An ongoing dialogue on HIV/AIDS, infectious diseases,
May 7th, 2009
Human Rabies from Bats: Another Look at the Numbers
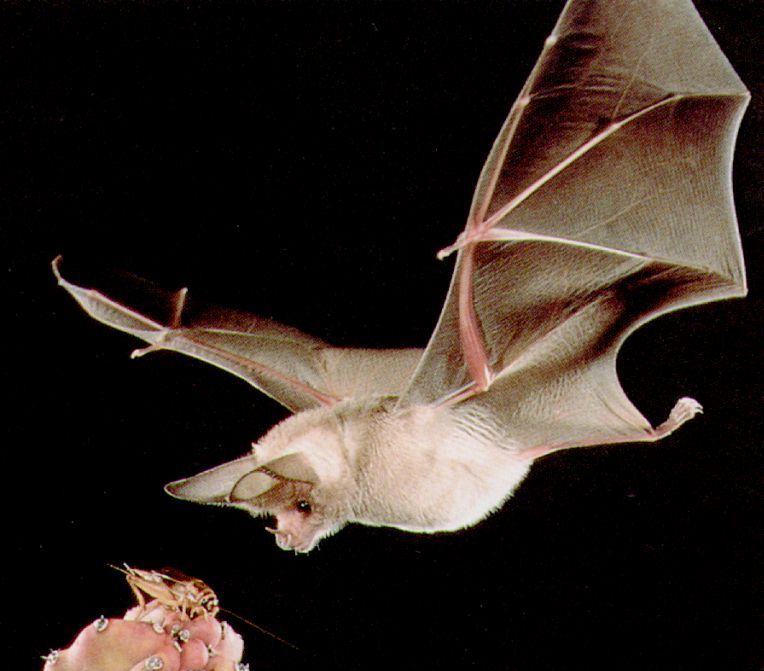 The gang from Canada is at it again, reviewing human rabies cases from bats and trying to make some sense of the data.
The gang from Canada is at it again, reviewing human rabies cases from bats and trying to make some sense of the data.
(For a summary of their outstanding prior paper in CID, read this.)
But before we get to their latest masterwork, here are some questions to ponder. While doing so, keep in mind the practice of giving the rabies vaccine to a person with “bedroom exposure to a bat while sleeping, without evidence of direct physical contact”:
- Are you more motivated by avoiding an “error of omission” (a mistake from not doing anything) than an “error of commission” (a mistake from doing something)?
- Do you ever envision yourself being named in a lawsuit for failure to provide preventive therapy?
- Do you sometimes imagine yourself cited in a newspaper as the doctor who said, “that isn’t necessary”, only then to have the patient in question be the one in a zillion who gets rabies? (“We called Dr. Freepner, and he said not to do it. Later, she was dead.”)
- Do you feel you have a moral imperative to provide preventive therapy for a condition that will likely be fatal, no matter how unlikely it is that a patient will develop it?
- Do you think cost, limited supply, and personnel issues should always be secondary considerations when making decisions about an individual?
- When you read official guidelines that state that preventive vaccination “can be considered” in low but not zero risk circumstances, do you interpret that to mean it should be given?
- Did you ever find yourself doing something clinically that you just knew made no sense, yet you did it anyway?
I suspect we all could answer “yes” to some, if not all, of the above questions. These are not rational decisions, they are emotional ones.
Hence this latest paper is such a joy to read. It provides yet more evidence that a policy of giving the rabies vaccine to patients with a “bedroom bat exposure” but no contact is, to be blunt, pretty ridiculous. Some of the key numbers:
- Based on a telephone survey done in Quebec, fewer than 5% of people with such bat exposure get vaccinated.
- The estimated incidence of rabies due to this exposure is 1 case per 2.7 billion person-years.
- The number needed to treat to prevent a single case of human rabies from bedroom exposure (but no contact) is around 2.7 million.
- If all potential exposures were investigated and evaluated fully — after all, this is recommended in the guidelines, right? — this would require 49 physicians, 491 nurses, and 259 veterinarians working full-time for a full-year. And this estimate does not even include administration of the rabies vaccine!
In short, what we are doing is absurd — we are giving preventive therapy to a small proportion of the potentially exposed only because they show up, and because we can. It has very little to do with preventing actual cases of rabies, but it sure makes us and our patients feel better.
But if it’s indicated for those who show up, what about the 95% who don’t? Solid quote:
Failure to intensely pursue a greater proportion of eligible persons then becomes paradoxical public policy: a recommendation that is known to be sustainable only if ignored by most eligible persons is of doubtful usefulness and questionable ethics.
So what are we to do? The authors conclude that the recommendations for rabies vaccine for bedroom or other occult exposures “be reconsidered.” I read that to mean, “be scrapped.”
And someone please point me in the direction of why some irrational physician behavior is so hard to shake.


Thank you for bringing this to our attention.
>>Thank you for bringing this to our attention.
You’re welcome. Next time you get called by a clinician wanting to know whether to give the vaccine for a bat in the bedroom, you can cite these numbers.
Dear sir, thanks. Dont you think is it possible swine flu transmitted by these kinds of vampire bats as vectors? As it was a report about of mysterious flu-like disease in bats several months ago.
First, I would point out that, given the extreme difficulty of diagnosing rabies infection, statistics regarding the frequency of human rabies fatalities certainly understate the reality, and may just be the tip of the iceberg.
Consider the large proportion of the US fatalities reported by the CDC where the victim languished in hospital undiagnosed, often for months, until after death. Then consider how many rabies deaths outside hospitals (and inside!) may have been ascribed to other causes, and never checked for rabies.
Secondly, I would point out that current preventative Rabies vaccination for humans (ie. pre-exposure) is not prohibitively expensive, and would become much less so, if there were a large, steady demand. Such vaccination should be strongly promoted for veterinary workers, hunters, and spelunkers, among others, especially since it appears now that a properly administered initial series confers lifetime immunity.
Thirdly, I would say that the suggested “take your chances” approach to Rabies infection relies on an “ignorance is bliss” attitude for acceptance. Most people, including physicians and even veterinarians, seem oblivious to the following stark realities:
1. once symptoms of rabies appear (and they may even then not be recognized as such), death is inevitable (and may be slow and gruesome)
2. The window of treatability shrinks dramatically as the site of infection nears the brain.
3. Rabies can be transmitted without any trauma to the patient via contact between infected saliva and mucous membranes or small cuts in the skin. Infection can result from touching an animal’s fur or muzzle, or even from inhaling the air in a cave frequented by infected bats (ie. in this disease, the “toilet seat” explanation DOES apply).
4. There is no sure way to rule out Rabies in a suspect animal without killing it and examining the brain.
5. Increasingly aggressive animal protection advocacy and laws make it more and more socially and legally hazardous to kill an animal on suspicion of Rabies. Some veterinarians are suggesting one should capture suspect bats alive, induce hibernation by refrigeration, and then place the animal under observation!
6. In Canada, where bats are the predominant Rabies reservoir, 90% of bats submitted for Rabies testing proved negative. Consequently, killing a bat on suspicion of Rabies (the only practical method of collection) incurs a serious risk of prosecution under animal cruelty legislation.
It follows from the combination of the above circumstances, that unreported human Rabies infections are sure to increase significantly in future, and with them, human Rabies mortality.
Encouraging physicians to “take a chance” with patients’ lives will certainly augment this mortality further.
I urge the reader to examine the annual Rabies mortality figures for Brazil, and consider whether the Brazilians are wisely conserving their medical resources.