An ongoing dialogue on HIV/AIDS, infectious diseases,
June 9th, 2024
The Mysteries and Challenges of the RPR — and a Proposed Clinical Trial
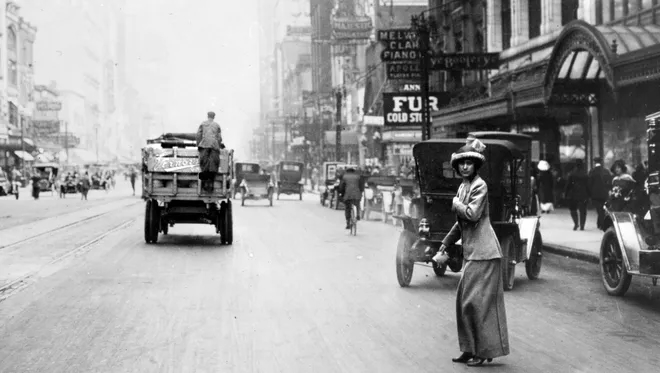
Detroit, early 20th century. RPRs are the Karius of the day.
Last week, we had a real treat for our weekly ID/HIV clinical conference — a review of controversies in the management of syphilis in adults by Dr. Khalil Ghanem, from Johns Hopkins. He’s a well-known expert in the field of sexually transmitted infections, syphilis in particular.
A highlight of the talk was his dismantling of a particularly confusing aspect of treatment monitoring, which is the serial checking of the RPR to assess the response to treatment, along with retreatment for failure to respond. An abbreviation for rapid plasma reagin, the RPR and its oscillations have vexed clinicians and their patients for decades.
How long? Well, since 1906 — 118 years ago, if his talk (and my math) are correct. To highlight how long ago this was, he showed a slide depicting what people were driving and wearing in 1906. (See photo for approximation. His slide is much funnier.) This is emphatically not a new technology. Don’t expect a high degree of accuracy from something that debuted before widespread electrification of homes in our country.
And the test is very weird. Unlike most antibody tests in infectious diseases, it measures not antibodies directed against the pathogen of interest, Treponema pallidum, but to cardiolipin-cholesterol-lecithin antigens; it’s an immunologic response triggered by the infection.
These antibodies are called “reaginic” antibodies — whatever “reaginic” means. Not surprisingly, the RPR is the quintessential non-specific diagnostic test, with tons of false positives (11% in one study), and a very well-known (and paradoxical) cause of false-negatives when the titer is particularly high, called the “prozone” phenomenon.
Which, trust me, isn’t a zone you want to be in.
To make matters more confusing, how about those units? Here’s a summary I wrote previously trying to explain how RPRs are reported, and what they mean:
When positive, RPRs are reported in dilutions — e.g., 1:4 is a one-dilution lower (and a twofold lower) titer than 1:8. Not many of our tests get reported this way (ANA comes to mind as another); in general, it’s only considered a significant change if it’s two dilutions or more — 1:16 goes down to 1:4 after treatment, for example.
So what about this fourfold change? As summarized by Dr. Ghanem, the data supporting this notion that this change is necessary for treatment success are weak indeed — in fact, the primary argument for it is that laboratory variability is a twofold change, hence you can’t say anything significant about a titer that goes from 1:16 to 1:8.
How about the view that if the titer doesn’t drop appropriately, then the patient should at the very least be retreated, with consideration of a CSF examination to diagnose occult CNS disease? Again, data are very weak to support these recommendations, even though I’ve heard some experts strongly advocate this approach.
In summary, we can legitimately question a strategy of retreatment of syphilis for “serologic non-response”. Even the STI treatment guidelines acknowledge this uncertainty.
Failure of nontreponemal test titers to decrease fourfold within 12 months after therapy for primary or secondary syphilis (inadequate serologic response) might be indicative of treatment failure … Optimal management of persons who have an inadequate serologic response after syphilis treatment is unclear.
Sounds like the perfect setting for a clinical trial. Indeed, during the question-and-answer period, Dr. Ghanem commented that he’d like to see such a study of syphilis serologic non-response with and without further treatment.
Inspired by his talk, I offer here a potential study design:
– Inclusion criteria: Asymptomatic people with treated syphilis who have serologic non-response, defined as a failure of nontreponemal test titers to decrease fourfold within 12 months after therapy
– Stratifications: Stage of disease (early vs late), HIV
– Exclusion criteria: Suspected reinfection, pregnancy, non-penicillin therapy
– Intervention: Randomization to 1) retreatment with penicillin or, 2) ongoing clinical monitoring alone, with assumption that the titer is the patient’s new baseline
– Primary endpoint: Clinical manifestations of treatment failure
– Secondary endpoints: RPR trajectory, other blood tests, additional testing (such as CSF exams), other treatments, patient satisfaction score, clinician time, costs
Would you refer a patient who meets these criteria into such a study? Anyone interested in doing it? Seems right up the alley of the great pragmatic trials run by our ID and sexual health colleagues in the United Kingdom — hope they (or someone else) will give it some thought.
And though it has nothing to do with syphilis, this UK export certainly makes me laugh every time I watch it.
(Thanks to Dr. Ghanem for sharing his expertise, and for input on this post. You can watch a version of his talk at this year’s CROI.)


Very interesting and thought provoking. Newer studies will certianly improve our understanding and are welcome. However, following observations deem considerarion:
Yes, RPR is non specific test, detects the antibodies formed against body tissue (not treponema). Its rising and falling titers indicate progressive or regressive tissue damage. It could happen due to a variety of causes like infectious, autoimmune etc). The minimum level of four fold change in titer is considered significant to overcome interlaboratory and intra llaboratory variations. All acceptable.
The strength of this test though old, is that it has stood the test of time. Like interpretation of any other test, it has to take clinical and other parameters into consideration. Is the same criteria not applied for other tests like raised CRP, total and differential leucocyte counts, titers of antibodies, enzyme levels, TNF level etc for variety of conditions?
RPR is still a good monitor of progression of chronic tissue damage (due to syphilis or otherwise) in the hands and minds of discerning clinician.
The specific tests of treponemal antibodies have not been able to help in monitoring progression of the disease Syphilis. (These tests indicate only past infections, even when treated and person is non infectious).
Let’s rethink. What are we worried about? Treatment of treponemal infection or Syphilis the disease? If it is to monitor disease, RPR still is useful. If it is to determine past treated or untreated infections (or even existing infections) only, specific tests are our choice. These could be good for epidemiological studies but not suiatble for monitoring progression of Syphilis, the result of infection.
RPR tests will still be useful till we develop better and more sensitive methods of monitoring the Syphilis.
Another insightful piece to start my Monday morning- thank you Paul. One thing not mentioned is explaining the RPR titers to our patients which is often quite challenging. Really hope that someone takes the lead with your trial design or better yet is there possibly a better test that could be developed?
I have always been fascinated by syphilis, its protean manifestations, diagnostic challenges, the need or not for CSF examinations, the interpretation of lab data, etc.. Wasn’t it Osler who called syphilis “the great imitator” and also said “to know syphilis is to know medicine”?
Then came “to know HIV/AIDS is to know medicine.” Don’t know who said that, but I heard it somewhere.
Well, maybe both are exaggerations, but you do learn quite a bit while caring patients with these two infections.
And I like the study proposal!
I’d refer a patient who is “serofast” to this proposed trial, but likely first would want a try at re-treating. Would that make them ineligible?
Excluding reinfection also VERY difficult in some people.
If I were designing the study, I’d exclude people who had already been re-treated. But that’s an idea for a second study!
-Paul
The post highlights the longstanding challenges and controversies in monitoring syphilis treatment using the Rapid Plasma Reagin (RPR) test. Given the limitations and inconsistencies associated with the RPR test, an alternative approach could be considered.
What about using syphilis PCR testing instead of RPR? Syphilis PCR has the potential to provide a more accurate and sensitive method for detecting active Treponema pallidum infections. Unlike RPR, which measures non-specific antibodies, PCR can directly detect the presence of the bacterial DNA, thereby confirming active infection. This direct detection could help differentiate between treatment responders and non-responders more effectively.
While the cost-effectiveness of syphilis PCR needs further evaluation, its higher sensitivity and specificity could make it a superior option for treatment monitoring. Has anyone had experience using syphilis PCR on serum samples or other specimen types? If the sensitivity and specificity are indeed high, why not consider a study comparing syphilis PCR with RPR, potentially replacing the latter in clinical practice?
This approach could align well with the clinical trial design suggested in the post, focusing on treatment responses and monitoring strategies for syphilis. A study comparing the efficacy of syphilis PCR versus RPR in treatment monitoring could provide valuable insights and potentially improve clinical outcomes for patients.
I love practical studies! The ACORN study is a great example of what you *could* do if you truly have no standard of care and true clinical equipoise. Enrollment would not be that challenging, especially if the outcome was serological titer and not a mushy and hard to standardize across sites ‘clinical outcome’.
Now do “when to order an HIV genotype.” At 200? 400? 500? 1,000? Once off or repeated elevation? How much clinical suspicion do you need that it isn’t non-adherence? What if you could confirm adherence with Tenofovir levels?
Scientifically, this proposed clinical trial makes a lot of sense and would contribute a lot to the optimal care of patients with syphilis.
Politically? Not so much… I’m a white doctor working in a primarily African American community. I’ve spent the last 10 years gradually building trust and credibility in my community. The moment word got out that I was recruiting patients for a government-funded syphilis study where patients may or may not receive what’s currently considered the community standard for treatment and may just get a placebo and be monitored clinically while they could continue to develop complications and spread the infection… I could talk about clinical equipoise until I was blue in the face, but my credibility in my community would be totally shot.
To be clear, I’m not saying at all that I think there’s anything unethical about this study design! But at least where I work, the perception would be terrible. I think this proposed study definitely has merit and should be considered, but probably in a different country with a different history and a different set of cultural memories.
I think first we need to fix the name RPR colloquially ‘non treponemal’ which is not totally true. Second, no matter how we view this test in terms of technology, test characteristics etc., it’s doing the job. In my view, RPR will not go anywhere soon unless we find another proteins or metabolite which will do the same and then we can can adopt that protein or metabolite/s to a fancier platform with a much bigger wallet (those who have!).
The problem with this study is finding people who were treated with penicillin. We still can’t get our hands on Bicillin. Going on two years of having to use doxy first line and hoping people will complete 2-4 weeks of it.
Increased incidence -> Increased demand -> decreased supply -> increased doxycycline use -> decreased completion of tx -> increased incidence
I bet annually screening suffices, or we may just take one-month doxyPrEP every winter vacation.