An ongoing dialogue on HIV/AIDS, infectious diseases,
May 15th, 2023
Types of HIV Papers — A Quick Guide
I spend a lot of my time reading HIV clinical research papers. A lot.
So here, for your viewing pleasure, is a poster I updated and modified from a brilliant xkcd web comic (using this tool), describing some common HIV clinical research themes.
Suitable for framing, it should prove helpful as you embark on your next research project.
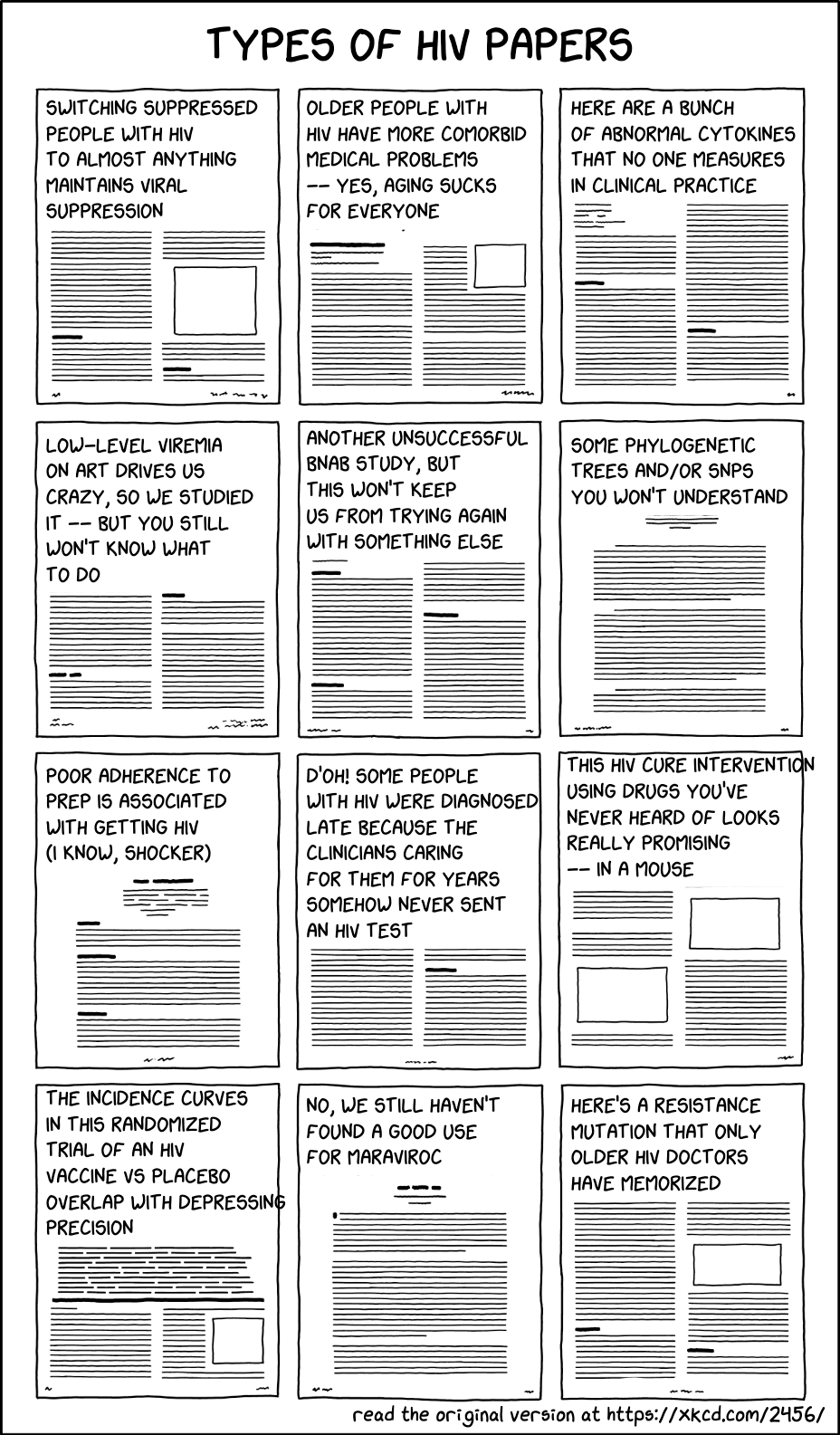
A brief commentary on the contents of these papers:
- Switching suppressed people with HIV (PWH) on antiretroviral therapy (ART) to almost anything maintains viral suppression. This is true for both biologic and behavioral reasons: there’s no viral replication at baseline, and only people with proven good medication adherence are eligible to participate. That means if it doesn’t work — like the raltegravir plus maraviroc switch — it’s pretty bad.
- Older people with HIV have more comorbid medical problems — yes, aging sucks for everyone. Everyone! No exceptions to the rule, alas.
- Here are a bunch of abnormal cytokines that nobody measures in clinical practice. They’re abnormal, yes. Clinical significance? Ummm … let me get back to you on that one. Or let me ask someone who loves cytokines, like the innovative and wonderful Dr. Irini Sereti.
- Low-level viremia drives us crazy, so we studied it — but you still won’t know what to do. I’m lucky to work with a guru of low-level viremia (among other things), Dr. Jonathan Li, a translational virologist and senior author on this fascinating study. He knows more about this annoying lab result — its causes and implications — than anyone on the planet. Good to have his number on speed dial, if “speed dial” is still a thing in a post-landline age.
- Another unsuccessful broadly neutralizing antibody (bnAb) study, but this won’t keep us from trying again with something else. Let’s try an even broader one! One that’s more potent! Let’s “extendify” it, using techniques of “extendification”, so it can be given less often! Then it might work. But if not, we’ll try again!
- Some phylogenetic trees and/or single-nucleotide polymorphisms (SNPs) that you won’t understand. Or at least, I won’t understand. Throw in a genomewide association study (GWAS) with a Manhattan plot, and let the confusion start.
- Poor adherence to preexposure prophylaxis (PrEP) is associated with getting HIV (I know, shocker). These are important studies from a behavioral health perspective, such as this recent one. But let me put this a different way — what if you had a strategy that clearly worked, but it wasn’t used? Would it still work?
- D’oh! Some people with HIV were diagnosed late because the clinicians caring for them for years never sent an HIV test. A remarkably common clinical error, even in 2023, sadly. Quoting this noted researcher in the title’s first syllable.
- This HIV cure intervention using drugs you’ve never heard of looks really promising — in a mouse. Or if not panobinostat, vedolizumab, or ipilimumab, how about some CRISPR?
- The incidence curves in this randomized trial of an HIV vaccine versus placebo overlap with depressing precision. Here’s the latest, alas. Oh well, it’s important to keep trying.
- No, we still haven’t found a good use for maraviroc. But still trying! Trivia buffs will know the clever brand name of this rarely used antiretroviral agent — Selzentry. Get it?
- Here’s a resistance mutation that only older HIV doctors have memorized. Guilty as charged. I’m still miffed that E138K is a resistance mutation for both nonnucleoside reverse-transcriptase inhibitors (NNRTIs) and integrase inhibitors. What’s up with that?
Ok, that’s a wrap. Am sure I left off some major themes, what else would you include?
Hey, dog lovers — is this you? (It’s definitely me.)
Greeting humans vs their dogs pic.twitter.com/NeGbEtd1n8
— Emma Pope (@emmerpope) September 21, 2022


Brilliant.
I’d add:
Adding or switching antiretrovirals to someone with HIV suppression does not impact neurocognitive impairment.
Recent ref from CID
Excellent list.
Need one for transplant ID!
Brilliant and thank you for the shout out!
I also loved “The Immune system is at it again” in the original version.
What is left out: Microbiome … but who really wants to go there? It merits its own “types of microbiome papers” (could be a challenge for a follow up post).
You’re welcome! After all, you are a true lover of cytokines! One day you’ll have to give me your opinion about the first one to enter clinical practice.
-Paul
You left out, “This vaccine doesn’t prevent HIV infection either” and its more optimistic cousin, “I don’t understand CRISPR but lets try a global CCR5-ectomy and see how it goes.”
Tim
🙂
Shock of recognition that I am responsible for contributing to many of these paper types.
(Not sure whether to apologize or be proud of that.)
Delightful! What about the “we compared x (disease/co-morbidity/co-infection/vaccine response) in HIV-positive people stable on ART with x in HIV-negative people. There was no difference.”
While the intent of this post would appear to reinforce the notion we all need to take a look in the mirror occasionally and not take ourselves too seriously, for me it misses the mark. Admittedly, I may not read a publication if it is a study in a mouse (no matter how humanized) and await the first in human trial (assuming I am not leading it), but everything has to start somewhere. I work in a field that has pursued the same vaccine target for 35+ years (malaria vaccines), and with each negative study there are lessons learned and incremental advancements in the field, such that we now have at least a partially effective vaccine and the prospects of doing considerably better. Sometimes belief (of a few) and dogged determination can get you somewhere and while one doesn’t have to agree with these efforts, they should not be belittled. If science and infectious diseases were easy we would be hitting home runs left and right – sadly, that is not the case. My hat is off to those in the research world – one of the toughest gigs out there…
A great list. Now in the age of CAB/RPV, even new HIV providers like myself have memorized E138K and other RPV-associated mutations. Vintage mutations can always come back in style!