An ongoing dialogue on HIV/AIDS, infectious diseases,
April 22nd, 2019
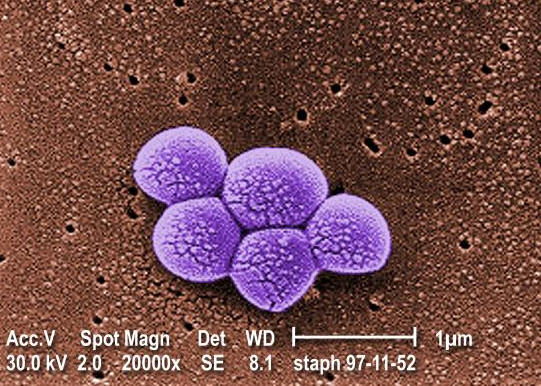
Two New Trials of Combination Therapy for MRSA Bacteremia Answer Some Questions — and Raise Several New Ones
Every clinically active ID specialist, hospitalist, and cardiologist realizes that treatment of bacteremia due to methicillin-resistant Staph aureus (MRSA) is no easy task.
In fact, it’s a problem so difficult that persistent bacteremia due to MRSA deserved highlighting here as an “Unanswerable Problem in Infectious Diseases”.
I wrote that over 5 years ago, and you know what? It’s still unanswerable!
One likely reason for the difficulty is that vancomycin kind of stinks as an antibiotic — there are molecular, pharmacologic, and potentially even immunologic reasons why it underperforms compared to beta-lactams.
Now, we have two new clinical trials to help move the field forward.
The first is the CAMERA2 study, just presented by Steven Tong at the European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), with summary below thanks to Erin McCreary:
https://twitter.com/ErinMcCreary/status/1118093904719618048?s=20
The study asked the question of whether adding a beta-lactam to standard of care therapy (vancomycin or daptomycin) would improve outcomes for adults with MRSA bacteremia. Some 356 adults were randomized to receive either monotherapy (vancomycin mostly, with some daptomycin) or combination therapy of vancomycin or daptomycin plus 7 days of an anti-staphylococcal beta-lactam (flucloxacillin, cloxacillin, or cefazolin).
The primary outcome was a composite one of several endpoints, looking at:
- 90-day mortality
- Persistent bacteremia at day 5 or beyond
- Microbiological relapse
- Microbiological treatment failure (positive sterile site culture for MRSA at least 14 days after randomization)
As pictured here, there was no significant benefit of combination therapy over standard of care — even though clearance of bacteremia was faster in the combination arm. The limitations of time to blood culture clearance as a surrogate endpoint echo what we learned previously when evaluating adding aminoglycosides to beta-lactams for treatment of MSSA — faster clearance of blood cultures, but no clinical benefit.
Importantly, participants who received combination therapy had significantly more acute kidney injury, and numerically higher mortality, leading to early termination of the trial. The post-hoc analysis showed that this renal toxicity was far greater with flucloxacillin/vancomycin than cefazolin/vancomycin, and hence the former cannot be recommended.
So, is that the end of combination therapy of vancomycin plus a beta-lactam for MRSA? Certainly not — as noted above, vancomycin treatment strikes most of us as suboptimal, and daptomycin is no better. In addition, the vancomycin/cefazolin strategy in CAMERA2 appears to be safe and may provide greater antimicrobial activity without increasing toxicity. The lead author suggested that this combination may be the next one tested by this group.
The second clinical study in MRSA bacteremia is a recently published pilot trial that randomized 40 patients with MRSA bacteremia to receive either vancomycin or the combination of daptomycin plus ceftaroline — italicized since it is the only FDA-approved beta-lactam with activity against MRSA, and hence fundamentally different from the combination strategy tested in CAMERA2.
Here are the surprising results:
Although the study was initially designed to examine bacteremia duration, we observed an unanticipated in-hospital mortality difference of 0% (0/17) for combination and 26% (6/23) for monotherapy (P=0.029), causing us to halt the study.
Wow.
But before we get too excited, here’s a critically important caveat — with such small numbers, these results could have occurred by chance, especially due to an imbalance of randomization (there were more patients with advanced lung cancer in the monotherapy arm). The authors acknowledge that the results must be considered preliminary due to the small sample size, and strongly encourage a fully powered study of this approach. Agree!
But what about ceftaroline alone? The drug is only FDA-approved for skin/soft-tissue infections and pneumonia; the lack of controlled data on ceftaroline therapy for bacteremia is an unfortunate data gap.
So, here’s a proposed study for MRSA bacteremia — a three-arm, randomized trial comparing:
- Standard-of-care (vancomycin or daptomycin, investigator’s choice)
- Ceftaroline alone
- Daptomycin/ceftaroline
Hey, we ID doctors can dream, can’t we?


Paul, Shouldn’t this be a 4 armed study and include cefazolin/vancomycin or is that impractical?
@easyasp
I have used Daptomycin/Ceftaroline combination for Vancomycin failure in the treatment of endocarditis with great results in at least 3 patients. Based on my experience I think the above mentioned 3 arm study is a great idea and should be conducted. I will not be surprised if survival advantage is found. Thanks!
And what about daptomycin plus fosfomycin? The BACSARM results presented in the las IDWeek showed some interesting results.
We have been using ceftaroline for vancomycin (or daptomycin) failures for several years now – casually defined as persistent fever or bacteremia or signs of ongoing inflammation despite pharmacologically appropriate Rx. Almost exclusively MRSA, total now = 8. Total successes (admittedly periodically with surgical drainage or valve replacement) = 6. Typical B-lactam toxicity’s (occasional rash),
Obviously very please. Two failures were in patients with IVDA, disseminated MRSA infection (multiple sites) and septic shock. Not sure I can b”blame” even those 2 on antibiotic failure – more likely MSOF.
Just an FYI
What about the combination of Vancomycin and Ceftaroline??
pls what are the best combination therapy for MRSA Bacteremia . i just need the drugs listed. thank u
Patrick