An ongoing dialogue on HIV/AIDS, infectious diseases,
June 20th, 2013
Let’s Move the HIV Testing Algorithm Into the 21st Century
As I’ve written before, the most widely used testing algorithm for HIV — enzyme immunoassay followed, if positive, by Western blot confirmation — is long overdue for an update.
A brief review why this is the case, and also why sticking with it is so problematic:
- Immunoassays have become progressively more sensitive, especially when paired with p24 antigen testing in “4th generation” tests.
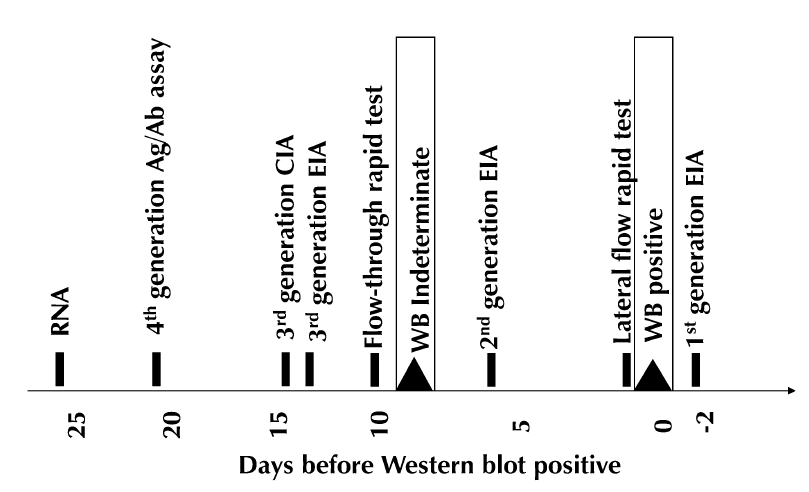
- In recently acquired infection, the screening test turns positive way before the Western blot — it can be a difference of several weeks (figure from Branson J Acquir Immune Defic Syndr 2010;55:S102–S105):
- Clinicians are not familiar with this problem, so they might conclude that a reactive screening test followed by a negative Western blot means that the person doesn’t have HIV — it’s a “confirmatory test”, after all, so you can understand their confusion.
- Patients during this phase of early/acute HIV infection are at their most contagious, hence most likely to spread the virus to others — especially if given the wrong information about their HIV status.
- Patients may seek testing soon after high-risk exposures — they’re motivated! — and hence are potentially in this window before the Western blot turns positive.
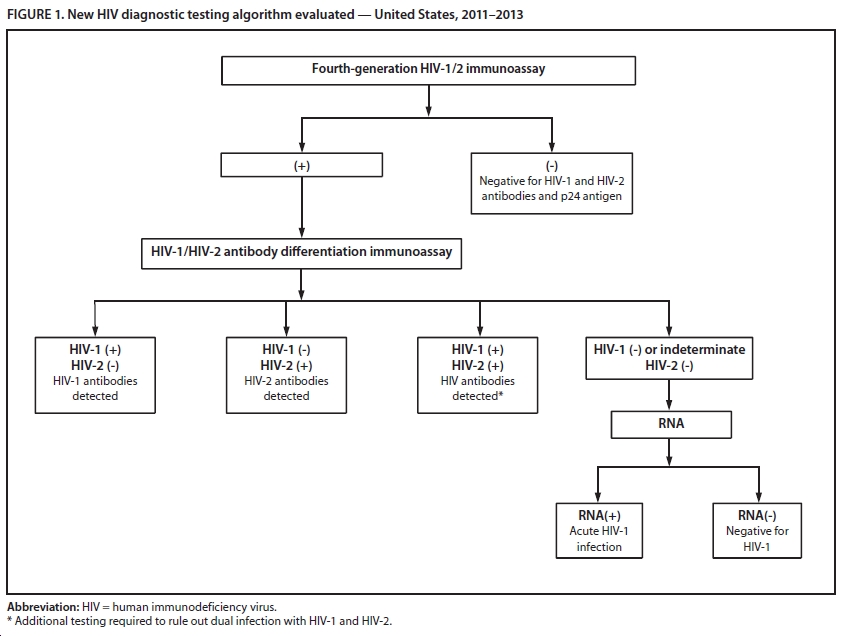
The frustrating thing about this state of affairs is that we have had the tools to correct this problem for some time. Laboratory guidelines for HIV testing were updated in 2011, recommending the following algorithm for HIV diagnosis:
Now, thanks to CDC, we have some concrete data about how useful this new testing strategy can be — in particular for those with recently acquired HIV. A screening program in an Arizona emergency department identified 37 individuals with undiagnosed with HIV, and twelve of them — nearly a third — had acute HIV that otherwise would have been missed by the Western blot.
A second validation study looked at over 37,000 samples drawn from high-risk patients in sites from New York City, North Carolina, and San Francisco; there were 99 cases where the screening immunoassay was positive and the second antibody test negative. In this group, 55 had acute HIV infection (diagnosed by HIV RNA), many of whom had negative Western blots.
According to Bernie Branson — HIV testing guru from CDC — the FDA approval of the differentiation assay (step 2 in the algorithm) has led many labs to adopt the new strategy:
The number of labs doing this has picked up considerably since Multispot received its new indication … nearly half of public health labs (e.g., FL, MA, IL, IA, NY) have adopted it, as have Stroger/Cook County in Chicago, Howard University Hospital in DC, and LSU hospital system (to name a few). California has proposed emergency regulations (expected to be effective July 2) that will permit all labs in the state to perform the new algorithm, which their current regulation precludes, and New York State has issued 2 public health advisories encouraging its use.
It’s time for the rest of us to do the same.
And if you’re feeling bad for the Western blot, it still has a (rare) indication — as a confirmation of HIV infection in “elite controllers”, those with HIV antibodies but no detectable HIV RNA.