An ongoing dialogue on HIV/AIDS, infectious diseases,
July 5th, 2020
Rapid, Inexpensive Home Testing for COVID-19 May Get Us Out of This Mess Before a Vaccine
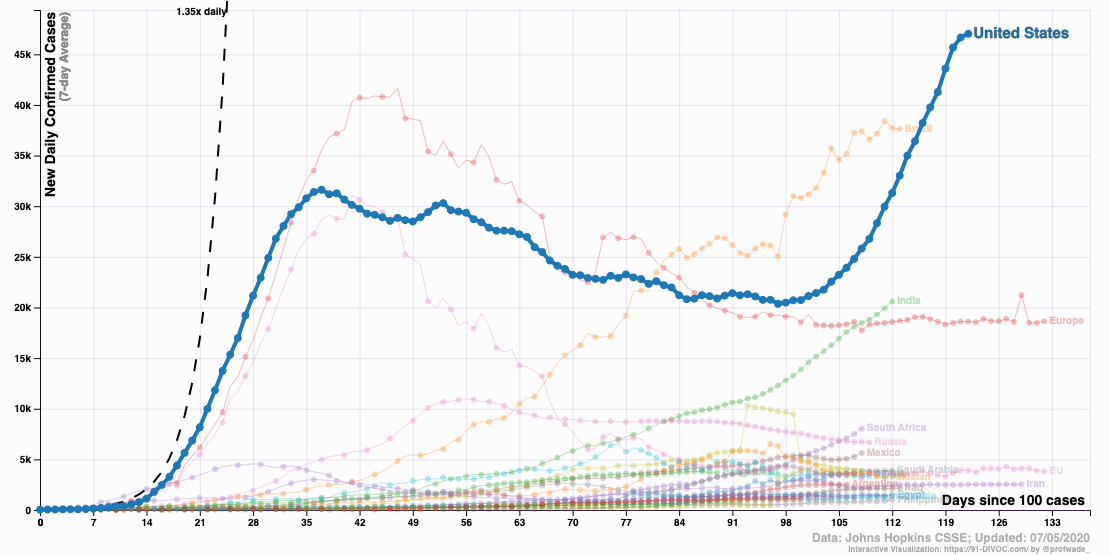
As cases of COVID-19 continue to climb to record numbers, it might seem impossible that something is already out there that could dramatically reduce new infections — and even bring us back to some semblance of normal life.
I’m not referring to a vaccine. It’s a rapid, inexpensive home test.
You’re forgiven for being incredulous. Indeed, you might be discouraged by a depressing sense of deja vu as you hear that hard-hit communities again must suffer delays on both obtaining tests and getting results.
And it’s not just Arizona, Texas, and Florida. Testing volume for COVID-19 has so overwhelmed commercial and national reference labs that turnaround times to get results are at the very least several days, and can be a week or longer — tests ordered from anywhere in the country.
Didn’t we learn anything from our lack of tests in the winter and spring, when contagious cases went undetected because of our inability to test all but symptomatic people? Didn’t that allow those with mild or pre-symptomatic disease to continue to spread the virus in the community, triggering an explosive increase in cases?
The problem is that we’re doing it all wrong. Again.
We need to test more broadly, even in people without symptoms. The critical window period for transmitting the virus starts a day before symptom onset.
And instead of relying on the gold standard for diagnosis — the polymerase chain reaction (PCR) tests, done on a nasopharyngeal swab — we need to lower the bar for accuracy and use one of the many rapid tests currently in development.
As noted in this spot-on perspective on rapid home tests written by Drs. Laurence Kotlikoff and Michael Mina, our PCR testing, while accurate, has many problems — it’s expensive, it’s slow, and it strains the lab supply chain. Our hospital has had to diversify the PCR tests it offers to at least 5 different platforms to avoid running low on any one particular test.
Some might argue PCR is too sensitive — it picks up fragments of viral RNA long after a patient is no longer contagious. These positive results generate all kinds of confusion and worry.
In addition, a nasopharyngeal swab requires trained personnel to obtain the sample. It hurts, too, as anyone who has had the test will tell you. There’s a reason the most common “joke” heard after undergoing PCR testing is likening it to a pituitary biopsy. Ha ha.
So why don’t we have rapid, cheap home tests available now?
It’s not for lack of trying — take a look at this list of companies working on the problem as of early June:
Thanks, Tomas
That makes 16 pic.twitter.com/QQcBDopaGL— Eric Topol (@EricTopol) June 7, 2020
Apparently, one thing that may be holding up FDA approval of these tests is that they are less sensitive than the PCR. That means they’re more likely than the PCR to miss someone who has COVID-19, wrongly giving a sense of reassurance from a false-negative result.
This is a legitimate concern, but one that should not block their urgent approval anyway. We should welcome these tests, even if less accurate, and broadly adopt them for widespread community use. Here’s why:
- They will be cheap. Estimates are that they would cost between 1 and 5 dollars. That’s around the price of a cup of coffee.
- They can be done on saliva. No brain biopsy required.
- They can be done frequently. Every day for college students, or healthcare workers, or bus drivers? Every third day for everyone?
- They will answer the key question — am I contagious to others right now?
Finally, and most importantly, they will answer this last question quickly. Results back in less than an hour.
Anyone with a positive test can self-isolate, be reported to public health officials, participate in a contact tracing program, and be monitored for symptoms. Maybe pre-emptive antiviral therapy will prevent severe illness.
We can choose to do a rapid home test any day we go to work, or to the gym, or to meet friends in a restaurant, or to attend a concert, or to pray in a house of worship, or to visit an elder loved one, or indeed partake in any activity we do in groups that now sadly may sustain the pandemic.
And for those worried about lack of sensitivity, two items of reassurance. First, false negatives are less likely when people have the highest amounts of virus in saliva and respiratory secretions — and this is when they’re most contagious to others. If the test is falsely negative due to low titers of virus, it may not matter very much.
Second, this modeling study finds that the frequency of testing is the key determinant of how well a broad testing strategy will limit the spread of the virus. It’s even more important than test sensitivity, and evidence that imperfect testing is better than no testing at all.
So bring on the rapid home tests — lower sensitivity notwithstanding — and the sooner, the better.
It’s one thing that could make Olive and Mabel’s retirement easier to take. Maybe they’ll even do a reunion tour.
Categories: Health Care
Tags: COVID-19, rapid home COVID testing, rapid viral diagnostics
You can follow any responses to this entry through the RSS 2.0 feed. Both comments and pings are currently closed.
72 Responses to “Rapid, Inexpensive Home Testing for COVID-19 May Get Us Out of This Mess Before a Vaccine”

Paul E. Sax, MD
Contributing Editor
NEJM Journal Watch
Infectious Diseases
Biography | Disclosures | Summaries
Learn more about HIV and ID Observations.
Follow HIV and ID Observations Posts via Email
- Federal HIV Guidelines Face a Shutdown — A Critical Loss for Clinicians and Patients
- The Mystery of the Isolated Hepatitis B Core Antibody, Solved
- Why the Sudden Firing of ACIP Members Should Put Every Clinician on High Alert
- How ID Doctors Get Paid, Part 2: Infection Control and Other Invaluable (but Often Invisible) Work
- How ID Doctors Get Paid, Part 3: The Grab Bag Edition
- ID Cartoon Caption Contest (125)
- ID Cartoon Caption Contest #2 Winner — and a New Contest for the Holidays (92)
- Dear Nation — A Series of Apologies on COVID-19 (80)
- How to Induce Rage in a Doctor (77)
- IDSA’s COVID-19 Treatment Guidelines Highlight Difficulty of “Don’t Just Do Something, Stand There” (74)
-
 NEJM Journal Watch — Recent Infectious Disease Articles
NEJM Journal Watch — Recent Infectious Disease Articles- Diphtheria Outbreak in the EU: Reason for Concern
- First-Line Therapy for C. difficile Colitis: Does Fecal Microbiota Transplantation Have a Role?
- Observations from ID and Beyond: The Mystery of the Isolated Hepatitis B Core Antibody, Solved
- Observations from ID and Beyond: Federal HIV Guidelines Face a Shutdown — A Critical Loss for Clinicians and Patients
- Ceftriaxone for Patients Hospitalized with Pneumonia: One Gram or Two?
-
Tag Cloud
- Abacavir AIDS antibiotics antiretroviral therapy ART atazanavir baseball Brush with Greatness CDC C diff COVID-19 CROI darunavir dolutegravir elvitegravir etravirine FDA HCV hepatitis C HIV HIV cure HIV testing ID fellowship ID Learning Unit Infectious Diseases influenza Link-o-Rama lyme disease MRSA PEP Policy PrEP prevention primary care raltegravir Really Rapid Review resistance Retrovirus Conference rilpivirine sofosbuvir TDF/FTC tenofovir Thanksgiving vaccines zoster

My sister has been thinking about testing for COVID 19 because she was just at a family reunion with a lot of people that weren’t very careful. She would really like to get some help from a professional so that she can make sure that she is safe and can protect others around her. Thanks for pointing out how symptoms can be shown and catching it right before they are could be really useful and testing people without symptoms could help them be safer. http://curevoya.com/covid19-response
We work in a molecular biology laboratory in the interior of Brazil and have the capacity to perform up to 1000 RT PCR tests for Sars Cov 2 at a cost of $ 40 per exam. Our proposal would be to do the group tests on asymptomatic people using saliva, managing to reduce the value of the test per person to 8 dollars and we could perform tests on up to 10,000 people per day. This without significantly reducing the sensitivity of the test.
I propose (worth discussing and thinking about it) a quick, inexpensive ligation- Loop-mediated isothermal amplification (LIGLAMP) method to diagnose COVID-19 without the need for RNA extraction, Reverse transcription and any device. If this method is possible, not only in health centers with low facilities but also in public places and at home, it will easily be possible to test each person in less than an hour with saliva or nasal samples. The following three steps are proposed for this method in the three serial microtubes:
1- releasing the RNA of the virus using a gentle treatment of a detergent such as Triton (or a lipase?) from saliva samples.
2- ligation Two-oligonucleotide fragment complement to a part of the virus genome using T4 ligase in the presence of RNA of the virus.
3- LAMP amplification and turbidity checking or adding a dye such as safe stain that allows amplification detection without the need to transilluminator, simply in the light of a cell phone.
Of course, this is a preliminary proposal and can be discussed and optimized. The first step is critical, how can release intact RNA and allow ligase to work in the next step? What is the optimal detergent concentration?
All tubes with contents can be lyophilized and only salivary or/and nasal fluid will be sufficient. Production in large quantities can lead to lower prices, and its transportation does not require a cold chain and can be stored for a long time in any environment. At the end of the work, all microtubes can be washed with any household detergent to prevent contamination.
Dr. Jalal Rostamzadeh
Dr. Rostamzadeh – I was intrigued by your suggestion of using LAMP amplification for inexpensive and frequent SARS COV-2 testing – and potential to do this at home. I am researching companies that are building technologies for exactly this – high frequency home based quick testing. Do you know of folks who are currently in production of these approaches?
Thanks!
Ben – It was an idea and no company produces it. It was presented for discussion.
Dear Dr Paul
Thanks for your paper.
What is your opinion about fecal PCR tests, in terms of sensibility ans specifity?
Paul – I have been reading Michael Mina’s work on this issue. I completely agree re: frequent, low cost and rapid testing could lead to greater confidence for people to get back to school and work – with at least less worry about becoming infected.
Is there a good resource in terms of continual updates on companies / labs who are developing different solutions in this space? Also it might be an opportunity for proof of concept – meaning grassroots applications (e.g., a school, company or university) who shows some success with this approach to build momentum more broadly.
I’m looking to learn more and get involved!
Thanks,
Ben
Is there anything actionable that a private citizen with a a small network of contacts can do to put pressure on anyone anywhere that might help this along? It’s not clear who are the players or where are the bottlenecks that have been identified, other than the general thought that it is slowed by the idea that the tests are not as accurate as the gold standards (but apparently accurate enough to deal with the real problem of infectiousness.) Anyone have actionable info that can focus pressure somewhere useful from private citizens?
To get involved in a grassroots effort, advised by Dr. Mina and Professor Larremore (author of the cited modeling study), visit https://rapidtests.org; the site also has prepared sample letters to representatives and a quick way to review them and have them emailed to all your representatives in congress and your governor, in a couple minutes.
There is also an associated group on Facebook that has 1100 members after just four days, and is carrying on active discussions and spreading the word.
Rapid inexpensive home COVID-19 tests and SARS-CoV-2 antibody tests are critically important because they will allow people to understand their health condition related to COVID-19. They provide opportunities for people using contact tracking programs for showing they are either not currently infected or have immunity because they have SARS-CoV-2 antibodies.
For home infection tests, when people know if they are infected, they can get treatment earlier.
For home antibody tests, one of the reasons people are using contract tracking programs is their concerns about privacy. When people can perform those tests at home, they can maintain the maximum protection for privacy by saving the test results in their cell phones and requiring their authorization for accessing the test results.
From the above article:
“That means they’re more likely than the PCR to **miss someone who has COVID-19,** wrongly giving a sense of reassurance from a false-negative result.”
This is a mistake, or a misunderstanding of the test. The goal of the lateral flow test is NOT to find people who HAVE COVID-19, but those who are INFECTIVE. For this goal, the test is extremely effective – it’s important to understand that this particular criticism of the test reflects lack of understanding of the purpose of the test and is a stumbling block to the FDA in giving permission for its release.
Critical is the proportion of wrong results and the prediction power of the results (both npv and ppv). Any screening tests having less than 100% specificity will inadvertently lead to enormous follow-up efforts to sort out. This means that the strategy is at least as important as the analytics, if not even more so for early diagnostics i.e. in areas of low prevalence and unsymptomatic populations. In contrast to NA tests, no protein-detecting assay has that 100% specificity.
In antigen testing using home test formats and LFAs, the preanalytical aspects also are important, because they detemine the diagnostic (not the analytical) sensitivities. I know of no study having systematically compared the sensitivity of self-testing (gargle etc.) vs. profession swab testing leaving the false negative rate unaccounted for.
In my opinion, the limitations to screening test in an pandemic can only be mitigated using strategies for repeatedly testing the cohorts several times within two weeks. That would require a very high discipline in the population, something that will not be achievable without an political leadership effectively and beliebably communicating uncomfortable concepts.
Low cost rapid tests could be a useful strategy. But do you think that people who refuse to use mask would actually use these tests?