An ongoing dialogue on HIV/AIDS, infectious diseases,
January 2nd, 2019
How Did Our Medical Notes Become So Useless?
Among the many complaints about electronic medical records (EMRs), the death of the useful medical note ranks very high.
Notes are too long, too complex, and filled with unhelpful words. It’s often impossible to glean what the clinician thinks is going on, or what’s planned.
Ever get a note from an urgent care clinic on a patient who went there with a viral syndrome? Or a discharge summary? The note contains pages of indecipherable gobbledygook, ICD10 codes, irrelevant review of systems, stock phrases — the medical words are there, but where is the content? Give a click on this note for a particularly egregious example (all identifying information removed). Then come on back here. I’ll wait.*
(*Good chance these notes are faxed to your office, then scanned into your EMR’s “media manager,” or whatever your EMR calls it. My wife, a primary care pediatrician, calls this part of the EMR “the place where information goes to die.” Yep.)
It hasn’t always been this way. I’ve worked with EMRs of various sorts for decades. One of them, designed for outpatient care, had two ways to file notes — the clinician either dictated a narrative (for complex cases) or, more often, wrote a brief handwritten note in a 3-line section that was immediately typed in by clerical staff.
Both types of notes were infinitely more useful than today’s behemoths. The long dictated notes told a logical story, the short ones highlighted only the most relevant information. Example of the latter:
New painful rash on back. PE: vesicles in T10 dermatome on L, otherwise neg. Dx zoster, Rx Valacylovir 1 gm TID for 7d. Discussed possible complications, reasons to return or call for f/u.
That’s it! Today, this would be unimaginable. In a paper published in the Annals of Internal Medicine, three experts in EMR optimization compared the length of notes in the USA vs other countries:
In other countries, [a note] tends to be far briefer, containing only essential clinical information; it omits much of the compliance and reimbursement documentation that commonly bloats the American clinical note. In fact, across this same EHR, clinical notes in the United States are nearly 4 times longer on average than those in other countries
So how did we get here? What caused the note to shift from being the primary means of communicating medical information to this gargantuan beast? Three primary reasons:
1. Money. Some might call this “billing” or “regulatory” or “compliance,” but let’s call it by its root source — money. Based on quirks of our strange American healthcare system, certain words or phrases or diagnoses yield higher reimbursement than others. This hierarchy has nothing to do with delivering good patient care or communicating with other clinicians.
It’s not just individual words — entire sections of notes owe their very existence to maximizing revenue from clinical services. Dr. Mark Reid, author of the entertaining Medical Axioms, complained last week about being forced to include certain words in his notes.
He received this painful response from a Cardiology fellow, who recently had his notes reviewed by a “Cardiology Coder”:
I got this message in my epic inbox. As a FIT, it was hard to look at this in any positive way. What can I do to help? pic.twitter.com/7oJ34DOUdF
— Ali A. Azeem (@aliahsanazeem) December 29, 2018
Not only did poor Dr. Azeem include a Review of Systems to satisfy the Insatiable Billing Monster, but someone reviewed his Review of Symptoms to ensure he used the correct words! Could there be a better example of what’s wrong with medical documentation than this anecdote?*
(*And could you imagine having that reviewer’s job? Shudder.)
2. Copy/paste. Some EMRs have a feature where you can highlight only the original — not the copied or imported — content of a note. If you do this, you instantly understand why “ID consulted, awaiting input” appears several days after you’ve done your consult and have been communicating regularly with the primary team. They’re not ignoring your beautiful consult, they just haven’t gone back to update the text.
Other symptoms of copy/paste madness are the gobs of laboratory and radiology data appearing in every note, copied from the actual reports and then pasted into the “Results” section, or imported via macros (see #3 below).
How bad is the copy/paste phenomenon in medical documentation? Researchers at UCSF reviewed the source of text from medical notes over an 8-month period, and their findings were not pretty:
We analyzed 23, 630 notes written by 460 clinicians. In a typical note, 18% of the text was manually entered; 46%, copied; and 36%, imported.
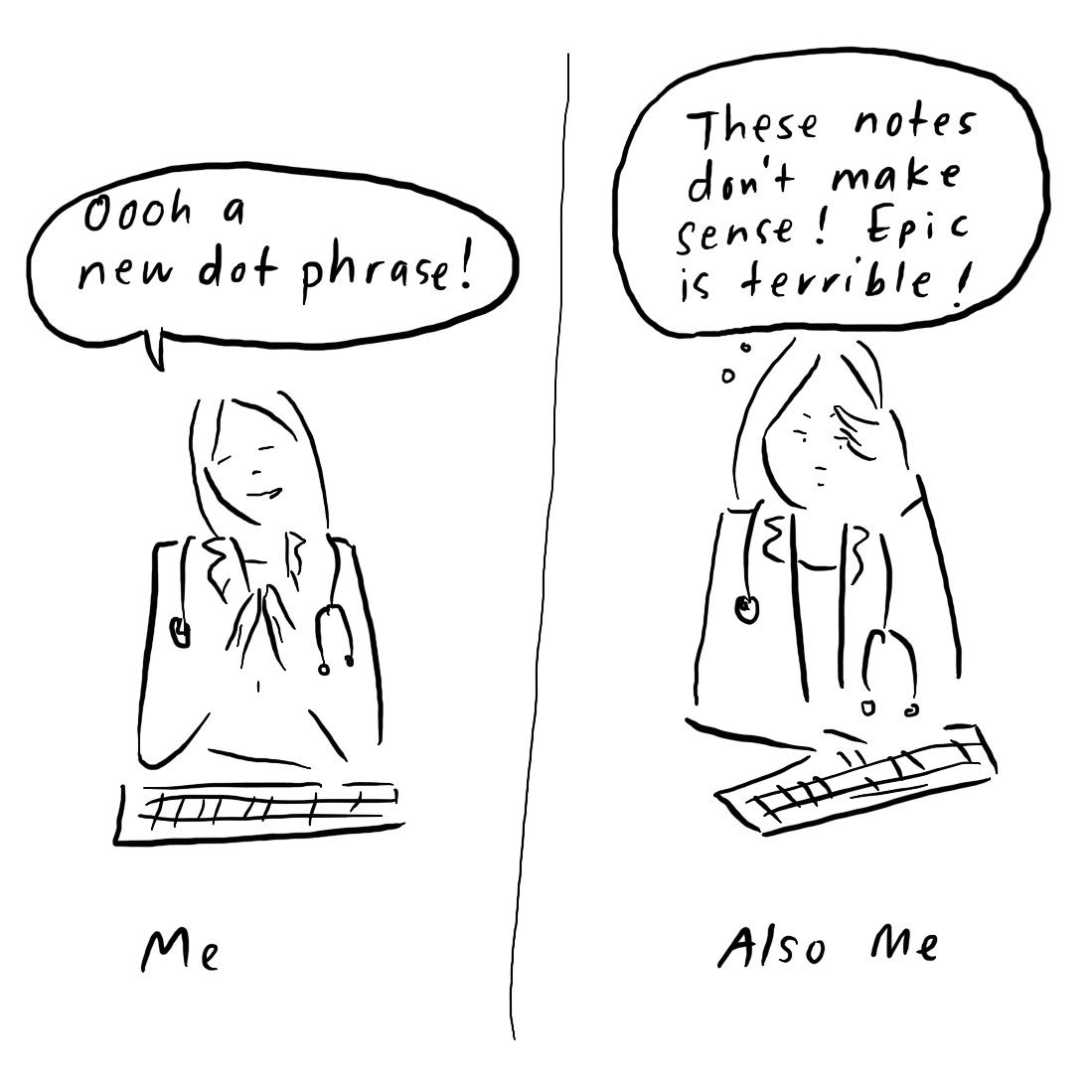
3. Text expanders. Call them what you like — “smart text” or “auto text” or “templates” or “dot phrases” — but these tricks of the trade, once mastered, are simply irresistible to most of us, for better or worse. Dr. Grace Farris captures our ambivalent relationship with this strategy perfectly in the cartoon that led off this post.
It works like this — we enter a magic little short string of characters, press return, and voila! Everything from a complex (but commonly used) sentence to a full medical note appears on the screen. Take a bow and admire your work!
From a Reddit thread on this strategy:
.NICU: As a peds resident, I made this dot phrase. Took me about 2 full days of work to get it together, but I basically created it to pull all the info I needed to preround on a patient. All the numbers from all systems, weight change, ecmo/ventilator settings, even the number of desaturations they had overnight. Approximately 6-8 pages worth of data, arranged in order of systems that we would present on rounds.
Impressive! But do we clinicians really learn, or interpret, material that “autopopulates” a note? And how can these one-size-fits-all notes apply to the infinite diversity of patient care?
Full disclosure: After once receiving feedback that my notes didn’t have sufficient documentation about the time spent on counseling and patient education, how did I respond? By creating “.saxcounsel”, of course — which when typed, expanded into a thorough description of time spent on counseling and patient education! That will show them!
So is there any hope for the medical note?
I do think there is a way to improve them, at least a bit, that won’t require a complete overhaul of billing regulations — but that will be a topic for a different post. In the meantime, I very much welcome your suggestions in the comments!


Dear Paul: You have left out Zuger’s law of inverse probabilities, namely: the more detailed and comprehensive is the note, the smaller are the chances that any of the listed details were actually elicited or that the described activities EVER took place, even in their first iteration.. I’m referring to all those normal reviews of systems, and those full physical exams including full neurologic evaluations with cranial nerves included.
There is no hope for us until the billers and coders are fired, and that will require a revolution. Up the revolution!
az
I loved the telegraphic notes and presentations of an intern colleague of mine in 1986 when we were doing it all longhand!. He was not fond of articles or fluff. It was completely understandable and went something like this:
58 male shoveling snow. Chest pain. Down. EMTs. Intubated. transported. ICU. (Vital signs and treatments given). Cath lab. 3VD. Ballooned (vessels). CCU. EF fraction. CPK max (predates troponin). 3 day stay, extubated (date). Floor. (vital signs and current meds). Complications: UTI. transient delirium. Near baseline. Smoking cessation, BP control, Weight loss, Rehab.
All ya need to know. I try to emulate to this day.
That seems to me to be a little TOO brief. Notes are meant to communicate (a) the patient’s course, (b) the diagnostic and treatment plan, and (c) the clinical reasoning. We must document WHY and BECAUSE (especially in the educational setting).
Just read a note from a Neuro Hospitalist regarding my patient who is obtunded and likely going to die in the near future – after he noted the poor prognosis he added a bullet point that he counseled the patient to follow up with his PCP (me)regarding his BMI of 33. This was one of those occasions that I hoped this was just billing fluff and he didn’t really have this discussion with my obtunded patient.
I could fill books with the useless notes I have received.
That’s both sad and outrageous at the same time.
Absolutely….
I’m sure I’m not the only internist who has done an eye-roll upon seeing “fundi without A/V nicking, arteriolar narrowing, exudates, hemorrhage, or papilledema” in an ORTHOPEDICS note.
seems to me that writing that you examined something when THERE IS NO WAY
such as the exhaustive comprehensive review of systems that I see in notes every day or an ocular exam by an orthopod is plain and simple FRAUD. I wonder when Medicare and then the privates will catch on and demand money be returned.
As a harried resident in the late 1970s, at the end of a long night on call in a busy NYC hospital I would often read the ER note, sub-intern note and intern note before having to add my own two cents. Fortunately there were no EMR compliance or bloated verbiage billing requirements. I simply wrote “As above , see below”. Unlike today’s cut and paste Joycean novellas, colleagues often read this note from beginning to end
This was some time back when I was in the Midwest where a prominent cardiovascular center existed that had excellent clinicians. Very soon it called loaded with care extenders who would complete notes before the attending physician finally signed and endorsed it. These notes were extensive nay exhausting. Once I was called to see a patient with overt hypothyroidism and as I was getting ready to enter the patient’s room (after reviewing the notes), I saw one of the pulmonologists leaving the room almost bursting into laughter. Once I saw the patient it became evident why my colleague was laughing. The admission notes stated “bilateral pedal edema with difficult to palpate distal pulses on both sides”. Trouble was that patient had had below knee amputation on left side years ago, and his prosthesis was by his bedside. I put down in my note that” the admitting service must have mastered the art of examining a phantom limb.”
Note from ED encounter with 9 m/o who presented with URI sx and fever included in ROS: no change in libido.
I think plaintiffs’ attorneys must be delighted when they see these fabulated elements in our notes. How easy to get a jury to question what other elements of the note are made-up?
I chastise my residents CONSTANTLY for copy-pasting. I type out all my meds, vitals, and labs daily, and I think I still don’t remember them as well as I did when I handwrote them on paper.
Agree with all the responders. Epic does make it easy to see what was cut / pasted versus actually entered…For most of my patients the ratio is 95:5. I am guilty of writing lengthy narrative-style attestations with pertinent history, exam, review of labs and assessment. I’m sure these are a biller’s nightmare but it’s the only way for me to actually go through a case in a logical way.
It’s a tiny modicum of satisfaction when colleagues thank me in person (or indirectly in their notes) for going through the data from scratch. It also helps justify recommending doxycycline over meropenem in a complicated MICU ID consult with fever of too many origins…(which worked by the way).
Thanks for this thoughtful blog. As much as people blame EHRs for issues, I think the amount of fluff that we have to now put into notes for QI, billing, etc has just gotten out of control. I know I’m going to sound like an old guy, but there was nothing better than a dictated note where you could tell the physician truly knew the patient
A few years ago I came across a pre-op note by a vascular surgeon that included an unusually detailed review of systems. A colleague reported overhearing the surgeon dictating a note in which he said, “Insert my usual review of systems”.
Although the nonsense in most EMRs is frequently amusing, it degrades patient care, and physicians who manufacture data are committing fraud. Write a free text note and billing be damned!
I think this note bloat for billing sake is probably the real reason that CMS wants to collapse the E/M billing categories of 2-4 into one level. Irrelevant ROS points and fraudulent counseling too easily make a simple-level 2-3 URI into a level 4 visit.
This madness will stop if/when we get to a national health program – like Canada’s – in which hospitals are globally budgeted (like a fire station), which will eliminate the need for billing entirely. Interested? visit the website of Physicians for a National Health Program.
I was a wanna-be immunologist, but I ended up detouring into the computer industry. As I read these wonderful comments, I think I made have made a prudent decision – for myself at least. As a patient I prefer simplicity. I feel sympathy for all of you as you are constrained more and more by government regulations and hospital policies that take you away from your original motivation to enter medicine: to help your patients. Continue the fight. I rather like the suggestion of “revolution.”
At least doctor’s handwriting is not the butt of jokes.
I remember inheriting a HIV+ young man from a pediatric clinic in another state. His viral load was suppressed on a complex and difficult regimen, so I requested old records to try to sort out his resistance. The records came surprisingly quickly, in five large boxes. On a slow day in clinic with many no shows, I decided to go through the records page by page, keeping only those pages with useful information. The clinical notes were mostly meaningless, though I did learn that at each and every visit, he was asked about his use of seatbelts, concerns about domestic violence, and his pastoral needs. I learned that his family history was reviewed at every visit but had never changed, perhaps because he was adopted. I learned about all the many symptoms that he consistently denied. I learned that every time his blood was drawn, it was from either the left or right antecubital fossa and that he “tolerated the procedure without complications.” I did find some CD4 counts and viral loads—almost the only pages that escaped the shredder. However, I did NOT find out anything about his resistance, since he had been suppressed for as long as the clinic had been using electronic records, they did not send the older paper records, and no one ever summarized his medical history or questioned his regimen.
The following is a typical example of a note when I began practice in the late 60s
ROM
Amox
Translation right otitis media
Rx Amoxil
With this minimalist writing I had plenty of time to discuss the family and the weather, actually do a history, I mean Hx, and perform a pretty good PERTINENT PE. I did not examine every fundus nor do rectals on 2 year olds with colds.
The pendulum swings
If we destroyed the “soap note” format and just had the 3 liner at the too and the billing “chart vomit” below, it would save a LOT of time. We have the option with our epic build to “hide copied text” and it greys out most of the note so you can find the updates hidden in the note.
I did a six-month locum in New Zealand. New Zealand has universal healthcare. The notes in the EHR system were always quite concise, there was no reason to add fluff to justify billing. Very useful addition was that the formulary was part of the EHR system . In being a universal healthcare country, everybody was on the same formulary.
This isn’t all private insurance co. related. In goverment health care this has gotten big particularly with medicaid billing.
I worked accounting for a mental health agency. They used to literally “chart” – and it was great. The chart was readable, you could page through, they would underline things to highlight them. They also filled out what we called a billing slip. It went into the billing side, with some coding (there were only 5 codes used so very easy). The contract had a capped total payment for the YEAR and plenty of extra service was delivered (this was a nonprofit with near infinite demand), and the org raised private donations to cover the rest. All in all a very efficient system.
Then one day we got a long lecture about compliance, including slides with folks in shackles and balls and chains who didn’t comply with things. A new electronic system would be implemented (Avatar), and yes, incredible amounts of absolute crap had to be documented in EVERY chart note. The saga went on from there (goverment ability to implement tech is WOEFUL), and for clinicians working in the field (90% of service was delivered to folks out of office) the work to get back, log into using this super cumbersome system, and chart was 100% ridiculous.
Because you could actually checklist these notes against a long list of criteria – site visits become less about patient outcomes, and more about checking lots of notes against long checklists for required elements and words.
The BS was so bad I left. As did many others. And I’m extremely tech savvy (younger generation) and love tech, but this stuff has gone off the rails. I now make much more (top 5% wage?) doing somewhat less rewarding work, but the thing that makes me happiest? NO MORE AVATAR!
Similar to Dr. Lake’s suggestion, some of our docs have addressed the utter uselessness of their notes by converting to the APSO format. Since no one wants to scroll through all the crap in their pasted, dot-phrased nonsense, they put the A/P at the top. Wrong solution to the problem, eh?
In the handwritten chart days, my notes were generally the longest ones in the chart, and now they are the shortest. They have not changed much, since I do not use dot phrases except for vital signs, meds, and my name and phone number. This makes me less efficient, but I think it is good for my patients.
A little more bad news: some of the data people (they are similar to Jawas, I think) would like to eliminate free text from notes, by making the entire note consist of discrete fields with words chosen from pull-down menus. If, heaven forbid, they ever succeed with this evil plot, notes will be totally harvestable for analysis, and totally useless for clinical care. (Try writing a text message using only the words suggested by your smartphone – that’s about how well it works.)
“Epic” is not a computer program, it is an entire culture. One of the key elements of that culture is the concept that as professionals we are now selling a “review of systems” for the money that comes from increased billing. This has multiple negative aspects. The monetization of our work encourages us to lie (for which we are rewarded). It also strips of our character as professionals who are motived by an honest concern for the well-being of our patients and whose practice is based on a specific scientific expertise.
Unfortunately, I don’t see an end to inefficient notes. One solution is to let machines sift through the fluff and help providers identify actionable information in real time. We, at http://www.diagnoss.com, have started to do this with medical coding. We’ve built a natural language processing engine that can make sense of the note enough to translate it into appropriate codes. It’s interesting to think that we’re now looking to machines to help as we reminisce over the short, handwritten notes of years ago that seemed to do the job.
I do agree that the current EMR system needs a lot of restructuring and Improvement, to find ways to cut out the fluff and better highlight the train of thought of clinicians. Writing a note to satisfy billing requirements is ludicrous, Unfortunately this was a significant part of my training as a resident.However the EMR is a positive step forward for medicine.I remember hand-written charts and medical notes where physicians would scribble four words together that no one could understand and bill medicare $800k per year. That was a joke. The EMR has a great potential and we need to continue to refine it.
Just wanted to point out this lengthy article on EMRs by Kaiser Health News. It more or less confirms everything we hate about the systems and points out how they can lead to errors: https://khn.org/news/death-by-a-thousand-clicks/