An ongoing dialogue on HIV/AIDS, infectious diseases,
April 7th, 2019
New York Times Highlights the Problem of Antimicrobial Resistance — and the Tricky Issue of Disclosure
Right there, on the homepage of today’s New York Times, our national paper of record — Sunday edition, no less! — appears this headline:
A Mysterious Infection, Spanning the Globe in a Climate of Secrecy
Most of this piece is about Candida auris, the highly resistant fungus that targets our most vulnerable patients — those with weakened immune systems due to extremes of age, comorbid medical problems, cancer chemotherapy, or immunosuppressive drugs.
The authors do an excellent job bringing attention to the seriousness of the problem. They provide some theories about its origin and cite the many challenges each Candida auris case brings to hospital workers, in particular those in charge of Infection Control.
But there’s a second message in this piece, one highlighted by the difference between the online headline and the one in print.
Online: A Mysterious Infection, Spanning the Globe in a Climate of Secrecy
Print: Fungus Immune to Drugs Quietly Sweeps the Globe
It’s that Climate of Secrecy phrase, implying there’s a widespread cover-up effort.
Indeed, there’s a distinct tone of blame in the article directed squarely at institutions that failed to disclose problems with Candida auris. One person quoted likened it to a restaurant failing to disclose that it had a food poisoning outbreak.
But with the caveat that I don’t work at the institutions cited in the article, I emphatically wish to state that we ID specialists strongly welcome all publicity about the seriousness of antimicrobial resistance.
In fact, if you want two messages about which we have 100% unanimity, here they are:
- Vaccines work, prevent illness, save lives, and save money — the risks are vastly outweighed by their many benefits.
- The overuse of antimicrobial agents leads to a dangerous increase in drug-resistant microorganisms, and this is a huge local, national, and global threat.
Read what Infection Control specialist Dr. Dan Diekema wrote after he saw the piece in the Times — he was “Happy to see” that this important issue had risen to such prominence:
Happy to see that an emerging, antimicrobial-resistant, healthcare-associated pathogen has made the FRONT PAGE of the NYT! The reporters do a good job placing C. auris in larger context..@PaulSaxMD @mike_edmond @eliowa 1/9 https://t.co/OH1ioEWJRT
— Dan Diekema (@dan_diekema) April 6, 2019
He (and all of us) are even happier that there’s another piece in the Times on antibiotic resistance, here describing how the combination of antibiotic overuse, crowding, and poor sanitation inexorably drives up resistance rates in low and middle income countries.
So, if there’s a cover-up about this important problem, it’s not coming from us ID doctors.
One last point — while I am all for transparency and disclosure if it improves patient safety, the public must realize that having patients with drug-resistant infections within the walls of a hospital by no means proves that these clinicians and Infection Control departments provide substandard care.
As noted above, it’s frequently the sickest, most complex, and vulnerable patients who develop these infections. Often they are transferred from other institutions after prolonged hospitalizations, with many weeks of antibiotic exposure before they even reach our inpatient wards, and they already harbor resistant bugs.
It would be a shame if tertiary-care hospitals viewed mandatory disclosures of resistant infections as a disincentive for providing care to these patients, who arguably need advanced care the most.
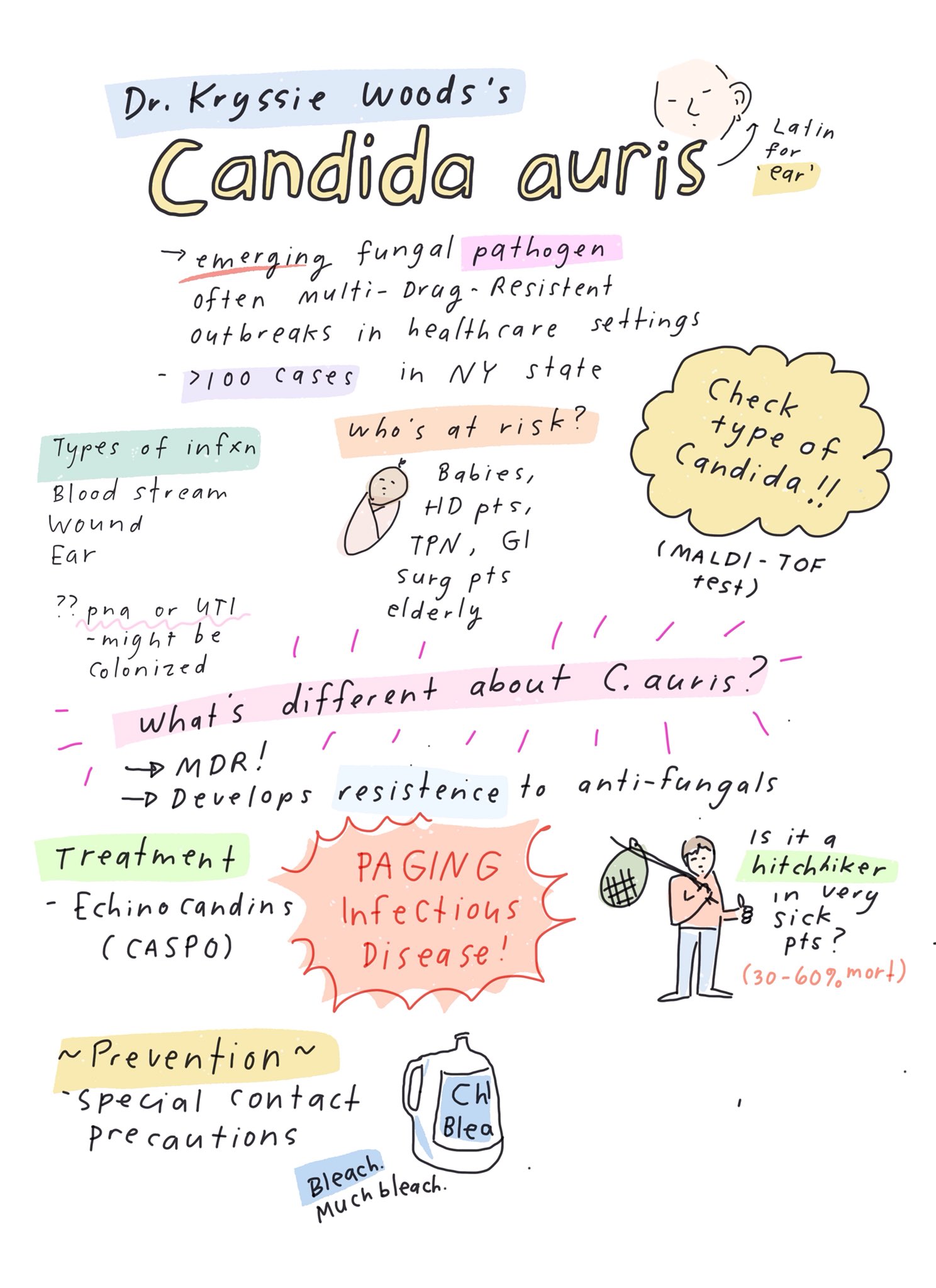
Meanwhile, here’s a wonderful summary of some key learning points about Candida auris — presciently sketched out by cartoonist-MD Dr. Grace Farris a couple of weeks before the Times piece was published. Thank you, Grace!


I read the article over the weekend and this quote stopped me cold: “…hospital workers used a special device to spray aerosolized hydrogen peroxide around a room used for a patient with C. auris, the theory being that the vapor would scour each nook and cranny. They left the device going for a week. Then they put a ‘settle plate’ in the middle of the room with a gel at the bottom that would serve as a place for any surviving microbes to grow, Dr. Rhodes said. Only one organism grew back. C. auris.”
Wow.
I was dismayed that the follow-up article you linked-to in your post propagated the common misconception that bacterial genes mutate (or “evolve”) in response to the presence of antibiotics: “Hard-wired to survive, many bacteria have evolved to outsmart the medications.” This is a point I emphasize to my students: Mutations are random. It is the “lucky” bacteria with the appropriate random mutation(s) that can survive and reproduce in the presence of the antibiotic we give our patients.
Just saw this new editorial in the NY Times: https://www.nytimes.com/2019/04/09/opinion/doctors-drug-resistant-infections.html The comments are enlightening as well.
One more nail in the coffin of public mistrust of medical institutions and physicians. Confusion and ignorance, stirred with media hype, provides fuel for public outrage.
Where are the voices of reason?