An ongoing dialogue on HIV/AIDS, infectious diseases,
April 21st, 2023
A Change-of-Season ID/HIV Link-o-Rama
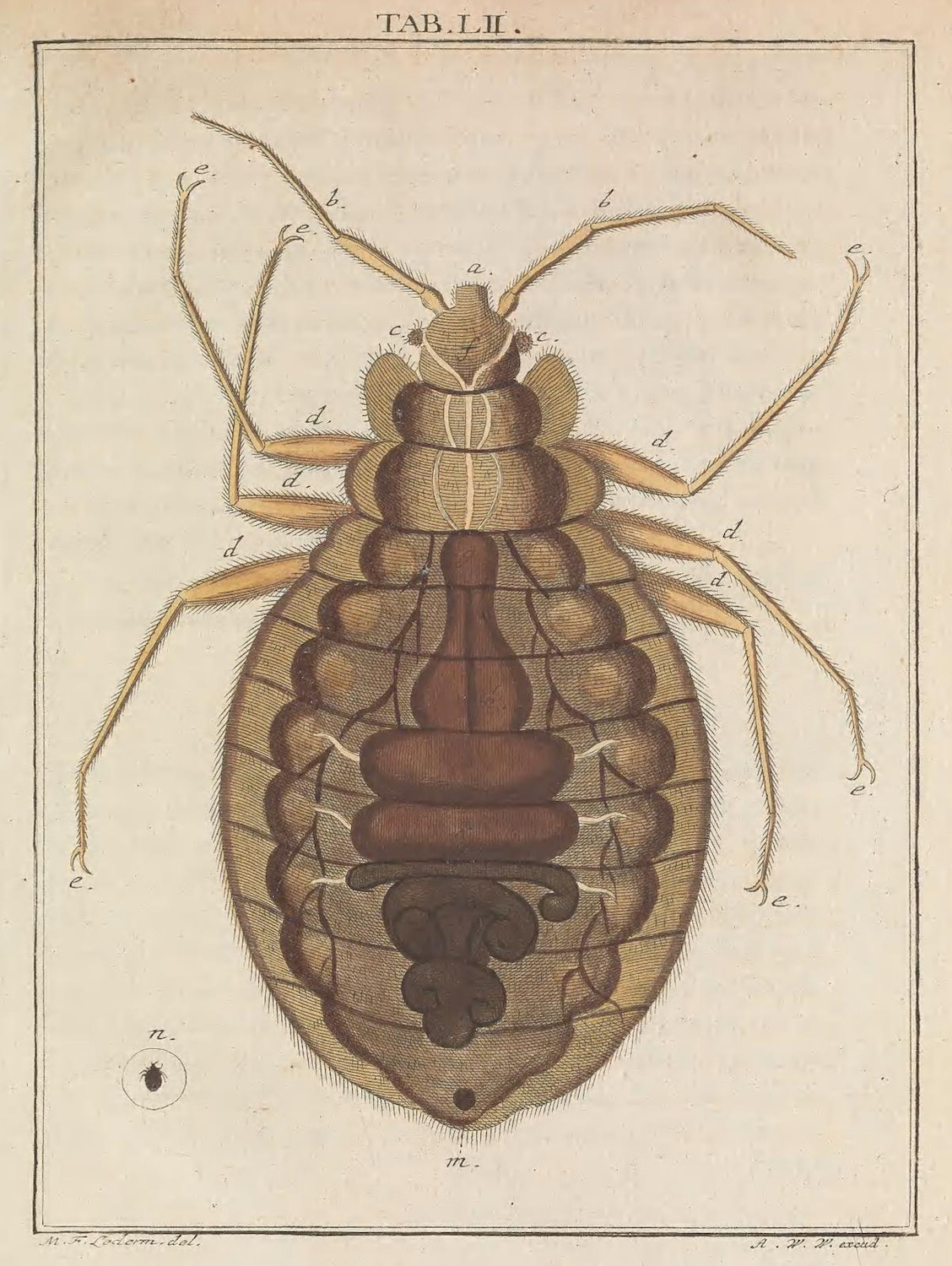
Bug, from Martin Frobenius Ledermüller’s Microscopic Delights (1759–63)
The warm weather takes its sweet time to arrive here in Boston, teasing us with an occasional comfortable day, but reverting frequently to chilly temperatures and high winds until mid-to-late May at the earliest. The afternoon sunlight might say, “Spring is here!”, but the nightly temps in the upper 30s/low 40s definitely say otherwise. Brrr.
Anyway, here are a bunch of assorted ID/HIV links of note, as the weather in Boston can’t decide between winter and summer — and eventually will skip spring entirely, as usual:
- Postexposure prophylaxis with one 200-mg dose of doxycycline reduced the risk of bacterial sexually transmitted infections (STIs). Based on this and two other studies from France, there is little doubt this strategy works. The key will be implementing it in the right population, which for now appears to be men who have sex with men (MSM) or trans women with a history of recurrent or multiple STIs. And of course, long-term risks (resistance, other adverse effects) remain unknown.
- An experimental RSV vaccine given during pregnancy reduced the risk of “medically attended” severe RSV-associated lower respiratory tract illness in infants. This was one of the co-primary endpoints; the vaccine was not significantly better than placebo for any medically attended RSV-associated lower respiratory tract illness within 90 days after birth. An accompanying editorial appropriately describes the “complex policy decisions” about whether to offer this vaccine to pregnant women, as another RSV vaccine did show a signal of increasing the risk of premature birth — one not observed here.
- A large study of statin versus placebo in people with HIV was stopped early due to efficacy. Participants were at low-to-moderate risk of myocardial infarction (MI), and had stable HIV disease; pitavastatin reduced the risk of major cardiovascular events by 35%. One particular area of interest will be how strong the signal of benefit is across baseline characteristics — I suspect that relative risk reduction will be preserved, but for some, the absolute risk will be quite low, limiting uptake. But add this study to the “put statins in the water” team.
- Prophylactic piperacillin-tazobactam prior to pancreatoduodenectomy (better known as a Whipple procedure) reduced postoperative complications significantly more than cefoxitin. The study stopped early due to the large beneficial effect of pip-tazo (which is how I avoid saying the expired brand name). This is the kind of clinical trial for common clinical strategies in ID we should see more often! I strongly suspect this one will change clinical practice guidelines.
- HIV incidence was higher among men choosing event-driven rather than daily PrEP. An important paper given both the relatively understudied population (MSM in West Africa), and the results — adherence to the event-driven strategy was significantly lower, clearly influencing the outcome.
- In a randomized clinical trial, participants receiving fluvoxamine plus inhaled budesonide had fewer ER visits or hospitalizations or complications due to COVID-19 than those getting placebo. Note that the dose of fluvoxamine is 100 mg twice daily, 2 times higher than in the negative COVID-OUT study. These positive randomized clinical trials (see metformin) in people immunized and/or previously having had COVID-19 ironically offer more direct evidence of clinical benefit in this immune population than molnupiravir — and some would say nirmatrelvir/r as well.
- In Staph aureus bacteremia, combination therapy with cloxacillin plus fosfomycin was no better than cloxacillin alone. We’re still awaiting a combination therapy study that shows “more is better” for this challenging clinical entity. The study was presented at the European Society of Clinical Microbiology and Infectious Diseases, often abbreviated to “ECCMID” — which is rapidly emerging as one of the premiere clinical infectious diseases meetings in the world.
- A man died of rabies even though he received appropriate postexposure treatment. In this, the first report of such postexposure prophylaxis failure, the authors speculate that his immunocompromised status was the cause. And while each detailed report of rabies reads like something from a horror movie — and keeps us ID docs up at night — an excellent accompanying commentary reminds us that rabies is very, very rare in the United States. Fortunately.
- Treatment with nirmatrelvir/r was associated with a lower risk of developing long COVID. Observational studies such as this one, which cannot adjust for unmeasured confounders, do not prove that treatment reduces the risk of long COVID, but they strongly suggest it — especially with the favorable results of the ensitrelvir placebo-controlled, randomized clinical trial, which I have summarized previously.
- A high dose of a nonpathogenic, nontoxigenic, commensal strain of Clostridia species significantly reduced the risk of recurrent Clostridioides difficile infection compared to placebo. The treatment, called VE303, came originally from healthy human stool samples, then was amplified using clonal cell banks. Though this is a small study requiring confirmation, these data plus those from the SER-109 trial strongly suggest that microbiome-based treatment will one day be part of C. difficile treatment and prevention strategies.
- Can fecal microbiota transplantation (FMT) be a viable treatment for patients who suffer from recurrent multidrug-resistant urinary tract infections (UTIs)? This is a tiny (n=5) but promising case series, showing reduced frequency of UTIs and decreased hospitalizations after FMT. Every ID doctor knows just how common multidrug-resistant UTIs are today, with much attendant misery.
- The “adjuvanted” HBV vaccine (Heplisav) induced protective antibody responses in 100% of vaccine-naive people with HIV (PWH). Importantly, the usual response to this vaccine among adult PWH is suboptimal (20-70%), so these are remarkably good results. A study with this vaccine in PWH who don’t respond to hepatitis B vaccine is ongoing.
- Candida auris is spreading — fast. A particularly worrisome observation from this CDC surveillance study is that echinocandin resistance was 3 times higher in 2021 than in the previous two years. Yikes.
- An outbreak of blastomycosis in a Michigan paper plant has sickened nearly 100 people. One person has died. This is the first non-lab occupational outbreak of this endemic fungal infection I can recall, and it is still undergoing investigation.
- A physician-patient described the experience of being sent home on IV oxacillin. The clinicians treating her chose this strategy despite her protests (she preferred an oral option) and, not surprisingly, the experience was not a good one. This account should be required reading for all who do hospital-only patient care to understand just how dismal the “OPAT” — outpatient parenteral antimicrobial therapy — experience can be.
- Should masks still be required in all healthcare settings at all times? It’s a nuanced pro and con look at universal masking in hospitals and clinics, ultimately concluding that the time for this strategy has passed. The authors are infection preventionists, many of whom I know well (disclosure). Certainly, there are strong opinions on this matter on both sides of the debate — here’s an alternative view.
- Universal testing of admitted patients for COVID-19 may have unintended negative consequences. In this prospective study of 2,794 admissions, 129 (4.6%) tested positive by PCR, and 54 (41.9%) were asymptomatic. From this group, 39 had a cycle threshold of >35 and were deemed noninfectious. Nonetheless, 23 had adverse consequences, such as delayed medical care, canceled surgeries, or inappropriate treatment. The flip side, of course, is that universal testing also may prevent in-hospital transmissions. We’re clearly in a transition phase in healthcare for both universal masking and testing!
- Differential time to positive blood cultures acts as a helpful diagnostic tool in diagnosing central line-associated bloodstream infections (CLABSIs). In this systematic review of over 20 studies, if the blood culture from the central line turned positive 2 hours faster than the peripheral blood culture, CLABSI was highly likely. An important caveat is that this didn’t do very well for Staph aureus or Candida spp., but we generally recommend line removal for these pathogens anyway.
- Antibiotic exposure is associated with an increased risk of inflammatory bowel disease. As noted by my colleague Dr. Sanjat Kanjilal, who alerted me to this paper, this large, population-based study shows that antibiotics have way more “off target” effects than just resistance, C. diff., and side effects.
Hey baseball fans — how are you liking the pitch clock? I’m loving it!
Landon Knack throwing an entire half inning vs. Pedro Báez throwing 1 pitch. pic.twitter.com/wHa2p6K7k8
— Rob Friedman (@PitchingNinja) February 27, 2023


This is a superb compilation of studies/stories relevant to non-ID as well as ID physicians. Thank you for this post, and please keep these coming periodically!
Important for people to understand that there are both benefits and costs to universal masking and testing. It’s going to be an interesting next year in hospital infection control around the country.
Interesting that they opted to use 3 doses of Heplisav instead of the standard 2 dose regimen. In our study of 67 PWH who had failed one or more courses of the recombinant vaccine, 58 (86.6%) responded to a 2-dose course of Heplisav. https://www.sciencedirect.com/science/article/abs/pii/S0264410X21012512?via%3Dihub
Thanks for taking the time and effort to provide that succinct informative summary
Very useful . Enables one to be aware of what’s in the “ air “ .
If you wonder how on earth fluvoxamine, an SSRI antidepressant, could work to modify Covid progression, read this https://www.nature.com/articles/s41380-021-01432-3.
Excellent! Thank you!