems are handled quite nicely by generalists, and no one gets an ID consult on patients who are doing well, the ID doctor’s rating of complexity is like the scale used on the WeRateDogs site:
This is Muffin. She hopes there’s still a spot on the Olympic team for her. Very confident this video is all they need to see. 14/10 pic.twitter.com/2uOyrUwJIx
— WeRateDogs (@dog_rates) June 29, 2021
That’s right — every case ranks at least an 11 on a 1-10 complexity score. Often higher. Like Muffin going for a swim up there. 14/10, go baby go.
In one of my favorite examples, I’ll cite again the landmark STOP-IT trial on the duration of antibiotic therapy for abdominal infections. Every ID specialist looked at the inclusion criteria — intraabdominal infection and adequate source control (emphasis mine) — and thought, “Who are these patients with adequate source control? Do they even exist?”
We have a resident rotating on our consult service right now who just did a consult on one such patient, and she couldn’t believe the complexity (certain details changed): The abdominal infection saga started in early-2020, and included a diverticular abscess, intestinal perforation, enterocutaneous fistulae, ventral hernia repairs, infected abdominal mesh, 8 separate admissions to three different hospitals, and innumerable polymicrobial cultures growing nearly every bacterial species in the MALDI-TOF database. Plus several different candida isolates.
“Adequate source control.” Ha ha ha.
3. We don’t give up. Shared, with permission, is this rant:
https://twitter.com/Boghuma/status/1407837071667040259?s=20
In the thread is further information that this application process started two months ago. Oh, and a later update — it’s still not resolved.
Who hasn’t faced the same thing when trying to get outpatient coverage for a novel antimicrobial? Omadacycline, anyone? Albendazole (the pricing of which is a true crime)? Tedizolid? Isavuconazole? I suspect we could fund an entire ID salary on the person-hours it has taken us to get our first few patients started on injectable cabotegravir-rilpivirine, which included a request for prescriber information that I didn’t even know existed.
And don’t get me started on clofazimine, which once upon a time was available by prescription, but now — just read about this painful process. Arghh.
COVID-19 brought with it an entire world of paperwork that previously didn’t exist, just like the virus SARS-CoV-2. Anyone who has tried getting monoclonal antibodies approved for inpatients with persistent COVID-19 probably thinks “EUA” stands for “Extra Unnecessary Activity.”
But we don’t give up. Because getting these obscure (and often frightfully expensive) drugs for people with difficult-to-treat infections is very much in our job description. So we do it.
4. We all have OCD — obsessive-compulsive disorder. I’ll never forget the sign-out I received from the graduating first-year fellow when starting my ID fellowship. A veritable tome, it weighed in at over a dozen single-spaced typed pages, each of them with the complete history, a detailed description of notable hospital events (surgeries, positive cultures, complications), antimicrobial courses (with doses), microbiology results, and assorted other factoids.
“I know it’s a lot,” she said, handing it to me. “But I’ve highlighted in yellow the things that need to be done today, and in blue those that might be important later.”
It was a color-coded masterpiece.
Look, we know we have a problem — and so does the rest of the medicine world, who gently tease us it about it periodically.
Here, take a look at the responses to this post:
What's more ID than writing an HPI that starts, "Briefly …"
… and then following it with a 1500 word note?
— Paul Sax (@PaulSaxMD) March 22, 2021
Many good responses, but this one truly captures it, from Dr. Joseph DeRose: “I do this as a prompt to tell myself to be concise … never works.”
Yep.
5. We don’t feel comfortable delegating work to others. I’ve thought about this one ever since my friend and neighbor, a thoracic surgeon, told me he had no trouble with our complex new electronic medical record.
“Barely look at it,” he said. “That’s what our PAs are for.”
Yes, he’s got a veritable army of support staff taking care of his patients — not just skilled PAs, but nurses, secretarial staff, scribes — and their responsibilities include note writing, prescription refills, prior approvals, insurance issues, filing, OR scheduling, patient transport, and likely also when to put new birdseed in his finch feeder.
No doubt this support he gets versus your typical ID doc is proportionate to the RVUs (otherwise known as RVU$) generated by an thoracotomy compared to a fever of unknown origin consultation. Still, the disparity remains quite stark.
But it’s not just that — often even when we ID doctors do have support staff to help us, we end up just doing things ourselves. I found one of my colleagues standing by the fax machine, in the process of sending a lengthy document to a skilled nursing facility so the staff there had the latest discharge summary on her patient. I asked her why she didn’t ask one of our (very nice) clinic staff to do it for her, and she looked at me as if I were some sort of prima donna physician, too elite to get his hands dirty using our ancient fax machine, which requires a hand-crank for power.
Yes, she’s as dedicated a doc as you could imagine — but is faxing documents a good example of a highly trained physician “practicing at the top of their license”?
So those are the Top 5 Reasons why ID is #1 when it comes to paperwork.
I’m sure there are others, but I don’t want to get all OCD about it!


Thank goodness I chose anesthesiology…..
It’s not just the weird drugs that sometimes take a long time to get approved. I once had a patient with Type 2 diabetes that was on Lantus insulin back when it was relatively new. His insurance company did not want to cover it and as usual, did not offer recommendations for a replacement. Even when I finally spoke to the pharmacist for PBM, she could not tell me of a suitable alternative. After two months, I was finally able to get his insulin covered. I am glad to see that there is now a “generic insulin” available at much lower cost.
By the way, as a family doc, I used to find that some surgeons would “punt” these requests for the family doc to handle. Another reason why primary care docs are near the top of the list.
With due respect to Dr. Sax, and Medscape, how many ID docs are doing:
– Disability forms
– Homecare forms
– Transportation forms
– Insurance forms
– School forms
– Sports forms
– Utility letters
– Work/school excuses
…
– and prior auths not just for novel antimicrobials but for new medications in all classes?
Family Medicine is clearly, *CLEARLY*, #1
(also OCD, also not giving up, also not delegating, and also managing complex patients … of all ages and stages. Oh, and we usually take pretty good histories too). Just sayin’.
ID, at least in my practice, does plenty of these assorted forms. Now that I have heard that FP is # 1, I can hopefully defer a lot of these to the PCP!
Alas, many of my patients do not have a PCP. Zounds…
I do all these things. I do work and school excuses and return to work releases and handicap parking and FMLAs and all of it for my HIV an non-HIV patients because frequently these things are related to the reasons that they are seeing me. In addition I AM primary care for my HIV patients and so are many others. A significant majority of my patients being treated for routine complex problems HAVE no PCP. We trained longer but make less than any other doctor group except peds. Meanwhile, while everyone readily acknowledges the challenges and importance of primary care, the relative attention shined at the particular problems of ID is limited. So I don’t think this post means that PCPs don’t have their own terrible difficulties- this is readily acknowledged. This was just an attempt to shine a light on a group who otherwise is not recognized enough as doing what they do and having the challenges they have.
As much as I want to argue (as a HIV/FM doc I can see both sides a bit), I have to concede. Managing OPAT requires much more intensive management than my FM home health patients, where I typically can just sign off the home health form.
The prior auths for many of my meds needing auths can be handled by my nurses who are great at what they do, however, to get some of the ID meds I use (CAB/RPV, valgancyclovir (sometimes), voriconazole, etc) I sometimes feel like I am writing a research paper with footnotes. This sometimes happens with newer antipsychotics too (vraylar, latuda, etc) but I don’t have to use them as often. I think the breadth of medications needing an auth compared to the RVU$ is probably pretty high for ID and I’ll buy that they probably beat me.
You never know when it will be important to document the name of the patient’s parakeet. That means you, Fruitloop.
I once had a surgeon tell me and my colleague that, after certain surgical patients had been in the hospital a very long time, he would get an ID consult to summarize the care that no one else could remember.