An ongoing dialogue on HIV/AIDS, infectious diseases,
March 7th, 2022
How to Induce Rage in a Doctor
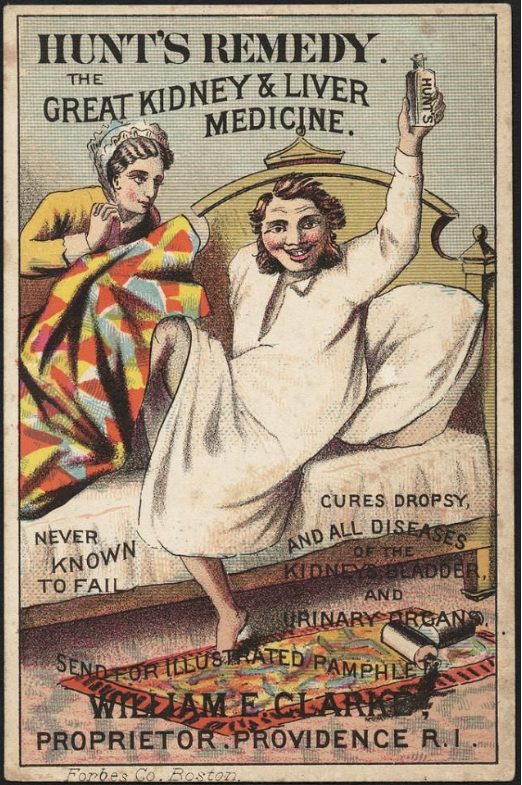
Advertisement for Hunt’s Remedy, which cured all diseases but did not require a prior authorization.
If you’re wondering how to make a doctor angry — really, really angry — read on. Because asking us to justify treatment decisions to insurance companies and their pharmacy benefit managers must rank right up there with the greatest tortures of practicing medicine in this country.
Mind you, this isn’t just about my patient, or about me — such infuriating events take place innumerable times in countless offices, hospitals, and clinics around the country every day, wasting everyone’s valuable time with no evidence whatsoever that they improve the quality of care.
Such struggles are an inevitable part of a healthcare system that values profits over people. The debates require a veritable army of staff on both sides to navigate what should often be very straightforward treatment issues.
Here’s a timeline of what happened. It’s Part 2 of the case presented a couple of weeks ago, which appeared with the patient’s permission (certain details changed).
February 6: Patient notifies me he needs a corticosteroid injection for back pain, which is contraindicated with his current HIV therapy due to a potentially serious drug interaction. We set up a video visit to discuss alternative HIV treatment options.
February 7: Televisit. I explain some treatment options, which I outline as bictegravir/TAF/FTC, dolutegravir/3TC, or doravirine plus TAF/FTC. He opts for the doravirine option based on side effects from previous treatments. Prescription sent to pharmacy.
I mention to him that doravirine sometimes requires a prior authorization. I also tell him that with his employer-provided insurance, it most likely will be fine. After all, the guy has a high-powered job in a very well known organization. He must have good coverage.
Furthermore, while HIV treatment remains quite expensive, none of the alternatives I’ve offered costs significantly more than what he’s currently receiving, and some cost less — at least based on the prices available to us.
Ha. Not so fast.
February 10: Message from patient that his pharmacy told him doravirine wasn’t covered. Needs a prior authorization.
I ask our pharmacy team, which consists of pharmacists and pharmacy techs hired for this express purpose, to help with it. They send it in, along with my office note from the televisit which justifies the reason for the treatment change.
February 14: I hear from the pharmacy team — prior authorization has been denied. Oh, and there’s this message:
Alternative Requested: PIFELTRO [doravirine] is NON-FORMULARY. MUST USE EFAVIRENZ, NEVIRAPINE, EDURANT. Call xxx-xxx-xxxx.
Well, this is a joyful Valentine’s Day present. They obviously don’t know his medical history, or much about HIV treatment. Why can I make this assumption?
- Efavirenz caused severe side effects years ago — he can’t take that.
- Nevirapine is not recommended in any treatment guidelines anymore, especially in people (like my patient) with high CD4 cell counts, as this increases the risk of severe hypersensitivity — he can’t take that.
- Edurant (rilpivirine) should not be given to people with low stomach acidity since it won’t be fully absorbed — he can’t take that.
I’ve always wondered — what if we followed these directives, and something truly terrible happened? After all, there are people who have died from nevirapine hypersensitivity, either from toxic epidermal necrolysis or fulminant liver failure or both.
Would the insurance company bear any of the blame, or legal risk? Would they care? I know the answer, sadly.
February 15: I call the phone number, which takes me to the pharmacy benefit manager. It’s the Giant-est of the Giants. How do annual revenues of more than 30 billion dollars sound? Pay for plenty of doravirine with that.
Phone tree. Then hold music. A warning about high call volume and long wait times. Then a person. Below a sampling of the dialogue.
Pharmacy Benefit Manager person #1: Hello, you’ve reached Brett. May I have the client’s member number?
Me: I don’t have it. I have his name and date of birth.
PBM person #1: OK, I’ll take that.
[pause while they look up the record]
PBM person #1: It says here the prior approval was denied. Pifeltro is non-formulary. You must use [pauses] EFAVIRENZ, NEVIRAPINE, EDURANT. [Difficulty reading the HIV drugs implies no knowledge of HIV medicine.]
Me: I know that — this is why I’m calling. But he can’t take any of those.
PBM Person #1: Do you want a clinician-to-clinician consultation?
Me: Yes. That’s why I called — this is the number we were given.
PBM Person #1: OK, let me transfer you.
[Hold music. Another warning about high call volumes and long wait times.]
PBM Person #2: Hello, you’ve reached Blake. May I have the client member #?
Me: I just gave that information to the previous person. Didn’t they pass that along to you?
PBM Person #2: Sorry, no.
Me: I have the name and date of birth, not the client #.
[Information given again.]
PBM Person #2: It says here that your prior approval was denied. You must use [pauses] EFAVIRENZ, NEVIRAPINE, EDURANT [more difficulty pronouncing the HIV drugs].
Me: That’s what the last person said to me, and I already know that. My patient can’t take any of these drugs. This is supposed to be a peer-to-peer consultation.
PBM Person #2: They sent you to the wrong number. I can forward.
[Hold music. Long hold.]
PBM Person #3: Hello, this is Bobby. May I have the patient’s name and client #?
Me: I only have the name and date of birth.
[Information given again. Third time, but who’s counting.]
PBM Person #3: I found the record. The Pifeltro was denied.
Me: Yes, Bobby, I know that, this is why I’m calling. Hoping you can help me. I’m an ID/HIV specialist in practice since 1992, and I’ve known this patient since 1996, including his full treatment history. The recommended alternatives are contraindicated — he can’t take any of them.
[Long pause.]
Me: Hello, do you need any further information?
PBM Person #3: I’m sorry, doctor, but I am not authorized to approve this drug.
Me [more than a little annoyed at this point — in fact here’s a good description of how I looked]: Why then am I speaking with you? This is the phone number I was advised to call. Are you a clinician? Do you have any knowledge of HIV treatment? Do you have access to the notes that were submitted for this claim?
PBM Person #3 [sounds like Bobby is now driving a car while speaking with me]: I’m sorry, Doctor. I am not authorized to approve this drug. If you want to appeal, or the patient wants to appeal, they will need to directly contact his insurance company with an appeal letter.
So why did all this happen? Why did Brett, Blake, and Bobby each fail to help my patient get his prescription covered?
It all starts with the relatively high cost of HIV treatment to begin with — a cost that has increased over 30% since 2012, a rate 3.5 times faster than inflation. Unlike most other industrialized countries, where government payers gather disease experts to review treatment options, then work with the pharmaceutical companies to arrive at a cost, such deliberations here are explicitly blocked and remain controversial.
With antiretroviral therapy so costly, insurance companies enlist the PBMs to negotiate what treatments get covered, what don’t, and how much they’re going to cost. It’s all done behind closed doors, in exchanges that one insider told me are “brutal.” As concisely (and accurately) stated in the opening to this recent perspective, “Prescription drug prices in the United States are opaque.”
The PBMs also sometimes direct where patients can most easily get their prescriptions filled (which may be the same companies, imagine that), and discourage dispensing of less expensive (but not negotiated) products.
If you think this clandestine process is ripe for distortion, obfuscation, and misuse of power, you’d be absolutely right. The lack of transparency means my patient and I have no way of finding out why doravirine isn’t covered — just that it isn’t.
But one thing I can state with 100% confidence — the refusal to cover my patient’s doravirine prescription has nothing whatsoever to do with improving the quality of his care, or following treatment guidelines, or really anything related to his health at all.
It was all about money. And that is sad indeed.
Hey, two more entries for the timeline:
February 25: Received information about the appeal process, and wrote the letter.
March 7: Still waiting …
(Thanks to brilliant colleagues Drs. Aaron Kesselheim and Ben Rome for reviewing this post. And to Dr. Glaukomflecken for making us laugh and cry at the same time.)


As a practicing ID physician, I’m impressed with your depth of knowledge but, even more so, with your willingness to undergo the “slings and arrows” of dealing with automaton PBM managers (are you sure the voice on the other end was human and not an enhanced AI system?)
There is, of course, another side to the coin. As a part time (med mal) reviewed I’m appalled at the profound ignorance, arrogance and just stupidity displayed my many of our fellow physicians. Treatments are routinely ordered based on, it seems, intensity of commercial promotion, vague ill-founded claims of superiority for some trivial feature (a purple pill rather than a white pill) or total disregard for drug interactions or long-term effects.
Handing drug management over to PBM managers is a poor choice. Sadly, giving physicians free rein of these decisions may not be much better.
Arnold Lentnek,
New York, NY
I am a Psychiatrist who sees patients of all ages. All of this is true, but much worse in Psychiatry. It’s not just incredibly expensive medication, it is anything that is not “dirt cheap” even if it is available as a generic formulation. No Viibryd, no Pristiq (even generic), can’t prescribe more than 1 capsule of Adderall XR (brand or generic) or dosage limits. Now dosage limits on all SSRIs and SNRIs even though there is plenty of evidence to document safety and efficacy. New absurd rules every week. The most recent one for a patient who needs 60 caps or tablet each month. Insurance will cover 30 or 104. Where did they get that number, they picked one that no one could possibly guess would be approved. This is the major factor in our current mental health crisis. I reached out to my politicians, local and national, and for the first time got no response from anyone. They all get a substantial contribution from insurance companies, regardless of party. We really need a union
The magnitude of this issue is huge. It effects all patients with chronic or serious Illness and those who care about them and take care of them. The resources drained from physicians and other team members must be staggering.
Thank you for the detailed description of the process that anyone can understand.
There have been times when I couldn’t get p.a., had no Rx so I sent pt to ER. This sometimes worked, but not applcable to this case. Try another neurosurgical consult for inpatient surgery, and have neurosurgeon Rx doravirine treatment as an alternative to expensive surgery.
Oh, this hit home. I had a week like that last week, only I was dealing with prior authorizations for multiple patients. An absolutely maddening experience, and a complete waste of time. The worst PBMs to deal with are the ones that are the gatekeepers for Medicaid plans. They put up barrier after barrier, including requiring PAs for common, cheap generic medications. And then requiring a new PA every time the dose is changed. And requiring a renewal of the PA in 1 year, with the same level of documentation the original PA required. I could go on… And that is IF they approve the medication and don’t deny it, forcing me to write an appeal letter.
I had a surreal moment with one of the PBMs. After giving my NPI number, the patient’s name and DOB, etc. to the lovely AI voice, it asked me to hold. “Calls may be recorded for quality assurance”. I muttered under my breath, “Oh, yes, I bet it’s for quality assurance”. At that point the AI voice said, “I’m sorry. I did not catch that. Could you repeat it?”. I tried just being silent at that point, but AI was having none of it. “I’m sorry….” etc. Then the voice started giving me a menu of choices for things I could do. The same menu I had just gone through. I didn’t know whether to laugh or cry, so I chose to laugh at the absolute absurdity of the situation.
I just spent a week working in Panama. They have a far from perfect medical system but interestingly HIV patients meds are covered 100%.
Just an interesting Comparison.
It sounds like the bad old days decades ago, when antiretroviral meds were relatively new, and, as a family doctor working at a community health center, I was put on a committee to help advise (i.e., rubber stamp) this state’s new private Medicaid management companies’ formulary decisions. I pointed out that most of the first-line HIV meds were not included on their formulary. They said that was fine, because they did include 2 antiretrovirals. They seemed completely surprised when I told them that most patients with HIV needed to take combinations of 3 antiretroviral drugs together at the same time, and needed additional alternative meds available to switch to, in case all too common drug resistance or intolerable side effects developed. They decided they no longer needed me on the committee.
Prior authorization = rationing by inconvenience. This is unacceptable. Time to rebuild this crazy non-system. At the very least, capture all those EHR data that explain why he can’t take the recommended meds. He’s lucky to have you as his doc!
Just read this Medscape article this morning: https://www.medscape.com/viewarticle/968834
PBMs are described by one doctor as “a parasitic infection to our healthcare system.”
Very frustrating indeed. However, there is a simple workaround if your hospital system wants to play ball (most hospital systems don’t, though). There is legal precedent that PAs, by themselves, serve no particular purpose, as described in the Gibson vs. Medco case a number of years ago (brought by a physician who felt the uselessness of these dumb PAs) and only serve to obstruct care. I have my staff fax the legal decision of the case, along with a form the insurance company can fill out and send along with a $99 payment if they want me to do a PA. We have no legal obligation to do PAs nor do we get paid for them. Haven’t had to do one in a while. One could argue urgency of patient care may take precedent, which occasionally but rarely may be the case.
The basic form I use is here, I just copied, pasted, and personalized: https://www.scribd.com/doc/297534113/Prior-Authorization-Consult-Request-Form
Hello Ben,
I would love to use the approach you described here! It sounds so Empowering! (Sweet revenge, really,)
In order for me to read the link you attached here, I’d have to subscribe to scrib, which I prefer not to do (it costs $9.99/month). Is there a way for you to share the attachment without joining scrib?
–Rick Pitch, MD
thank you for enlightening those who were not aware of the problem.
I had this same thing happen, also for an urgent steroid injection in someone on a boosted régimen with some prior 2 class resistance. Couldn’t get fostemsavir unless 4 class failure and no DOR. Not sure why people have to have 4 class failure to use a drug that needs optimized backbone or if DDI or comorbidities are an issue. But only allowed to comment if drug resistance, no place on insurance forms for other rationale. Can’t talk to a real person…
And the poor guy who needed to switch for a backache over a month ago? Is he in a wheelchair yet? Or addicted to painkillers? 🙁
Another frustration is not even realizing when you might be hit with the prior auth- so many insurance companies all with their own rules makes it impossible to keep track. So if you need an urgent change and then the patient can’t fill a medicine it creates a HUGE problem. An URGENT prior auth process or appeal is still in the 72 hour time bracket for the insurance companies. Also it can be an issue if you got a prior auth for a medication but annually they make you prove again why this is needed. That can catch you unawares as well and lead to lag in getting refills. It is such an insane and broken system.
Our pharmacy team at the HIV clinic where I work handles a number of both PA issues and peer-to-peer appeals. When I call on these, some of the phone reps try to steer me towards only using an appeal form rather than a peer-to-peer interaction. Typically I either push back hard or just call back, talk to another rep, and bluntly ask for a peer-to-peer to appeal the denial. The second call was a charm last week on a similar issue with a denial for a heavily treatment experienced patient. The most frustrating part is getting to the right place through a confusing phone tree.
Hello Doc
I feel your pain…
It is very frustrating but why are you surprised? I am willing to bet you strongly support something akin to Medicare-for-all. If its not a profit-hungry private entity intruding into the relationship, just wait until the heartless federal bureaucrats are FULLY embedded in the process. We turned this over to the low-spinal-response-based, algorithm-driven Bret-Blake-Bobby types a long time ago. We reap what we sow.
M Lacy
I call is Prior Authorization Fatigue Syndrome (PAFS). I recently reported a similar situation at KevinMD.com.
https://www.kevinmd.com/2021/11/how-prior-authorization-fatigue-syndrome-impedes-asthma-care.html
An hour on the phone with long term care pharmacy Ex S just tog get back where started. The trauma stated with me for days or PAST (Prior Authorization Stress Disorder) –
The fact there are so many comments illustrates the magnitude of the problem – thanks for sharing
The worst is when the ER only provides 1 day of meds and tells the patient to contact their physician for additional doses which require a STAT prior auth! It is an impossible task and you don’t even have time on your schedule to create a billable visit. The system is pushing us off the precipice!
Not surprising.
I have often asked physicians working for insurance companies why they made that choice, being an existentialist. Some admit to making a deal with Lucifer for the reward of supra clinical income while working in the proverbial PJs. Well, at least they admit that their brand of solipsism is an ethical compromise. Others censure the patient’s choice of insurers. Yet others are merely following a script and are as cognitively perspicacious as our “leaders” in D.C. The fantasy of a “Wonderful World” will only be attainable on an old Disney ride.
Hoo-eee! Where’d you learn all them fancy words? La-di-da, la-di-da.
Part of the problem, of course, is that pharmaceutical companies charge Way more for drugs here in America, than are charged in other countries. We developed many of the drugs in this country, but still, it’s too much. They heavily advertise on television, wine and dine us doctors, etc. Much of the research was government-funded anyhow.
Democratic and Republican administrations have both promised action on this issue, but it does not seem to be forthcoming.
Think about cost managers err, I mean case managers. I would try organizing a system where the PA’s get sent to your CM. The CM comes to your office daily or periodically to handle these. The patient needs to pay their fee, about $35/hr. You do nothing but give them your cases. The patient has to pay them by credit card in advance. You make nothing on this, so you do not appear money motivated to the patient. You are now freed from “free” administrative burdens. This is the very kind of things Cost, I mean Case Managers are set up to do.
This could not have happened without the collaboration of physicians and medical institutions and organizations that have essentially compromised their ethical obligations due to financial or political reasons.
I’ve had countless days filled with wasted minutes/hours dedicated to futile prior authorization conversations with PBMs. I did find a fast loophole for a few appropriate patients/situations, and that is asking them to forward me to an emergency use authorization provider. I.e. In the case of patients with uncontrolled diabetes who are unable to take regular oral medications due to renal issues or side effects and precluded from insulin due to recurrent hypoglycemic episodes obviously are going to need some thing quickly and any delay could cause serious repercussions; this is one of those items where a clinician can circumvent regular due process. If you tell them that your patients health and well-being are being ‘seriously impacted by the wait imposed by the insurance protocol’, and that they ‘require immediate intervention’, this emergency need can get many crucial drugs approved right away. I’ve done this and it is a godsend. Clearly you can’t abuse this loophole… especially for things like ADHD medication’s lol. But for legitimately time sensitive situations, you can use this scoot around.
Yes. This is truly one of the most rage inducing aspects of the job. I know we all have these stories — the one that always sticks with me was the time I was calling for a PA for a patient and had to give thei diagnosis. I said “schizoaffective disorder.” (I’m a psychiatrist). And the perky individual on the phone literally said, “Wow! I’ve never even heard of that!” And yet that is the person who gets to approve or deny the medication. I’m a pretty humble doctor, I know there’s plenty I don’t know, but that was just a slap in the face.
“Prior authorization = rationing by inconvenience.” Yup. I kept a stack of certified receipts at my desk, and I had a canned letter in which I would fill in the blanks of everyone I spoke with on the phone tree, advising that I would cooperate with or suggest initiating legal action against them. I sent certified letters to their legal staff. It often helped. What helped more was leaving medicine.
1. Only do PA’s during appointments since it is part of care.
2. Always tell clerks it’s nothing personal, but to be sure to tell superiors you are eager to attest that their delays may well cause bad outcomes and you’ll testify they must share liabilty and do not have a license to practice medicine.
3. Empatize with patients during delays.
I’m still laughing and just had to comment! Considering myself as a dinosaur-1) being one of the last to “put out your shingle” in private practice FP…surviving HMO/PPO BS early ’90’s, succumbed to emp.Dr. to deploy-then retiring twice… your insight and experience-although true to fact, in retrospect… I wish that I would have laughed more. Thank you! and keep up the good work-we Will persevere,as pts. are counting on that! Carry On!
Let’s talk business.
1. The physician is not the customer.
2. The patient is not the customer.
3. The employer is the customer.
So, why should the insurer worry if the patient doesn’t receive appropriate care and the physician is frustrated? They don’t.
I ask my patients to contact their benefits manager to let them know that they are paying a lot of money to an insurer that is providing a substandard product. They need to look at other providers.
This confirms to the patient that I am their advocate as is their employer. Sometimes, it actually works.
The problems with our health care system begin when the $$ are transplanted from the patient’s wallet and into the accounts receivable of the insurance company.
But why do we submit to this. Oh, because hospitals have the power to bankrupt us with a single admission. Interesting how the hospitals and insurance companies are symbiotic with each other, but parasitic to the patient.
We need a better alternative to hospital based care.
Think we can all relate! I felt like writing a similar op-Ed many times. As the process has been taking so long, I have even filed safety reports with my institution about medication delays that have led to significant disease worsening. I have many times wanted to bill insurance companies for the time and resources spent dealing with this because it only hurts them when it hits the wallet. Patients could rightfully sue the insurance company in some cases. It’s up to us to fix it for the next generation. Glad you put it out there! It’s infuriating
As the process has been taking so long, I have even filed safety reports with my institution about medication delays that have led to significant disease worsening. I have many times wanted to bill insurance companies for the time and resources spent dealing with this because it only hurts them when it hits the wallet. Patients could rightfully sue the insurance company in some cases. It’s up to us to fix it for the next generation. Glad you put it out there! It’s infuriating
Complete waste of time. In the end does any of this save money? . We are at healthcare costing 18 percent of the GDP despite all this anyway all the cost saving strategies aren’t curbing spending one bit.
I do believe Medicare For All is the best solution. Traditional Medicare requires almost no prior authorization, compared to private insurance. Medicare prescription coverage is currently private. That would change with Medicare For All. Isn’t it obvious by now that when profit enters the equation, profit making entities gain by interfering with physicians’ clinical judgment, potentially harming our patients?
While my idea won’t completely solve the problem at least it can keep me from losing my mind. I understand prior authorization for surgeries. I get paid for the procedure so it’s my job to get it approved by the insurance. I don’t love it but I can accept it.
Prior authorization for medications is an entirely different situation. I am spending money on extra staff to help the patient save money on a drug so that the drug company can make money. What’s wrong with this? The cost of prior authorization of medications should fall squarely on the patients shoulders. Until this is done, physicians will continue to shoulder the burden until it doesn’t make any financial sense to practice medicine. I want to start asking patients to pay for prior authorizations. If enough physicians did this, at least we won’t be used by insurance companies and drug companies so that they can make a profit.
I am a practicing, board certified internist.I encounter similar problems with the insurance companies. I not only end up spending the whole afternoon with these insurance companies but i end up doing it in my spare time dealing and arguing with these insurance agencies. I receive the similar response from people with no medical license making decisions like denying the doctors requests for approving the essential medications for their patients. They are indeed practicing medicine without license. There is no peer review mechanism with many of these insurance companies. The bottom line is medicine. Those people without medical license who deny the physicians legitimate requests for medications for their patients should be made legally accountable for trying to practice medicine without license and the insurance companies who employ such people without peer review options should be made equally countable legally by the federal authorities. That seems to be the only option and that will hopefully deter the insurance companies from resorting to such malpractice.
Why don’t we give these stories to news media and have them expose these rackets ?
So-I’m, a medical director, for a national health plan. And I’m going to be very straightforward:
1) No one, and I mean literally NO ONE on the medical side of the health plan likes the PBM, or anything about the PBM process. The issue , however, is not entirely down to the plans, or the PBMs. Pharmaceutical companies make pricing opaque to us (the plan) as well; we hire a PBM so we don’t have to hire a raft (and here I mean a bigger raft) of pharmacists to get the best prices from pharma companies. Unfortunately, while our contracts with PBMs say they will act as our fiduciary when dealing with pharma companies, no one is ever sure that they actually are, because *we can’t see into the pricing schema either*. It’s maddening for us as well; PBMs have become a necessary evil for insurers because we can’t individually negotiate with all the pharma companies and remain viable economically. (And unless you want to go back to being paid OOP for everything, you need insurers.
2) Not everyone makes treatment decisions as good as yours. Please believe me when I suggest that I’ve been told, by actual physicians, that the reason they want $EXPENSIVE_DRUG is because they no longer use $INEXPENSIVE_DRUG_THAT_WORKS_JUST FINE_FOR_MOST_PATIENTS, which is what most clinicians start with. When I ask why, with citations to literature, I get crickets. Fact is, I know why: $EXPENSIVE_DRUG is buy and bill, and they make a shiny profit on every transaction; $INEXPENSIVE_DRUG_THAT_WORKS_JUST FINE_FOR_MOST_PATIENTS is an oral drug that they can write a script for, which makes them no money at all.
Please, before you vilify the insurer, ask yourself “Why do they do this?”, and imagine that it’s not just to make themselves money – at the operational level (i.e. the money made or lost from actually receiving premiums and paying for health care) most health plans run anywhere from a 1-2% profit to a 1-2% loss every year – it fluctuates around the break even line; one year the plan I worked for made a big 4% profit, and we thought it was a banner year. Health insurance is not a big money business in that sense. Don’t believe me; read the annual report for J. Random Insurer. It’s all right there. I won’t say that saving money isn’t part of the goal – it is. But remember that not every physician is a complete altruist. (Neither am I, but I like to think I’m middling honest, and that means I have professional standards that require me to be able to back up my claims that what I want is the best for the patient with at least some science). But there are physicians that will practice in such a way as to maximize their profit, and tell themselves it’s because it’s better for patients when all it is is better for their wallet, while making it more expensive for everyone else. (Remember, all insurers do is take money from a lot of people, and then pay it to fewer people to provide services they need but otherwise could not afford). We both pay taxes and premiums, sir. Who do you think is watching out for taxpayers and the premium paying public? Me. That’s what I do. And when you ask qui custodiet ipsos custodes, I can answer that, too: Just about everyone. Health insurance is one of the most regulated industries in the US. The government audits us, the states audit us, independent outfits like the NCQA and URAC audit us…and we have to keep up with that while also doing our jobs, and for some of us, even from time to time taking care of patients.
So before you get all up on your high horse, realize that the rage goes both ways; those of us working the insurance side are really, really tired of everyone thinking all we care about is money. I didn’t practice emergency medicine (in a few nice places, and quite a few knife and gun clubs) for 25 years to be told by *anyone* that I don’t care about making sure patients get the best care. You do that retail and good for you; I do it wholesale nowadays, and believe me, I have done at least as much good doing what I do now as I did when I was in the ED making the crooked straight and the rough places plain.
I ask for a peer to peer and inform them that a physician not licensed in our state cannot overrule a physician in practice.
Many times I get a physician who is not, so I inform them of this and they sometimes give in. Either way, I they’ll them that I’m charging for the peer to peer as a consult conversation.
Sometimes get paid. A
But, bottom line is physicians are no longer respected nor believed. And insurance companies and drug companies are not interested in patient care.
My recent favorite prior auth request:
Order glucometer for diabetic patient > patient tells me 2 days later prior auth is needed > call pharmacy for more information > glucometer covered, but insurance company told pharmacy that NO TEST STRIPS are covered without a prior authorization > PA currently pending….
Patient can have a glucometer…just no way to use it beyond telling time I guess?
The last 10 years has seen a “pandemic” of prior authorizations for brand and generic medications. Two years ago I stopped doing prior authorizations except for rare situations. I am a family physician in Texas and take commercial insurance, medicare and medicaid. This is a problem across the board.
I am very up front with all reps that come to my office to pitch their drugs. I have told all of them I am willing to complete a prior auth but I need to be paid for my time or my employees time. I have yet to have any drug company step up to the plate. I have had suggestions that I can charge the patient. I have spent tens of thousands of dollars in my time and my staffs time filling out forms. I finally had to say enough is enough! I think it is time for all doctors to say ENOUGH IS ENOUGH! When did it become our duty and job to comply with prior authorizations?
The timeline of this phone tree is extraordinary..it goes EXACTLY the same way for me.
They give you a number to call for PEER to PEER which is the same number anyone from patient to medical assistant to RN call and then transfer you from person to person who all ask you the same questions (what doctor know the patients ID number?) only to connect you with a person who can’t help. It’s vile. Yes drugs are expensive but billions of dollars can go into the development of ONE drug (not always successful despite that) Tired of hearing about big bad pharma. Why are insurance companies (who are making huge profit) getting away with this?
In situations like this I demand to speak to a reviewer board certified in my specialty. At least ninety percent of the time they respond reasonably and the interests of my patients prevail.
For the other 10 percent I ask the recalcitrant physician reviewers if they are licensed to practice in my State. Florida has prosecuted out of state physician reviewers who have denied care. I get their names and I inform them that I will communicate actionable information to the patient and the patient’s attorneys. I ask them if their personal lawyers have reviewed any promises from their employers regarding indemnification and how confident they are that they are protected from criminal or civil liability. It doesn’t always work, but it makes them think.
Be aware that insurers find licensing is a cost of doing business in a state. I have 2 licenses which I have ‘legitimately’ (meaning: I have practiced medicine in those states, both for many years). I will soon have a raft of others, courtesy of my employer, who paid not just for the licenses, but for a company to obtain them.
The thing is, 80-90% of the requests are reasonable – but the explanations we receive for them are often either inadequate or missing. Once I get the data I need to make the right decision, it’s easy enough to do. And be honest: If we were asking for a ton of your money, would you just hand it over, or would you want to know we were keeping an eye on the store? How hard did you look at your health plan before you dropped that first premium? If you’re at all like me, you looked really, really hard. (Once, I was employed by a group that did not have a group plan – but did supply additional dollars for you to find an individual plan. My broker got the fourth degree (passing the third degree right on by) before I signed, believe it. This was before I worked for a health plan, mind, but I learned a lot of the lingo during that period).
It runs the other way, too, from time to time. More than a few times I’ve been asked to do a peer-to-peer, spoken with the doc, and been told some variation of “Yeah, you’re right; it’s not unreasonable to start with X; it’s just that the patient demanded Y, and I felt obligated to call”. And honestly, I don’t mind those calls. It’s not easy to tell the patient who absolutely knows what they need (even if you are less certain) “No”. Among other things, they may go see some other doctor. Instead, I serve as a convenient bad guy. Happy to do it. (I once reviewed a request for tretinoin cream for wrinkles – it’s cosmetic, and thus not covered. On it, someone (provider, staff, don’t know) had written “We know it’s not covered, please deny”. So I did, for the win. Company wins (did not pay for unnecessary medication); provider wins (did not have to deny the patient directly, maintains relationship with patient), and maybe the member wins (not exposed to unnecessary adverse effects for no really good reason – at least, no good therapeutic reason; if she really wants to be rid of the wrinkles, she can pay for the tretinoin out of pocket – it’s not like the provider wasn’t willing to prescribe it, after all (he already had; denial of coverage at the pharmacy counter is what triggered the request for authorization). DO you really feel that no one should keep an eye on that? We’re not the Doctor Police (I always have to spend a lot of training time with new MD/DO staff on that, because many would *love* to be the doctor police; this is why there are guidelines); we (like many people at a managed care organization) are stewards of the premium payer or taxpayer’s money. It’s our job to make sure you’re spending the money wisely and efficiently. it’s your job to show us you’re doing that. If we both do our jobs well, this can be relatively friction-free. Because so many doctors don’t feel obliged to work with the health plans, it’s more painful than it needs to be. This isn’t hard: explain it like you would to a reasonably bright colleague, who may not be in your specialty, but who can read just fine, and (if she’s been doing this a while, like many have) usually has looked at this kind of case before. Explain why either 1) the science we’ve used to create our guidelines doesn’t apply to your patient, because $REASONS, or 2) why the guidelines are not current (we work hard to keep them current, usually (and this is required by many auditing organizations) by working with people who are in your specialty to craft guidelines that are up to date and reasonably valid). Or 3) Your patient is, for some reason, a special snowflake, either temporarily or permanently. For commercial insurance, I can almost always say “You know what, let’s do it your way for 3 months/6 months/reasonable trial period of your choice. If it works, you tell me so in the next request. If it doesn’t, I don’t get a next request”. Unfortunately, Medicare and Medicaid don’t allow me to do that (authorizations must issue for a plan year, i.e. from when they were issued to whenever the plan renewal date is), so I have less leeway.
I’ve already gone on and on; part of what I;m getting at, though, is that the entire busted-a** system is so complex, with so many moving parts and competing agents, that it’s hard to figure out how to make things happen. One of the reasons I like single payer healthcare is that it would inevitably streamline that at least some. I hear everyone saying it would kill choice, make more bureaucracy and so on, and I think “How can any government system create MORE bureaucracy than ALREADY EXISTS NOW?” I don’t think it can be done; I think government involvement, for a change, would actually reduce the complexity of the (so-called) health care “system”. It’s worth a try, because the one thing we can both agree on, I suspect, is the the current system vacuums. (Think about what vacuums do and you’ll understand the concept I’m getting at).
M Lacy. Why change the narrative to your dislike for Medicare for all. This is not an either-or situation. Prior authorization does not have to exist whatever system we embrace.
I have a better story. A couple years ago, we found a pancreatic mass “with metastatic disease”. My order for PET CT was denies, even though she had a BS PPO. I end up a peer- to- peer with an internist who tells me he would not approve it as the “patient will not survive anyway and this study would not alter treatment cours.”
I should have followed thought with my treat to report this idiot to the board to have his license revoked. I did however tell him to call his medical insurance and demand a refund as they did not teach him the most important aspect to being a doctor, compasion!
As a medical director who has done a bunch of these types of reviews, I’m with you on this one. He may or may not be right about her chances of survival (they look pretty bleak to me, without having done any research yet or knowing any of the details) – but that’s not his call. The PET scan was indicated, and likely met the criteria they were using; that reviewer was letting his own feelings interfere, and trying to be the Doctor Police (which we’re not permitted to do, and which, when I’m training new MD/DO reviewers, I spend a lot of time cautioning them not to do).
The picture of how you felt dealing with the PBM describes exactly how I felt this past week trying to refill Lantus insulin for a patient who had been on it for awhile. Even though it was on our state’s Medicaid current Preferred list, it was denied and required a PA. Since generic insulin glargine (or Semglee) was also preferred, I turned around and ordered this only for it to be denied. After 3 calls like noted above, I finally reached someone who told me that “Yes, those insulins are on the preferred list, but they still need a PA (even though their denial letters noted these were preferred and a PA was NOT required!.” I finally found out that the ONLY long-acting insulin that would be approved without a PA was Levemir, which is not exactly the same as Lantus. But who cares!
I am laughing and crying while reading the conversation for prior authorization. I have been there more times than I can believe and like you I go to the end to help my patients. I really try to be respectful and civil with the reviewers but sometimes I just can’t. The last time I just said. “Why do you even exist in this job, a monkey could do what you do because you tell me you are bound by protocol so absolutely nothing I say will make any change in the outcome”.
Used to be that 10-20% of one’s patients took up 80-90%% of one’s time/energy…this has changed. I’m not sure how it falls out currrently, but that puzzling/troublesone 10-20% no longer gets that chunk of time (and effort), nor do all the other folks needing care, whether straight-forward or very complex
The insurers and others on.the business side of medicine get a disproportionate share of time,that could be spent with real patients and thier care.
It is very disheartening to see that profit-driven business interests require as much of our time and reources as they currently do.Do we have ANY leverage in this situation, to answer back effectively?
My personal favorite was when my patient needed 60 pills for 30 days:
Me: I am requesting 2 pills per day of (generic medication[sic]).
Them: Why not one pill?
Me: BECAUSE MY PATIENT REQUIRES 40 MG PER DAY AND THE PILL ONLY COMES IN 5 MG, 10 MG, AND 20 MG DOSES!
I wonder if physicians in countries where health care is socialized have similar problems?
I am in a rage!!!
When I really needed to get a PA approved back when I worked with insured patients, I found that if I called at 4:15 on Friday, my odds were better. They didn’t want to get into a tedious conversation. If the HS graduate on the other end of the line DID give me a hard time, I requested their medical license number. When they stammered about that, I would reply that “I DO have a medical license and I am telling you that the patient needs this drug for this reason. Unless you know better than me about this, I need an immediate approval.” That generally did the trick. But only works if you can get to a real person.